Abstract
Background
Cosmetic tourism is a global commodity, but patients seeking treatment for complications of international cosmetic tourism appear to be on the rise. We calculate the financial burden to a single NHS trust and summarise the literature, reviewing the implications of cosmetic tourism and summarising available guidance to assist surgeons in this ethically challenging, but expanding, field.
Methods
Hospital episodes for patients with complications from cosmetic tourism between January 2016 and March 2017 were retrieved using the patient management system. The coding department provided the episode costs. A literature search was conducted using Medline, EMBASE and HBE identifying 273 English abstracts. The abstracts were reviewed for relevance followed by assessment of the 48 selected full articles by all authors and 17 papers contained relevant, new information.
Results
Eleven patients underwent management for complications of cosmetic surgery, most commonly infection, with a sum of 29 inpatient episodes and total cost of £259,732.
Discussion
Our study illustrates the management of complications of cosmetic surgery carries a high cost. This is not an experience limited to just this trust in the UK. Internationally, healthcare systems are evolving to raise the safety profile for cosmetic tourists, some going the extra mile to accommodate healthcare tourists, reaping the financial reward.
Following the examination of the literature, we query whether NHS trusts should heighten their presence as providers of private services on the international market, eliminating numerous medical–ethic concerns associated with substandard cosmetic tourism.
Level of Evidence V
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cosmetic tourism is an established global commodity. Data captured by the International Society of Aesthetic and Plastic surgeons (ISAPS) in 2017 illustrates cosmetic surgery is a relentlessly expanding market [1]. More than 11 million cosmetic procedures were carried out, with a 1% rise in face and body procedures, 4% rise in breast procedures and a cumulative rise of 7% in body and extremity procedures [1]. The main contributors to the total number of operations were: the USA (18.4%), Brazil (10.4%) and Japan (7.2%). Cosmetic tourists most frequently visited Thailand (30.8%), Columbia (26%) and Mexico (23.4%), with breast augmentation, liposuction and blepharoplasty being the three most common procedures.
With rationalisation and funding shortfalls across the NHS for what were once common elective plastic surgery procedures, the number of patients seeking treatment for complications of privately funded, international cosmetic tourism appears to be on the rise. Tourists follow the path of least financial resistance, directly to the National Health Service, for ‘free’ emergency treatment. In this retrospective study and literature search, we calculate the financial burden of cosmetic tourism on our department, explore the patient factors and review the implications of cosmetic tourism, summarising available guidance to assist surgeons in this ethically challenging, but expanding field.
Methods
The plastic surgery department inpatient lists were reviewed to identify patients admitted with a complication from a privately funded cosmetic procedure between January 2016 and March 2017. Both British and foreign tourists undergoing international and domestic (UK) procedures were included. The dates of all hospital episodes, inpatient and outpatient department (OPD), were retrieved using the hospital patient management system. The coding department provided the cost of each episode based on the management, the codes used in theatre and on discharge summaries and clinic episodes.
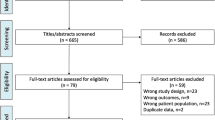
A literature search was conducted using Medline, EMBASE and HBE (Fig. 1). In total, 273 English abstracts were identified and 13 duplicates removed. The abstracts were reviewed for relevance followed by assessment of the 48 selected full articles by all authors and 17 papers contained relevant, new information.
Results
Eleven patients underwent management for complications of their private cosmetic surgery under the care of the Plastic Surgery Department at Chelsea and Westminster Hospital between January 2016 and March 2017 (Table 1). The most common surgery was a body contouring procedure to the abdomen (Table 2). The primary procedure was most commonly performed within the UK (Fig. 2), and the most common complication was infection (Table 1).
Two patients had ongoing management during the time frame of this study, but their management commenced in 2012 (Table 2, patient 7) and 2013 (Table 2, patient 2). One patient transferred to the private services within the trust after four days during their admission (Table 2, patient 11).
