Abstract
Objective
To develop a new patient-reported outcome instrument (PRO) to measure body-related satisfaction quality of life (QoL).
Methods
Standard 3-phase PRO design was followed; in the first phase, a qualitative design was used in 45 patients to develop a conceptual framework and to create preliminary scale domains and items. In phase 2, large-scale population testing on 1340 subjects was performed to reduce items and domains. In phase 3, final testing of the developed instrument on 34 patients was performed. Statistics used include Factor, RASCH, and multivariate regression analysis. Psychometric properties measured were internal reliability, item-rest, item-test, and test–retest correlations.
Results
The PRO-developed instrument is composed of four domains (satisfaction with the abdomen, sex life, self-esteem and social life, and physical symptoms) and 20 items in total. The score can range from 20 (worst) to 100 (best). Responsiveness was 100 %, internal reliability 93.3 %, and test–retest concordance 97.7 %. Body image-related QoL was superior in men than women (p < 0.001) and decreased with increasing age (p = 0.004) and BMI (p < 0.001). Post-bariatric body contouring patients score lower than cosmetic patients in all domains of the Body-QoL instrument (p < 0.001). After surgery, the score improves by on average 21.9 ± 16.9 (effect size 1.8, p < 0.001).
Conclusions
Body satisfaction-related QoL can be measured reliably with the Body-QoL instrument. It can be used to quantify the improvement in cosmetic and post-bariatric patients including non- or minimally invasive procedures, suction assisted lipectomy, abdominoplasty, lipoabdominoplasty, and lower body lift and to give an evidence-based approach to standard practice.
Level of Evidence I
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Evidence-based medicine has changed the way in which health practitioners provide medicine [1–3]. Nowadays in most areas of medicine, if a new treatment has not been proven effective in a properly designed randomized controlled trial, it is very unlikely to become standard practice; on the contrary, classic interventions that have proven ineffective quickly become forgotten and replaced by newer more effective interventions [4, 5].
All study designs that aim to determine the efficacy of a treatment should at least specify an intervention, a population in whom the intervention will be tested and an outcome that must be clinically relevant to patients. [6, 7].
In aesthetic surgery, the direct objective is making a segment of the anatomy more beautiful. Although beautification of the body is the obvious objective for patients, the reasons to undergo a risky and expensive procedure are of a more complex nature [8]. Dissatisfaction with body image can negatively impact on several aspects of quality of life (QoL). Patients that are not satisfied with their body image often have sex life impairment; low self-esteem, social isolation, and feel rejected by their peers, even impacting their function at work, social and personal life. Mild cases of abdominal skin sagging present few physical symptoms; but moderate to severe abdominal ptosis can lead to a bulge sensation in the abdominal area, pain and fold moisture-related problems such as excoriation or fungus development. These symptoms are not unique to the massive weight loss (MWL) population, but also shared with those so-called cosmetic patients [8, 9].
Accordingly, the underlying objective of cosmetic procedures is to improve QoL by means of making the body more beautiful. Therefore, a reliable way to measure the efficacy of body contouring surgery (BCS) is to measure its impact on QoL from the patients’ perspective and to consequently measure all psychological, social, and physical aspects that a patient may feel are attributable to their self-body image impairment.
The current best approach to measure qualitative outcomes is through questionnaires developed using systematic and reproducible methods [10–12], using a mixed qualitative and quantitative approach. These rigorously developed questionnaires are valid and reproducible and as a result are trusted that they accurately measure the phenomena for which they were developed. In particular, instruments that assess phenomena from the patient perspective are called Patient-Reported Outcome Measures (PRO or PROMs).
No such instruments exist specifically designed for BCS patients, neither cosmetic, nor MWL patients. [13, 14]
Given the lack of a valid instrument for such a common problem, we aimed to develop a new PRO to measure body-related satisfaction and QoL for patients undergoing body contouring procedures such as liposuction, abdominoplasty, or body lift.
Methods
Design
The study was approved by the ethics committee and Institutional Review Board [15]. All patients gave written informed consent to participate in the study.
A standard 3-phase design for PRO development was followed [16, 17]; the detailed information of the design has been described [9].
Briefly, phase 1a aimed to create the preliminary instrument, exhaustive literature review, and in-depth interviews with 16 patients before and after the surgeries were performed. From the literature review and in-depth interviews, a preliminary instrument was created. This was subsequently tested for understanding and wording on an independent sample of 29 patients before the surgery, following which the preliminary Body-QoL reached 5 domains and 120 items.
