Abstract
Background
Several different methods have been proposed for treatment of gynecomastia, depending on the amount of breast enlargement and skin redundancy. The liposuction pull-through technique has been proposed as an efficacious treatment for many gynecomastia cases. This work aims to study the outcome of this technique when applied as an outpatient procedure, without the use of drains and through a single incision.
Methods
Fifty-two patients with bilateral gynecomastia without significant skin excess were included in this study. The liposuction pull-through technique was performed through a single incision just above the inframammary fold and without the use of drains. Patients were followed up for 6 months.
Results
The proposed technique was able to treat the gynecomastia in all patients, with a revision rate of 1.9% to remove residual glandular tissues. There were no seromas, hematomas, nipple distortion, permanent affection of nipple sensation or wound healing problems.
Conclusion
The liposuction pull-through technique is an effective treatment for gynecomastia without significant skin redundancy. It combines the benefits of the direct excision of glandular tissues, with the minimally invasive nature of liposuction. Performing the procedure through a single incision without the use of drains and without general anesthesia is a safe alternative.
Level of evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors http://www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There have been many different surgical approaches described for the treatment of gynecomastia, including liposuction, direct excision and excision with skin reduction and nipple reposition. The main goal in surgical treatment is to achieve a pleasant male breast and chest wall shape with acceptable or concealed scars, removal of the glandular tissues, avoidance of skin irregularities, preservation of nipple and areola sensation and avoidance of other complications [1]. Cosmetic complaints after gynecomastia excision are not uncommon, and include visible scars, nipple distortion or malposition, under resection, asymmetry and a “dished out” appearance. In addition, postoperative hematoma and seromas are also seen due to the large dead space often left after an open excision.
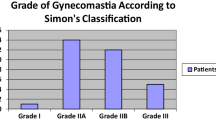
Simon’s classification [2] is a commonly used classification for gynecomastia that can help determine the surgical technique. The classification includes: Type I—Minor breast enlargement/No skin redundancy, Type IIa—Moderate breast enlargement/No skin redundancy, Type IIb—Moderate breast enlargement/minor skin redundancy and Type III—Gross breast enlargement with skin redundancy resembling a female breast suffering from ptosis.
The ideal surgical approach should include short and hidden scars, have a low rate of cosmetic complications and allow removal of both the fatty and the glandular tissues. The liposuction pull-through technique for gynecomastia treatment offers many advantages for treatment of Grade I and II gynecomastia, and allows a complete excision of the glandular tissues, a relatively faster recovery and facilitates intraoperative shaping and contouring. Several authors have shown good results with the use of this technique [3]. We have been using this technique for gynecomastia without skin redundancy, and modified the technique by using a single scar, limiting the use of drains, and opting for intravenous sedations in place of general anesthesia. The goal of this work is to prospectively study the efficacy of this modified liposuction pull-through technique for Stage I and II gynecomastia.
Methodology
Fifty-two patients were enrolled for this study. All patients had bilateral gynecomastia, and had a mean age of 26.9. Gynecomastia was type I in 10 patients (19.23%), type IIa in 25 patients (48.07%) and type IIb in 17 patients (32.7%).
The study was approved by the Department of Surgery and followed the Declaration of Helsinki, and an informed consent was signed by all patients. Inclusion criteria included all patients who presented for surgical treatment between February 2013 and March 2015. Exclusion criteria included patients who had less than 6 months follow-up, patients who had type III gynecomastia, patient treated by liposuction alone, and patients with previous chest scars.
Preoperative and postoperative photographs were taken, and subjective patient satisfaction evaluated at 6 months. This included satisfaction with four categories: cosmetic outcome, pain, change in nipple sensation and affection of shoulder movement. Patients were asked to fill out a brief intake questionnaire with Yes/No answers to the above four categories. All surgeries were performed under local anesthesia with intravenous sedation as a day case surgery.