The average inpatient stay was nine days for medical management, surgical intervention or a combination of both. Three patients required critical care admissions: two intensive care unit (ICU) and one high-dependency unit (HDU) (Table 2: patients 3, 4 and 7). Across ten patients, there was an average of three operations and five dressing clinic appointments. A mean of two consultant-led outpatient appointments per patient were required (Table 3).
Eleven patients had a sum of 29 inpatient episodes (Table 4). The total cost for inpatient management amounted to £247,982, £259,732 with the inclusion of outpatient clinics. The three most expensive patient episodes based on management (Tables 2 and 4) were from patients 3, 4 and 7: £33,991, £99,261 and £53,637, respectively. Patient 3’s primary cosmetic procedure was in the Dominican Republic, whilst patient 4’s and patient 7’s procedures took place in Turkey.
The literature search identified 17 relevant papers published between 2010 and 2019 on trends in cosmetic and medical tourism (Table 5). These papers explore the impact of this industry on an international stage.
Discussion
Patient Incentives
The motivating factors behind medical tourism extend beyond healthcare needs and have been described in a hierarchical order [2]. This ranges from fulfilling ‘basic’ healthcare requirements such as immunisation, to patients seeking to optimise physical and mental well-being. Cosmetic surgery can be placed towards the top of this hierarchy.
Driving forces facilitating interest in cosmetic tourism include anonymity, shorter waiting lists, consumerism, patient dictated operations, less stringent regulation, new innovations unlicensed for use in the home nation and, most commonly, cost savings [3,4,5]. Klein et al. describe it as patients seeking ‘First-World service at Third-World cost’ [3], the cost being one part of the value perceived by patients. Harvard university strategist Michael Porter surmised that the patient perceived value is equal to the patient-relevant outcomes at a particular price [6]:
Consequently, the patient seeks a lower cost and perceives an increase in value. Outcomes, however, are patient-specific and influenced by factors including patient co-morbidities, the ability and experience of the surgeon performing the procedure, compliance with post-operative instructions, the occurrence of complications and appropriate management in a timely fashion. Following the PIP scandal of 2013, Sir Bruce Keogh highlighted the lack of robust regulation within the cosmetic industry, highlighting the potential for a lack of accountability, further adding to the variability in outcomes for cosmetic tourists [7].
Alizideh identifies patient education as fundamental in bridging the gap between patient expectations and the actual patient outcome [8]. The importance of this patient education is reflected by the efforts of representative organisations such as British Association of Plastic Surgeons (BAPRAS), the British Association of Aesthetic Plastic Surgeons (BAAPS) and the American Society Of Plastic Surgeons (ASPS), with their persistent and very public efforts [9,10,11].
Cosmetic Surgery as a Commodity
The conversion of surgery into a commodity has allowed interference from market forces in the patient’s decision-making process. This is reflected by the established association between particular countries and particular procedures: South America for aesthetic surgery, Hungary and Poland for dental treatments and countries such as Switzerland, Belgium and Canada attracting wealthier clients because of their attention to delivering patient preference with modern technology [1, 12].
The UK itself is a net exporter of medical tourists [13]. This net emigration is reinforced by the widespread availability of low-cost airlines and the increasing prominence of ‘packages’ offering a cost-effective flight and surgery all-in-one deal [14]. The financial lure, however, commits the patient early into undertaking what are entirely elective procedures, straddling an ethically fine line for cosmetic surgery providers [15].
A lack of access to the provider in the post-operative period is also significant concern, often arising due to geographic distance between the tourist and the initial provider. Sir Keogh’s report emphasised that providers have a duty to ensure suitable post-operative management, for an appropriate amount of time, with the patients having an avenue for recourse regardless of geographic location [7]. This study identified a cost of £259,732, an average of £23,612 per patient, across eleven patients, between January 2016 and March 2017, to a single trust for managing complications of private aesthetic surgery. Despite 37% of patients in this study having their private cosmetic procedure in the UK, all patients presented to the National Health Service for immediate, definitive and continued management of their complication, accruing costs that were not reimbursed by the private provider or the patient.