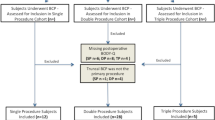
In phase 2, the preliminary Body-QoL was tested in a large scale and scope of patients. Three samples were drawn: (1) general population, (2) a surgical cohort of patients undergoing BCS, and (3) a historic population of patients between 1 and 3 years after BCS. The objective of phase 2 is to reduce the number of items and domains to the most robust and sensitive ones, using appropriate statistical tests to select the items.
In phase 3, the reduced scale was tested on another sample of patients to measure the final psychometric properties.
Sampling and Patients
In phase 2, we aimed to sample a large scope of patients ranging from normal individuals to most severely diseased. For that reason, we sampled members of the general population and BCS patients. For the general population group, forms were distributed by paper to non-plastic surgery patients and patient companions at the hospital, university students, and hospital staff, and electronically distributed freely and anonymously by email, Google drive, and Facebook.
The historical population was conformed by all the patients in whom BCS had been performed, including liposuction, abdominoplasty, lipoabdominoplasty, and lower body lift. Patients were contacted by telephone and email.
The before/after cohort was composed of all patients operated on between June 2013 and March 2014 at our institution scheduled for BCS procedures that consented to participate in the study and returned at least one form. The preoperative Body-QoL instrument was administered prior to the surgery in the week before or as soon as the patient attended the hospital. The postoperative Body-QoL application was administered by email 3 months after the surgery.
Preliminary Body-QoL Characteristics and Other Variables
The phase 2 Body-Qol was a 120-item instrument clustered in five domains: (A) clothing and physical appearance, (B) sexual and emotional life, (C) body image and self-esteem, (D) social relations, and (E) physical symptoms. Items were organized as Likert questions in which a statement is made and the patient rates their agreement with the statement on an ordinal scale ranging from 1 to 5 (strongly disagree to strongly agree).
After the reduction of the instrument, the final scale was administered to a small sample of 34 patients and repeated 2–4 weeks after to determine test–retest correlation coefficient, and time to complete the scale and scale responsiveness.
The Body-QoL questionnaire was self-administered in paper or in electronic forms that can be answered via personal computer or handheld devices such smart phones or tablets on our website (http://www.bodyqol.org).
Besides the Body-QoL questionnaire, demographic characteristics were asked, and in the before/after surgery cohort population comorbidities, surgical procedures and technical aspects of the surgery were also recorded.
Statistics
The total study sample population of phase 2 was divided into an exploratory sample and a confirmatory sample. The exploratory sample comprised the general population that had not had any previous BCS as well as the before form of the surgical cohort. The confirmatory sample comprised the patients in the control group that did have previous BCS, the historic patients, and the “after” form response of the before/after surgical cohort.
For the item reduction, only the exploratory sample was used.
In the exploratory sample, RASCH analysis and Factor analysis were performed to select the best discriminating items and to reduce domains.
We reduced the items until we reached a lower boundary of Cronbach’s alpha of 90 %.
Once adequate internal consistency was achieved, we tested the selected items in confirmatory factor analysis.
Finally, to evaluate our construct validity, the reduced scale was tested on the confirmatory population (initially left out from the analysis) performing logistic regression to test the capacity to predict the score after the surgery and to test predictive validity or the capacity to discriminate between the control population that want to have BCS from people who were fit, with normal body mass index and who do not want to have BCS. Also, linear models were used to assess how different risk factors and population groups affected the Body-QoL score.
Among the psychometric properties of the scale, we calculated item responsiveness, internal reliability (Cronbach’s alpha), item-test correlation, item-rest correlation, test–retest concordance correlation coefficient, and time to complete the scale [13, 21].
Other standard statistical tests used were Mann–Whitney and Kruskal–Wallis tests to test ordinal outcomes between different groups, t test and one-way ANOVA to test continuous or normalized variables between groups, and linear and fractional polynomial regression models and Z proportion test for binary variables.
In all statistical tests, an alpha value equal to or less than 0.0500 was considered statistically significant.
For data analysis, STATA® 12.0 (StataCorp, TX, USA) and SPSS® software were used. Body-QoL electronic administration was performed via our study website or powered by Google Drive forms.