Technique:
The surgical procedure was done under local anesthesia with intravenous sedation. Markings for the procedure were done, while the patient is in the standing position and included the inframammary folds, boundaries of liposuction as determined clinically and the skin incision. This was a single incision for each breast, measuring 8–10 mm and marked 1 cm above the inframammary fold and 1 cm lateral to the nipple line (Fig. 1). Tumescent solution containing local anesthetic with epinephrine 1:200,000 was used for subcutaneous infiltration. Liposuction was then performed to remove the fatty component of the gynecomastia, contour the pectoral region and separate the glandular tissue. Isolation of the glandular tissue aims to separate glandular tissue from its superficial (cutaneous) and the deep (muscular) attachments to facilitate its excision through the same skin incision. To achieve that, liposuction is performed along two different planes. In the deeper plane a 4-mm 3-hole cannula is used above the pectoral fascia (deep to the mammary gland). In the superficial plane, a thinner cannula was used (2 mm) to separate the breast tissue from the subcutaneous tissue and skin. Once liposuction is completed, the glandular tissue should be almost completely detached both from the deep and the superficial attachments and be only attached to the areola. Whenever needed, cross-tunneling is done by introducing the cannula from the contralateral side. Digital palpation is used to confirm the smoothness of the residual skin and fat, and to assess presence of any residual glandular tissue. This glandular tissue is clamped, pinched and grasped using a surgical hemostat passed through the same skin incision. The instrument is then pulled out through the skin, and with the aid of small hook for retraction, the glandular tissue is excised using a scalpel. Hemostasis is ensured. The removed tissue is sent for pathological examination. After glandular tissue removal has been completed, consistency and uniformity of the area are checked by palpating and pinching the skin. If there is any need for an additional liposuction, this is done by the aid of a thin cannula. The skin incision is left open for drainage. A compressive dressing is applied at the end of surgery, and an elastic garment is worn for one month.
Results
The liposuction pull-through technique successfully reduced the breast volume in all patients, and no cases had to be converted to a periareolar incision. (Figs. 2, 3, 4, 5, 6, 7) There were no cases of wound healing problems, bleeding or seroma. Ten patients (19.2%) suffered transient reduction of the nipple–areola complex sensitivity, and complete recovery was achieved within 2–6 months. The revision rate was 1.9% (1 patient). This patient had an undersection, and there was residual parenchyma evident in the subareolar area, which was later excised under local anesthesia through a small periareolar incision. No patients complained of chronic pain, cosmetic concerns (other than the one patient mentioned above) or limitation of shoulder movement.
Discussion
This case series shows that the single incision combined liposuction pull-through technique without drainage is a safe and effective treatment of gynecomastia when the skin redundancy is mild or moderate. It combines the minimally invasive features of liposuction (including short scars, ability to assess the amount of resection as it is progressing and minimal dead space) with the benefits of removing the glandular tissue. Our case series demonstrates an acceptable complications rate and high patient satisfaction. This work adds further evidence to previously published articles on the efficacy of this technique, and adds the important modification of not using a drain and using a single incision only and avoiding a periareolar incision.
Many techniques have been described for surgical correction of gynecomastia. The choice depends on the severity of the deformity in terms of breast volume and skin redundancy. The ideal technique should remove the excess mammy tissue, avoid skin redundancy and irregularities, provide an attractive male chest appearance, and minimize surgical trauma. Mladick and others stress the importance of resecting the parenchyma instead of suctioning it to have specimens for pathological examination [4]. Compared to surgical procedures that use a periareolar approach [5], the technique that we used has important aesthetic and functional advantages. These include the avoidance of periareolar incision, less risk of the dishing deformity and no permanent sensory impairment. Areolar deformities occur because of excessive tissue removal just below the areola. The skin incision used for the pull-through technique is relatively smaller (8–10 mm) and well-hidden just above the inframammary fold. Compared to liposuction alone, the combined technique allows direct visualization of the parenchyma, a more definitive removal of breast tissue with minimal risk of relapses, and direct control of bleeding and hemostasis. The pull-through technique combines the advantages of suctioning procedures with preservation and availability of breast tissue to be examined.
