Abstract
Background
Nipple reconstruction is an important last step in the process of autologous or implant-based breast reconstruction. A multitude of techniques have been described, among others the S-flap. To prevent nipple retraction after surgery, we modified the originally described method by Cronin.
Methods
By adding an S-shaped incision line, the flap can be transposed with less tension and sutured on top of the new nipple along a curved line. Furthermore, two small triangular flaps were inserted at the base for reinforcement and reduced linear contraction. Assessment was completed by measuring nipple diameter and projection with a caliper.
Results
A total of 16 patients underwent the technique, of whom 11 could be followed after 3 and 6 months. Overall patient satisfaction with the aesthetic result was high, and we observed no infection or necrosis. Nipples were stable in size and shape at 6 months. Although reduction of 68% in projection and 31% in diameter was observed, the nipples remained pleasantly similar to the contralateral non-operated side.
Conclusions
The modified S-flap is a simple and reliable technique for moderate-sized nipple reconstruction. By providing more tissue at the base, size and projection remain stable and durable. Moreover, by a modified linear incision line at the base, tension and subsequent scar contraction is minimal.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The nipple represents an essential part of the breast and consequently of breast reconstruction following cancer surgery. Therefore, most patients consider nipple reconstruction as an important factor to regain corporal identity in their reconstructive process [1, 2].
Although several techniques have been described for nipple reconstruction [3], none seems to be entirely satisfactory and loss of projection over time remains a major issue [4, 5]. Depending on the reconstructive technique, decrease in projection between 50 and 70% has been described, with most of the shrinking occurring within the first year after reconstruction [6, 7]. To increase projection and volume, dermal and/or flap grafts, acellular cadaveric dermis (AlloDerm) and cartilage grafts can be implemented, with various degrees of success [8–10]. If designed properly, however, the flap method alone can achieve favorable results for the reconstruction of small-to-moderate-sized nipples, without the need for non-autologous material or additional donor sites. With this study, we propose a modification of the S-flap technique by providing more tissue and using a modified linear incision at the base.
Materials and Methods
A total of 16 patients after mastectomy due to breast cancer (range 25–48 years) were included in this study. Eleven patients underwent previous expansion and transfer of latissimus dorsi flap, three patients underwent direct soft tissue expansion on the chest, and two patients underwent a slow, continuous expansion with Becker adjustable implants after transfer of the latissimus dorsi flap. Between December 2005 and July 2011, nipple reconstruction with the modified S-flap technique and the second step of an implant-based secondary breast reconstruction was performed simultaneously. The median time interval between breast reconstruction and nipple reconstruction was 14.4 ± 3.3 months (range 10–21 months). Fifteen reconstructions were performed unilaterally, and one reconstruction was performed bilaterally. Written consent was obtained from all patients, and the guidelines of the Declaration of Helsinki were followed throughout the study.
Technique
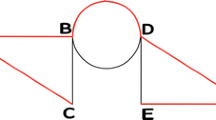
The flap is marked at a sitting or standing position, with arms attached to the body and both shoulders leveled. The point O is the center of the new nipple, which is determined by symmetry to the normal side in unilateral reconstruction, and by symmetry, shape and size in bilateral reconstruction. To support enough connective tissue, a circle is made around point O with a diameter of 40 mm.
The circle is split in half by a horizontal diameter between points E and E′. Another diameter oblique to the horizontal line by 60° joins the circle at points G and G′. On the horizontal diameter were points F and F′, both at 10 mm to point O. With the points E and E′ as centers, two 10-mm circles are drawn to cross the large circle at points H and H′. Then, two S-shaped curves are drawn to join points F and H and points F′ and H′.
Along the 40-mm circle around the “O” two sets of opposing flaps are outlined. With reference to the diagrams (Fig. 1), the area bordered by line EF′, curves GH′ and H′F′ represents flap a; the area bordered by line E′F, curves CD′ and B′D′ represents flap b; the area bordered by line AC and curve CD′ represents flap c; and the area bordered by line A′C′ and curve C′D represents flap d. For the larger flaps a and b the base is one-third of the 20-mm circle; for the smaller flaps c and d, the base is one-third of the 10-mm circle.