Bias Control
Specific maneuvers to control bias inherent to PRO [10, 12, 16, 17] development were undertaken. To assure content validity (face validity), domain and item generation were performed using qualitative methods (in-depth interviews) in phase 1a; furthermore, an exhaustive literature review was performed and expert opinions were retrieved. During phase 1b, pilot-testing for feedback of relevance was done in 29 patients. Also in phase 2, unstructured interviews were performed with patients to enquire about problems in the preliminary instrument; however, no relevant information was retrieved that differed from previous phases.
In the absence of a gold standard or reference pattern to compare with, to test construct validity, different populations were compared. A priori, at least it was expected that the Body-QoL:
-
Score was lower in the obese population than the eutrophic population.
-
Score was lower in preoperative BCS patients than in the general population.
-
Improves after BCS in all domains.
-
Score was lower in post-bariatric patients compared with cosmetic patients.
Sensitivity to change validity was tested determining change in preoperative versus postoperative scores. Also, predictive validity was tested, calculating the capacity of the Body-QoL score to differentiate between the preoperative and postoperative population.
Results
In phase two, a total of 1346 forms were completed by 1200 persons. The response rate for the surgical before/after cohort was 63.7 % (109/171). The response rate for the general population cannot be calculated exactly, but the dropout rate (patients that stopped responding after opening the form) was 15.7 % (211/1346). The general characteristics of populations are depicted in Table 1.
After RASCH and Factor analysis, four factors explain our construct with robust internal reliability. Therefore, we decided to reorganize our scale in four domains of 5 items each, ranging from 20 (worst) to 100 (best) score. Resulting domains after reduction are (1) satisfaction with your body, (2) sex life, (3) self-esteem and social performance, and (4) physical symptoms.
Scale internal reliability was 93.3 % for the whole population, 93.6 % for cosmetic patients, and 92.2 % for post-bariatric patients. By surgery type, reliability was 93.4 % for liposuction, 93.6 % for abdominoplasty, and 96.3 % for body-lift patients. Responsiveness of the scale was 100 %. Time to complete the final instrument was 4.3 ± 2.3 min. The definitive Body-QoL instrument is shown in Table 2, and psychometric properties collapsed by domain are depicted in Table 3.
Among the studied factors in the multivariate analysis, female gender (p < 0.001), increasing BMI (p < 0.001), and increasing age (p = 0.004) significantly decrease body-related QoL (Figs. 1 and 2). Also, patients who did not want to have any BCS scored better than patients who wanted to have a procedure (median 79 vs. 67 points, p < 0.0001) and patients who have had previous BCS scored better than the control population regardless of their desire to have a BCS or not (median 86 vs. 74, p < 0.0001, Fig. 3). The detailed descriptive statistics of Body-QoL score stratified by gender, age, and BMI are shown in Table 4.
In the surgical cohort, the score improved significantly from preoperative and 3 months after surgery [53 (IQR 42–60) to 82 (IQR 72–91)], p = 0.0008, Fig. 4) Differences between preoperative and postoperative scores were on average 21.9 ± 16.9 (range 4–55) with an effect size (ΔScore/SD1) of 1.8.
Also, all domain scores showed significant improvements in body satisfaction (Fig. 5). Preoperative scores were significantly different (p = 0.0391) between liposuction (58.5 ± 23.3), lipoabdominoplasty (52.1 ± 11.8), and body-lift patients (50.3 ± 13.6), as shown in Fig. 6. In post-bariatric patients, preoperative and postoperative scores were lower than in cosmetic patients (p = 0.0142 and p = 0.0206), but the improvement before and after the surgery was equal between populations (22.2 ± 5.3 vs. 21.2 ± 6.1, p = 0.9179, Fig. 7). Post-bariatric patients scored lower on all domains compared with cosmetic patients (p values 0.0312, 0.0026, 0.0057, and 0.0104 for domains A, B, C, and D, respectively, Fig. 8).
Normalized Body-QoL® scores stratified by surgery (Mean 52.2 [0], SD 12.1 [1] )
Discussion
Our study was conducted according to current best standards for PRO development [10, 16, 17]. In phase 1, items were developed taking account of the patient perspective, expert opinion, and comprehensive literature review to ensure content validity.