Emergency Management in the NHS
The eleven patients included in this study were solely managed by the Plastic Surgery Department at Chelsea and Westminster Hospital. This is a narrow reflection of the true extent and a likely under-representation of complications arising from breast surgery, for which there are a number of reasons.
The distribution of plastic surgery units across London means that there are two other large plastic surgery units in South London and a further three units in North, East and West London. This Pan-London network of plastic surgery units, a number of which with an established sub-specialty service in breast, creates an uneven pattern of referrals from primary care, secondary care and as decided by patients through their presentation to emergency departments.
Within the NHS, breast surgery is also an established sub-specialty of general surgery. It is a commonly encountered and accessible service within numerous district general hospitals, by comparison with the often tertiary centre located care delivered by plastic surgery units in the UK. We hypothesise that this furthers divides patients with complications from cosmetic breast surgery leading to their under-representation by a single unit.
Thirdly, although the NHS is a free point of emergency care for all individuals, when implants require removal in the case of emergency such as frank infection, the National Health Service’s position is not to offer replacement [14]. For patients who have undergone augmentation, this may offer enough concern for patients to pursue private management from the outset of any complication.
NHS Trusts As Providers Of Private Services
Previous studies have shown the UK to be a net exporter of patients for medical tourism [13]. This is reflected in our study with 54% of patients having their cosmetic surgery performed outside of the UK (Fig. 2). Hospitals within the UK do derive some benefit from medical tourists financially, with one tertiary care trust having estimated earnings of £20 million across 650 patients from international locations. In these centres with readily accessible private services, healthcare tourism will contribute a significant proportion of private patient generated revenue. We raise the question: Should more NHS trusts be proactive in offering private services?
Hospitals in Southeast Asia proactively cater to healthcare tourists within their healthcare model to actively attract these patients. In this model, medical tourism is a state-led business generating a revenue of $7.5 billion US dollars from 2004 to 2008, which has led to the formation of a centre of excellent health care of Asia initiative, focused on attracting this international patient cohort [16]. Whilst competitive pricing is a common attraction for many tourists, there are a proportion of patients travelling to well-industrialised countries to attain high-quality care at a premium price [1, 12, 13]. NHS trusts in the UK fall into this category and engaging medical tourist would relay both local and national benefits.
Revenue generated may reduce reliance on government funding for day-to-day maintenance matters and allow greater funding for matters concerning national modernisation of outdated NHS hospital buildings and historic NHS digital platforms, enabling systems to be more efficient and communicate on a local and national level [17, 18].
Local benefits include increased investment into operative and clinical spaces, in addition to the employment of a much-needed larger workforce with enhanced pay scales. Optimising working conditions would improve retention and reduce reliance on agency staff and the associated expenditure [18]. Heightened operative capability would enable reduced elective waiting times which has historically attracted fines in the remit of £300 for every patient not operated on within 18 weeks [19].
Brightman et al. [20] found 83.9% of 368 American plastic surgeons reported their patients had complications from procedures performed by non-plastic surgeons, with infection the most common complication. Although 35 of 45 surveyed medical tourism companies required provider or hospital accreditation, this was not to a uniform standard and only 19 companies had a role in coordinating follow-up. Our local study demonstrated that the most expensive patients to manage were those who had their cosmetic surgery abroad, requiring admission to critical care and management amounting to £186,889 across only three patients whose presenting complication was related to infection.
Specific benefits to UK nationals undergoing private surgery within NHS trusts include reduction in risks from medium- to long-haul travel post-surgery, more accessible follow-up, opportunity for more timely management of both emergency and non-urgent complications and where infection arises, reduced exposure to and co-transport of foreign pathogens, allowing for greater efficacy of our local microbiology-led empirical antibiotic choices [21]. Increased awareness and availability of private services within NHS trusts would provide an attractive alternative for cosmetic tourists, offering solutions to many of the peri-operative clinical and ethical concerns which compromise patient safety and increase morbidity.