After flap elevation, the large flaps are joined and sutured to each other to form a cylindrical shape. In the distal ends, the flaps are interlocked to form an S-shaped suture line on the top. Then, the small flaps are inserted to the base for enhancement.
Surgical Procedure
With the patient sitting or standing upright, the position of the new nipple was marked according to the opposite side. After having measured the width and projection of the opposite nipple, the flaps were drawn as previously described to guarantee sufficient width. The cylinder was designed to have a maximum projection of 30 mm and was situated more laterally toward the armpit (Fig. 1). The procedure was performed in the outpatient clinic under local anesthesia. Limiting pedicle damage, anesthesia was injected subcutaneously by a 5-ml syringe at the lateral sides of the flaps. Also, to better assess blood supply to the flaps, once raised, 1% lidocaine solution without adrenaline was used.
The incisions were made with a No. 11 blade, starting from the border of flap a and finishing at flap c. The flaps were carefully dissected and elevated to gain adequate mobility while keeping a layer of subcutaneous fat, especially when approaching the pedicle (Fig. 2a, b).
After meticulous hemostasis was performed, the donor incisions from flaps a and b were closed first in a layered fashion, starting at the medial end on each side. Then, the large flaps were approximated to assess the size of the new nipple. If the nipple was too big or the tension inadequate, some of the excessive subcutaneous fat was removed. After trimming, the flaps were sutured together in a layered fashion, first along the vertical line, and then along the S-shaped curve line on the top, to complete the cylindrical shape. Then, the small flaps c and d were inserted to the base of the cylinder and met the cylinder along the two side lines (Fig. 2c, f).
At the end of the procedure, the surgical area was covered with 1% chloramphenicol ointment and non-adherent, doughnut-shaped dressings until one week after the surgery. After that, the patients were advised not to wear tight bras until 6 weeks after the surgery. Interrupted stitches with non-absorbable sutures were removed after 7 days. Photographs were taken, and the projection and diameter of the reconstructed nipple was measured by a caliper after 3 and 6 months.
Results
Eleven patients completed the 3- and 6-month follow-up. There were no infections or necrosis in the follow-up period, and all patients had a pleasant result. The nipples were stable in size and shape after 6 months with a satisfactory outcome up to 24 months (Figs. 3, 4, 5, 6, 7). On average, the retraction rate of nipple projection was 68.47 ± 2.68%, whereas the retraction rate in nipple diameter was 31.03 ± 2.57% (Table 1).
A 32-year-old female patient after modified radical mastectomy due to right breast cancer 3 years ago, and breast reconstruction with expander-based latissimus dorsi flap 4 months ago (a, b). She underwent the second step of an implant-based secondary breast reconstruction by anatomic silicone implants and simultaneous nipple reconstruction (c). The 6-month follow-up showed a good shape of both breast and nipple (d). Nipple projection was 8.5 mm, diameter was 9 mm, and retraction rate of projection and diameter were 68.5 and 30%, respectively
Discussion
The originally described S-flap method was proposed in 1988 by Cronin et al. [11], who elevated two dermal flaps vertically and sutured them together. The dermal column was then covered by a full-thickness skin graft. As reported by Lossing et al. [12] skin grafts on a dermal surfaced nipple have no long-lasting nipple projection. Due to this reason, we further evolved the technique from dermal flaps to full-thickness skin flaps.
Some authors suggest that the results of nipple reconstruction are associated with the underlying tissue and type of breast reconstruction [6], while most agree that the nipple projection is largely determined by flap thickness, vascularity and supportive tissue at the base.
A major complication of its reconstruction can be nipple necrosis, as a result of poor vascularization. To maintain robust blood supply, we carefully kept the width/length ratios high, more than 1:1 for smaller flaps and more than 1:2 for larger flaps. The broad pedicles provide a solid base for a robust and safe blood supply of the flaps. Furthermore, the back cuts along the curves DC′ and CD′ further reduce tension at the base to a minimum. Additional attention is paid to previous scarring. Ideally, the flap pedicles should not be located in the scar area; if unavoidable, the scar should lie at the distal end or border area of the flap.