Large-scale application in phase 2 was conducted in a large scope population, including individuals of widespread ages, weight, BMI, level of education, and desire for surgery and in both preoperative and postoperative patients. The reason for that methodological decision was to ensure the good performance of the Body-QoL in all populations, so the instrument can be used to measure satisfaction with the body not only in plastic surgery patients but also in other populations such as bariatric surgery patients or other scientific fields. Definitive items were chosen according to their psychometric properties, focusing on the development of an instrument sensitive to change and with content validity for the whole spectrum of disease, reflected in the patient characteristics for their BMI, abdominal ptosis severity, and the surgery performed (liposuction, lipoabdominoplasty, or abdominoplasty and body lift). After item reduction, all our previous hypotheses to validate our construct validity were proven; in the absence of a gold standard or reference pattern, the mentioned comparisons built up our construct validity.
We chose to keep scoring as simple as possible, giving all items a score from 1 to 5, in that way the total score is calculated easily, by just adding each domain subtotal score and allowing direct comparison between preoperative and postoperative or any comparison that a clinician or researcher wants to perform.
The main threats to validity in PRO are the content validity (ensuring that the instrument includes all the scope of the phenomena to be measured) and construct validity (demonstrating that the instrument performs as theoretically expected or compared with a gold standard) [10, 16, 17]. As described in the methods section, we take care to prevent bias in all research steps.
Other researchers have chosen to develop different scales based on the procedure. We think that PRO should be patient based rather than procedure based. In our perspective as plastic surgeons and researchers, the satisfaction with the body is a continuum ranging from mild dissatisfaction to severe dissatisfaction, quite often (but not always) dissatisfaction is related to anatomical abnormalities, and a wide range of procedures can be selected to improve the anatomical problem and consequently restore body-related satisfaction. If a single scale is developed for each procedure, for example, one for liposuction, one for abdominoplasty, and another for body lift, then it will be impossible to compare differences between populations or procedures. Any clinician is aware that more than often a single patient can choose between different procedures with similar results, and in plastic surgery, there are a wide range of procedures and combinations than can be performed; from our point of view, it would be impractical to use and implement one different scale for different procedures. Therefore, we choose to approach the phenomena ‘body related QoL’ from a generic perspective to compare different procedures and different populations.
Another question that this study cannot answer is if the motivations for surgery are the same in other populations in different countries and continents. Although widespread availability of plastic surgery can lead to the assumption that motivations should be the same, these assumptions must be tested, validating the Body-QoL questionnaire in other languages and different populations.
This is the first reported PRO specifically developed to measure body satisfaction-related QoL for plastic surgery patients. Other generic instruments like SF 36 [18], Patient Health Questionnaire, and Generalized Anxiety Disorder [19] have been used and failed to demonstrate improvement of QoL after BCS on MWL populations. We think that the difference in our findings can be explained because generic instruments are not sensitive enough to detect such changes. Other instruments related to obesity have been used with good results [20–24], but quite often they ask questions that are not relevant for the cosmetic population (lipoabdominoplasty or lipoplasty patients). [13, 14]
In our study, we found that patients with higher BMI have lower self-esteem; this has been properly documented previously by several authors [25, 26]. An interesting finding is that men, even when they get older, have higher self-esteem than women, although our study can only show association and we can only hypothesize about our results. In fact women suffer at least a twofold increase in depression, anxiety, and somatic complaints than men [27]; moreover, women feel pressed by the media, peers, and couples to look slimmer and younger, and this is a transcultural phenomena [28–31] and indirectly supported by the fact that more than 90 % of cosmetic procedures globally are performed on women [32]. Although in males, body-related QoL decreases with obesity, it increase with age suggesting that self-esteem in males is related to other life aspects, different than body image, like professional or academic success, money income, or power. Our explanation for the observed phenomena is merely theoretical, due to the lack of evidence in gender determinations of self-esteem [33].
Our data show that liposuction patients score higher than lipoabdominoplasty patients and the latter higher than body-lift patients, this can be explained by a gradient of the body contour distortion (decrease on the Body-QoL score), the more severe, the more aggressive procedure is needed to restore the body contour.
Surprisingly, patients who had previous body contouring procedures scored better on the Body-QoL than other women, even women who did not want a body contouring procedure. We think that this finding may be true in nature or related to this subgroup of women being more self-conscious about their body-related QoL.
The Body-QoL instrument can be easily used in clinical practice, it is self-administered, and the questions are in lay language. It should be used at least one time before surgery and one time after surgery, once definitive results are achieved.
The Body-QoL opens a whole new research area providing a means of measuring something that has never been measured before. It can be used to compare before and after within patients and can also be used to compare between techniques used as a main outcome measure in randomized controlled trials. Also in cohort or case–control studies, it can be used to identify the profile of patients with lower or better improvement in body satisfaction-related QoL.