Medical And Ethical Guidelines Within The Cosmetic Tourist Industry
For a patient to make an informed decision, there needs to be a consultation with the provider prior to any financial commitment, followed by a cool-off period [15]. Pareira et al. [22] identified that prior to having surgery abroad, patient counselling may only be by a non-medically trained representative. Following their review of the literature on the issues affecting cosmetic tourists, they put together a series of travel health recommendations, for cosmetic tourists, at three distinct phases: the pre-travel consultation, during travel and at the time of return. These recommendations provide the patient with a safe framework of considerations peri-operatively, aiming to reduce the morbidity associated with cosmetic tourism and allow for future complications to be dealt with locally in a safe environment.
Lorio et al. [23] summarise recommendations by representative bodies in the USA into a guidance for providers of cosmetic surgery. This includes the recommended content of the pre-operative consultation, provisions for post-operative care, including a named service provider for continued local follow-up for patients out of region and a commitment to reporting complications. These recommendations are in harmony with the recommendations by Pereira et al. which are from the patient perspective and is information which we advocate for patients to be informed of and coordinated in partnership with their surgeon [22, 23].
Although the responsibilities of the provider are evident and there is increasing emphasis on patient awareness pre-operatively, there is limited acknowledgment of the responsibilities of the domestic plastic surgeon in managing the complications of a cosmetic tourist. Within the NHS, the Department Of Health’s recommendation is that emergency treatment should be provided, but no revision or elective treatment should be undertaken for patients who have undergone private cosmetic surgery elsewhere [14]. From the patient perspective, what access do they have to recourse and should the NHS be remunerated by the private provider or insurance?
In private healthcare systems, there is potential for reimbursement by insurance companies for out of country medical treatments such as cardiac valve procedures. The funding by insurers, however, is only for reconstructive procedures that would be required due to complications, let alone funding elective cosmetic procedures. From a surgeon’s perspective, it may be less feasible to take on the care of these patients secondarily, due to lack of access to information pertaining to the primary procedure and the consumption of resources without equivocal reimbursement. Further management of the complications of cosmetic tourist privately will be even less desirable due to the escalating threat of litigation in an already unsatisfied patient [23]. Whether the complications of cosmetic tourism are managed privately or on a ‘free’ health service, the higher risk when the primary procedure is performed in developing countries, is becoming a matter of public health concern [24]. As revision procedures are entirely elective, for the revising surgeon, the decision to perform subsequent procedures should be based on the same parameters as any patient, in keeping with the surgical guidelines, recommendations from governing bodies and ethical principles.
Reform In The Cosmetic Tourist Industry
This study does not investigate the qualifications of the cosmetic tourist’s primary surgeon, but the rise in ‘high-street’ cosmetic procedures by the non-medically or surgically trained is well documented [25]. Where complications of cosmetic tourism are encountered, where feasible, we recommend the cosmetic practitioners are informed by the patient and their details documented at the least. This information will allow for trends to be noted and relationships identified, with the potential for this information to be used to inform management locally, regionally or nationally as a public health concern where significant.
Within the qualified surgical and medical profession exists a range of allied and sub-specialties of plastic surgery with names that undoubtedly would cause confusion amongst the non-surgically trained. Examples include oculoplastics, facial plastic surgeons and aesthetic medical practitioners, all of which will have a range of surgical and medical training, but nomenclature potentially leaves scope for generalisation of their skill set by a member of the public. In the ethically ambiguous service provider, this could be used to attract tourists for procedures out of the scope of the practitioners’ routine practice.