Various technical variations were described by several authors. Bracaglia and others [6] described their pull-through experience using three incisions. In our study, we have used a single incision only. If needed, we will use the contralateral incision for cross-tunneling. An additional incision, however, can be easily added with minimal increase in operative time or complexity if the surgeon prefers or at the beginning of adoption of the technique. Lista and Ahmad [7] also perform the liposuction pull-through technique, but with the aid of power-assisted liposuction (PAL). Ramon et al. [8] associated the PAL technique with endoscopic-assisted pull-through excision. Although PAL could possibly reduce surgical time and fatigue, we only use traditional non-powered liposuction as we feel it allows for more precise control of the skin flap thickness, especially below the NAC and along the borders of the pectoral area. Similarly, direct exposure of the parenchyma by pulling it out allowed for complete control of the excision and hemostasis, without needed an endoscope. In addition, our simplified technique does not need sophisticated instruments and is therefore easier and more economical to adopt. Moreselli and Morellini [9] described the combined liposuction and the “pull-through” technique using two incisions (one inframammary and another at the anterior axillary pillar) with a routine placement of a suction drain for 1–2 days and inpatient hospitalization. In our series, we had similar satisfactory results but with only a single well-hidden scar, no suction drain placement, and avoiding general anesthesia and inpatient admissions.
While drains are generally considered important for decreasing seroma and collapsing any dead space, they are a significant source of patient discomfort and may act as a portal for infection [10]. Patients frequently cite drains as one of the greatest discomforts in postoperative recovery, and increased number of drains has been associated with increased patient discomfort as well as longer length of hospital stay [11, 12]. While infection is relatively uncommon in gynecomastia surgery, speed of recovery and pain is an important factor, and one that patients will often inquire about before surgery. There has been a trend toward avoiding drains in procedures that were traditionally always associated with drains, such as abdominoplasty and breast reduction, and our work shows that this should be similarly applied to gynecomastia surgery.
As in many procedures, comparison of the outcomes of different techniques should be approached with caution as different surgeons have variable levels of confidence with the different techniques. An advantage of the liposuction pull-through technique is the relatively shorter learning curve, compared to direct excision though a periareolar approach. Direct excision of the gynecomastia had been reported to have a complication rate between 3 and 17% and could be higher in inexperienced hands [13–15]. The liposuction pull-through technique should be expected to have a lower likelihood of causing cosmetic deformities, as the careful surgeon will be able to judge the external appearance of the chest as the liposuction continues. Seromas and hematomas are not common after liposuction in general. Lista and Ahmed had a seroma rate of 1% in their series of 96 patients using the liposuction pull-through technique for gynecomastia, while Hammond et al. had one seroma in 27 breasts [7, 16]. Like Bracaglia et al. [6], we did not encounter any seromas with this technique.
This combined technique does have its limitations. It cannot be used for gynecomastia with significant skin excess, and experience is needed to judge the condition of the skin and the amount of skin contraction that will be needed for a good contour. A learning curve is needed, although surgeons experienced in liposuction will find it easy to judge the amount of liposuction needed to free the parenchyma without overly thinning the tissues. While the shorter and single scars and the avoidance of drains and general anesthesia will help enhance and speed recovery, the use of compression bandages is mandatory and might be bothersome to patients. However, compression bandages are the usual postoperative protocol with other gynecomastia surgeries as well. Finally, we only had a 6 month follow-up, and we therefore cannot comment on the long-term outcomes or the incidence of late recurrence. However, such recurrences should theoretically be uncommon as the glandular tissues are removed with the pull-through technique.