Another challenge and common problem of nipple reconstruction has been loss of projection and volume over time, which is reported as high as 50–70% [13]. As suggested by some authors [14], we overcorrected the reconstructed nipple by nearly 300% in projection and about 150% in diameter, in order to warrant an aesthetically pleasing long-term result. Moreover, Rubino et al. [15] reported that nipple projection and volume can be improved by increasing the dermis-fat ratio within the flap. Thus, during elevation of the flaps, we avoided over-trimming the subcutaneous fat in order to preserve proper volume. On the other hand, we designed an S curve to reduce linear contraction and successfully avoided a concaved appearance on the top of the nipple. Likewise, we added a set of small flaps to refine donor-site closure, which resulted in reduced scar contraction and avoidance of dog-ears at the base.
In addition, the base may broaden with time, which progressively flattens the nipples. This is essentially caused by retraction forces of the surrounding and underlying tissues [16]. Thus, prerequisites for achieving a long-term projecting nipple do involve a flap with a wide pedicle and meticulous separation from potentially retracting surrounding tissues [3].
In a recent paper by Topol et al. [17] the use of a delayed technique in a two-stage nipple reconstruction enhances the underlying dermal circulation and hence improves flap viability and nipple projection. In our method, however, we use a one-stage technique with simultaneous expander-based breast and nipple reconstruction. It works like a delay technique, and over-expansion provides additional tissue for nipple reconstruction.
Some authors advocated the use of a silicone shield to reduce long-term flattening of the reconstructed nipple [18]. The rigid silicone structure is suggested to offer a valid support against pressure on the reconstructed nipple, reducing the absorption of the subcutaneous tissue. However, we did not use the silicone shield or any other rigid protective device, as it potentially may damage blood supply at the base due to the applied pressure.
All 11 patients were satisfied with the final result, as they generally perceived the breast as “complete” after nipple reconstruction. To measure durable projection, we performed caliper measurement. The measurement indicated that on average projection loss was 68.7% and diameter loss 31.03% within 6 months, which is comparable with previous reports in the literature [4]. We hypothesize that providing more tissue at the base with the two smaller flaps leads to stable and durable size and projection while limiting retraction forces and contraction of the flap.
A review of 600 breasts showed that the mean diameter of the areola is approximately 4 cm, the average nipple diameter is 1.3 cm, and the average nipple projection is 0.9 cm [19]. The average nipple–areola and areola–breast proportion is approximately 1.3 cm [20]. Zhong et al. [4] noticed an average loss of nipple projection of 75% at an average of 44 months following nipple reconstruction using the modified skate flap technique. In another study by Richter et al. [21] long-term projection of the reconstructed nipple was evaluated after using a modified skate flap, a quadrapod flap or a nipple sharing procedure. The authors noticed a mean decrease in projection for the nipple sharing method of 27.6 ± 18.2%, 45.0 ± 11.1% for the skate flap method and 49.9 ± 11.56% for the quadrapod flap. Similar results were reported for other techniques, such as 59% long-term projection loss for the modified star-dermal fat flap technique [7]. Cheng et al. [22] described maintaining nipple projection in Asian females with the use of a modified top-hat flap in combination with costal cartilage banked at the initial flap inset. After long-term follow-up of 58 patients, they found an average of 26.1% projection loss after 45 months.
A limitation of our study is the short-term follow-up, and therefore a further loss in nipple projection may occur over time. More prospective, large-scale and long-term case–control studies are needed to validate our findings.
Conclusions
Our modified S-flap technique is a safe and reliable method for moderate-sized nipple reconstruction. By providing more tissue at the base, size and projection remain stable and durable. Moreover, by using a modified linear incision line at the base, tension and subsequent scar contraction is minimal.