Within the UK, the Royal College of Surgeons, BAPRAS and BAAPS have consciously produced information for patients on the expected standards of care when pursuing cosmetic surgery, home or abroad. These organisations have facilitated formation of the Cosmetic Surgery Inter-specialty Committee (CSIC) and its certification scheme and the Joint Committee for Cosmetic Practitioners (JCCP), which provides the public with a means to verify their cosmetic practitioners training, qualifications and experience. These changes aim to provide a more ethically balanced framework within an industry that has existed unregulated, optimising patient safety through transparency.
To drive the necessary reform, change at a government level is needed. These changes may seek to mirror those established in France with the enactment of the Kouchner law 2002, providing comprehensive safeguards such as advertising regulation, in addition to the established role for criminal law in a patient’s desire to pursue recourse [26].
Conclusion
Our study illustrates the management of complications of cosmetic surgery carry a high cost. This is not an experience limited to just this trust in the UK [27]. Internationally, healthcare systems that have evolved to accommodate healthcare tourists, however, are reaping the financial reward.
There is still a need to raise the patient safety profile for cosmetic tourism, and solutions include a database for reporting complications to facilitate development of healthcare strategies and the subscription to the ‘Global Partner’ agreement amongst international plastic surgery societies that commit to maintaining a high standard in plastic surgery [27, 28]. Nevertheless, significant milestones have already been reached in the UK since the absence of a regulatory framework was officially highlighted in 2013 [7].
As the cosmetic tourist industry continues to strive for higher global standards, we query whether NHS trusts, with their certified surgeons and physicians, established standards of care, regulation and governance, should seek to heighten their presence as providers of private healthcare services on the international market. The proactive provision of these services would be a means of generating further income for financially strapped NHS trusts and potentially eliminate a number of the clinical and ethical concerns associated with international substandard healthcare and cosmetic tourism.
References
ISAPS (2018) ISAPS international survey on aesthetic/cosmetic procedures performed in 2017. Available: https://www.isaps.org/medical-professionals/isaps-global-statistics/. Accessed 17 Sep 2019
Runnels V, Carrera PM (2012) Why do patients engage in medical tourism. Maturitas 73:300–304
Klein HJ, Simic D, Fuchs N, Schweizer R, Mehra T, Giovanoli P, Plock JA (2017) Complications after cosmetic tourism. Aesthet Surg J 37(4):474–482
Chen LH, Wilson ME (2013) The globalization of healthcare: implications of medical tourism for the infectious disease clinician. Clical Infect Dis 57(12):1752–1759
Miyagi K, Auberson D, Patel AJ, Malata CM (2012) The unwritten price of cosmetic tourism: an observational study and cost analysis. J Plast Reconstr Aesthet Surg 65(1):22–28
Porter ME (2010) What is value in health care? N Engl J Med 363(26):2477–2481
The Department Of Health and Social Care (2013) Review of the regulation of cosmetic interventions. Available: https://www.gov.uk/government/publications/review-of-the-regulation-of-cosmetic-interventions. Accessed 17 Sep 2019
Alizadeh K (2017) Commentary on: complications after cosmetic surgery tourism. Aesthet Surg J 37(4):694–697
British Association Of Plastic, Reconstructive and Aesthetic Surgeons. Considering Cosmetic Surgery? Available: https://www.bapras.org.uk/public/patient-information/cosmetic-surgery/considering-cosmetic-surgery. Accessed 17 Sep 2019
British Association Of Aesthetic Plastic Surgeons (2010) Shocking new statistics fail to shock surgeons. Available: https://baaps.org.uk/media/press_releases/1332/shocking_new_statistics_fail_to_shock_surgeons. Accessed 17 Sep 2019