There are several weaknesses of the study. We used a subjective evaluation for possible complications, and recorded the answers as positive or negative. The use of a Visual Analog scale, Likert Scale or a validated outcome questionnaire would have been more accurate. While the Breast Q has been validated for female breast surgery and is becoming more commonly used, no similar method exists for male breast surgery [17]. In addition, we did not have a control group to compare our results. We have been using this technique prior to starting this work and did not feel that randomizing patients would have been ethical.
In conclusion, the single puncture combined liposuction pull-through technique is a safe and effective surgical option for types I and II gynecomastia, i.e., gynecomastia without significant skin excess. It has the advantages of the cosmetic scar, tissue sampling for pathological examination, avoidance of drains, avoidance of hospitalization and the ability of surgeons to resect as many tissues as needed thereby decreasing the incidence of under or over resection.
References
Li CC, Fu JP, Chang SC, Chen TM, Chen SG (2012) Surgical treatment of gynecomastia: complications and outcomes. Ann Plast Surg 69(5):510–515
Simon B, Hoffman S, Kahn S (1973) Classification and surgical correction of gynecomastia. Plast Reconstr Surg 51(1):48–52
Morselli PG (1996) “Pull-through”: a new technique for breast reduction in gynecomastia. Plast Reconstr Surg 97(2):450–454
Mladick RA (1991) Gynecomastia: liposuction and excision. Clin Plast Surg 18:815
Rohrich RJ, Ha RY, Kenkel JM, Adams WP (2003) Classification and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plast Reconstr Surg 111(2):909–923
Bracaglia R, Fortunato R, Gentileschi S, Seccia A, Farallo E (2004) Our experience with the so-called pull-through technique combined with liposuction for management of gynecomastia. Ann Plast Surg 53(1):22–26
Lista F, Ahmad J (2008) Power-assisted liposuction and the pull-through technique for the treatment of gynecomastia. Plast Reconstr Surg 121(3):740–747
Ramon Y, Fodor L, Peled IJ, Eldor L, Egozi D, Ullmann Y (2005) Multimodality gynecomastia repair by cross-chest power-assisted superficial liposuction combined with endoscopic-assisted pull-through excision. Ann Plast Surg 55(6):591–594
Moreslli P, Morellini A (2012) Breast reshaping in gynecomastia by the “pull-through technique”: considerations after 15 years. Ear J Plats Surg 35(5):365–371
Kumar S, Lal B, Misra MC (1995) Post-mastectomy seroma: a new look into the aetiology of an old problem. J R Coll Surg Edinb 40(5):292–294
Saratzis A, Soumian S, Willetts R, Rastall S, Stonelake PS (2009) Use of multiple drains after mastectomy is associated with more patient discomfort and longer postoperative stay. Clin Breast Cancer 9(4):243–246
Jain PK, Sowdi R, Anderson AD, MacFie J (2004) Randomized clinical trial investigating the use of drains and fibrin sealant following surgery for breast cancer. Br J Surg 91(1):54–60
Babigian A, Silverman RT (2001) Management of gynecomastia due to use of anabolic steroids in bodybuilders. Plast Reconstr Surg 107:240–242
Ratnam BV (2009) A new classification and treatment protocol for gynecomastia. Aesthet Surg J 29:26–31
Cigna E, Tarallo M, Fino P et al (2011) Surgical correction of gynecomastia in thin patients. Aesthetic Plast Surg 35:439–445
Hammond DC, Arnold JF, Simon AM, Capraro PA (2003) Combined use of ultrasonic liposuction with the pull-through technique for the treatment of gynecomastia. Plast Reconstr Surg 112(3):891–895 discussion 896-7
Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ (2009) Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 124(2):345–353
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Khalil, A.A., Ibrahim, A. & Afifi, A.M. No-Drain Single Incision Liposuction Pull-Through Technique for Gynecomastia. Aesth Plast Surg 41, 298–303 (2017). https://doi.org/10.1007/s00266-016-0749-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-016-0749-z