References
Buck DW 2nd, Shenaq D, Heyer K, Kato C, Kim JY (2010) Patient-subjective cosmetic outcomes following the varying stages of tissue expander breast reconstruction: the importance of completion. Breast 19:521–526
Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA (2000) Determinants of patient satisfaction in postmastectomy breast reconstruction. Plast Reconstr Surg 106:769–776
Farhadi J, Maksvytyte GK, Schaefer DJ, Pierer G, Scheufler O (2006) Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg 59:40–53
Zhong T, Antony A, Cordeiro P (2009) Surgical outcomes and nipple projection using the modified skate flap for nipple-areolar reconstruction in a series of 422 implant reconstructions. Ann Plast Surg 62:591–595
Hammond DC, Khuthaila D, Kim J (2007) The skate flap purse-string technique for nipple-areola complex reconstruction. Plast Reconstr Surg 120:399–406
Shestak KC, Gabriel A, Landecker A et al (2002) Assessment of long-term nipple projection: a comparison of three techniques. Plast Reconstr Surg 110:780–786
Few JW, Marcus JR, Casas LA, Aitken ME, Redding J (1999) Long-term predictable nipple projection following reconstruction. Plast Reconstr Surg 104:1321–1324
Guerra AB, Khoobehi K, Metzinger SE, Allen RJ (2003) New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg 50:31–37
Gullo P, Buccheri EM, Pozzi M, De Vita R (2011) Nipple reconstruction using a star flap enhanced by scar tissue: the Regina Elena Cancer Institute experience. Aesthet Plast Surg 35:731–737
Nahabedian MY (2005) Secondary nipple reconstruction using local flaps and AlloDerm. Plast Reconstr Surg 115:2056–2061
Cronin ED, Humphreys DH, Ruiz-Razura A (1988) Nipple reconstruction: the S flap. Plast Reconstr Surg 81:783–787
Lossing C, Brongo S, Holmstrom H (1998) Nipple reconstruction with a modified S-flap technique. Scand J Plast Reconstr Surg Hand Surg 32:275–279
Bodin F, Bruant-Rodier C, Lutz JC, Himy S, Wilk A (2008) Reconstruction of the nipple–areolar complex: long-term results. Ann Chir Plast Esthet 53:334–341
Bernard RW, Beran SJ (2003) Autologous fat graft in nipple reconstruction. Plast Reconstr Surg 112:964–968
Rubino C, Dessy LA, Posadinu A (2003) A modified technique for nipple reconstruction: the ‘arrow flap’. Br J Plast Surg 56:247–251
Nimboriboonporn A, Chuthapisith S (2014) Nipple–areola complex reconstruction. Gland Surg 3:35–42
Topol BM, Campbell CJ, Dalton EF, Ponn TA (2010) Nipple reconstruction on implant-only breast mounds: the use of a delay. Plast Reconstr Surg 125:15e–16e
Salgarello M, Cervelli D, Barone-Adesi L (2008) The use of a silicone nipple shield as protective device in nipple reconstruction. J Plast Reconstr Aesthet Surg 61:1396–1398
Sanuki J, Fukuma E, Uchida Y (2009) Morphologic study of nipple–areola complex in 600 breasts. Aesthet Plast Surg 33:295–297
Hauben DJ, Adler N, Silfen R, Regev D (2003) Breast–areola–nipple proportion. Ann Plast Surg 50:510–513
Richter DF, Reichenberger MA, Faymonville C (2004) Comparison of the nipple projection after reconstruction with three different methods. Handchir Mikrochir Plast Chir 36:374–378
Cheng MH, Ho-Asjoe M, Wei FC, Chuang DC (2003) Nipple reconstruction in Asian females using banked cartilage graft and modified top hat flap. Br J Plast Surg 56:692–694
Acknowledgements
We thank Nicola Keller for his contributions to the preparation of the figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Shaoqing Feng and Bo Zhang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Feng, S., Zhang, B., Kappos, E.A. et al. Modified S-Flap for Nipple Reconstruction. Aesth Plast Surg 41, 312–317 (2017). https://doi.org/10.1007/s00266-017-0789-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-017-0789-z