American Society Of Plastic Surgeons (2010) Briefing paper: cosmetic surgery tourism. Available: https://www.plasticsurgery.org/news/briefing-papers/briefing-paper-cosmetic-surgery-tourism. Accessed 17 Sep 2019
Hanefeld J, Horsefall D, Lunt N (2014) What do we know about medical tourism? a review of the literature with discussion of its implications for the UK National Health Service as an example of a public healthcare system. J Travel Med 21(6):410–417
Hanefeld J, Horsefall D, Lunt N, Smith R (2013) Medical tourism: a cost or benefit to the NHS? PLoS ONE 8(10):e70406
Jeevan R, Birch J, Armstrong AP (2011) Travelling abroad for aesthetic surgery: informing healthcare practitioners and providers while improving patient safety. JPRAS. 64:143–147
General Medical Council. Explaining risks and seeking informed consent. Available: https://www.gmc-uk.org/ethical-guidance/learning-materials/seeking-informed-consent. Accessed 17 Sep 2019
Noree T, Hanefeld J, Smith R (2016) Medical tourism in Thailand: a cross-sectional study. Bull World Health Organ 94:30–36
Iacobucci G (2019) PM’s £1.8bn pledge for NHS buildings is “drop in the ocean,” say experts. Available: https://www.bmj.com/content/366/bmj.l5031. Accessed 5 Nov 2019
NHS Digital. (2019). Modernising our delivery model. Available: https://digital.nhs.uk/about-nhs-digital/our-work/transforming-health-and-care-through-technology/fit-for-2020-report-from-the-nhs-digital-capability-review/modernising-our-delivery-model. Accessed 5 Nov 2019.
Robertson R, Wenzel L, Thompson J, Charles A (2017) Understanding NHS financial pressures How are they affecting patient care? Available: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/Understanding%20NHS%20financial%20pressures%20-%20full%20report.pdf. Accessed 5 Nov 2019
Brightman L, Ng S, Ahern S, Cooter R, Hopper I (2018) Cosmetic tourism for breast augmentation: a systematic review. ANZ J Surg 88(9):842–847
Adabi K, Stern CS, Weichman KE, Garfein ES, Pothula A, Draper L, Tepper OM (2017) Population health implications of medical tourism. Plast Reconstr Surg 140(1):66–74
Pereira RT, Malone CM, Flaherty GT (2018) Aesthetic journeys: a review of cosmetic surgery tourism. J Travel Med 25(1):tay042
Iorio ML, Verma K, Ashktorab S, Davison SP (2014) Medical tourism in plastic surgery: ethical guidelines and practice standards for perioperative care. Aesthet Plast Surg 38(3):602–607
Ross KM, Moscoso AV, Bayer LR, Rosselli-Risal L, Orgill DP (2018) Plastic surgery complications from medical tourism treated in a U.S. academic medical center. Plast Reconstr Surg 141(4):517e–523e
BAAPS (2019) Cosmetic surgery stats: number of surgeries remains stable amid calls for greater regulation of quick fix solutions . Available: https://baaps.org.uk/about/news/1708/cosmetic_surgery_stats_number_of_surgeries_remains_stable_amid_calls_for_greater_regulation_of_quick_fix_solutions. Accessed 5 Nov 2019
Griffiths D, Mullock A (2018) Cosmetic surgery: regulatory challenges in a global beauty market. Health Care Anal 26(3):220–234
Sadr AH, Pau A, Griffin MF, Butler PE, Mosahebi A (2019) The implications of cosmetic tourism on tertiary plastic surgery services; The need for a national reporting database. J Plast Reconstr Aesthet Surg 72(7):1219–1243
Campbell CA, Restrepo C, Navas G, Vergara I, Peluffo L (2019) Plastic surgery medical tourism in colombia: a review of 658 international patients and 1,796 cosmetic surgery procedures. Plast Reconstr Surg Glob Open 7(5):e2233
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial or commercial conflicts of interest. No funding was required.
Ethical Approval
As a retrospective review, ethical approval was not required.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Asher, C.M., Fleet, M., Jivraj, B. et al. Cosmetic Tourism: a Costly Filler Within the National Health Service Budget or a Missed Financial Opportunity? A Local Cost Analysis and Examination of the Literature. Aesth Plast Surg 44, 586–594 (2020). https://doi.org/10.1007/s00266-019-01571-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-019-01571-7