In the development of the Body-QoL, two different problems emerge: (1) surgeon perspective of the result and (2) postoperative pain and discomfort experienced by the patient after surgery. We choose to separate the phenomena into three different scales. Accordingly, the Body-QoL® aims to measure QoL, the Body-PPDS® (Postoperative Pain and Disability Scale) to measure impairment from the patient perspective, and the Body-PSSOAS® (Patient/Surgeon Subjective/Objective Assessment Scale) will target the surgeons’ and patients’ perspectives of technical details of the surgery such as contour, naturalness of the result, and scar problems. Both the Body-PSSOAS and Body-PPDS are in phase 2 of development and together they all conform the Body-PROM instrument.
Conclusion
Body satisfaction-related QoL can be measured with high reliability with the Body-QoL instrument. It has adequate sensitivity to change, good reliability and consistence. Body-related QoL perception is better in men than women and decreases as body mass index increases. Regarding age, satisfaction with body in men slightly increases with age; women on the contrary improve their body satisfaction reaching their peak in their 20′s and steadily decreasing after their 30′s. Patients who have undergone BCS have better body satisfaction than patients who have not. Also, patients improve their body satisfaction after surgery. MWL patients have worse body satisfaction than other groups of patients; they improve after surgery reaching values similar to those of the normal population.
References
Chung KC, Ram AN (2009) Evidence-based medicine: the fourth revolution in American medicine? Plast Reconstr Surg 123:389–398
Chassin MR, Galvin RW (1998) The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA 280:1000–1005
Offer GJ, Perks AG (2000) In search of evidence-based plastic surgery: the problems faced by the specialty. Br J Plast Surg 53:427–433
Rossouw JE, Anderson GL, Prentice RL et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 288:321–333
Gilbert R, Salanti G, Harden M, See S (2005) Infant sleeping position and the sudden infant death syndrome: systematic review of observational studies and historical review of recommendations from 1940 to 2002. Int J Epidemiol 34:874–887
Hulley S, Cummings S, Browner W, Grady D, Hearst N, Newman T (2001) Designing clinical research, an epidemiologic approach, 2nd edn. Lippinkott Williams and Wilkin, Philadelphia
Sackett DL, Haynes RB, Guyatt G, Tugwell P (1991) Clinical epidemiology. a basic science for clinical medicine, 2nd edn. Little, Brown and Company, Boston
Klassen AF, Cano SJ, Scott A, Johnson J, Pusic AL (2012) Satisfaction and quality-of-life issues in body contouring surgery patients: a qualitative study. Obes Surg 22:1527–1534
Danilla S, Dominguez C, Cuevas P, Calderón ME, Rios MA, Andrades P, Benitez S, Erazo C, Shulz R, Al-Himdani S, Sepúlveda S (2014) The Body-QoL®: measuring patient reported outcomes in body contouring surgery patients. Aesthetic Plast Surg 38:575–583
Streiner D, Norman G (2008) Health measurement scales, a practical guide for their development and use, 4th edn. Oxford University Press, Oxford
Fletcher R, Fletcher S, Wagner E (1996) Clinical Epidemiology, the essentials, 3rd edn. Williams and Wilkins, Baltimore
Pusic AL, Lemaine V, Klassen AF, Scott AM, Cano SJ (2011) Patient-reported outcome measures in plastic surgery: use and interpretation in evidence-based medicine. Plast Reconstr Surg 127:1361–1367
Reavey PL, Klassen AF, Cano SJ, McCarthy C, Scott A, Rubin JP, Shermak M, Pusic AL (2011) Measuring quality of life and patient satisfaction after body contouring: a systematic review of patient-reported outcome measures. Aesthet Surg J 31:807–813
Jabir S (2013) Assessing improvement in quality of life and patient satisfaction following body contouring surgery in patients with massive weight loss: a critical review of outcome measures employed. Plast Surg Int. doi:10.1155/2013/515737
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Johnson C, Aaronson N, Blazeby J, Bottomley A, Fayers P, Koller M et al (2011) Guidelines for developing questionnaire modules, 4th edn. EORTC Quality of Life Group, Brussels
U.S. Department of Health and Human Services. Food and Drug Administration. Center for Drug Evaluation and Research (CDER). Center for Biologics Evaluation and Research (CBER). Center for Devices and Radiological Health (CDRH) (2009). Guidance for industry, patient-reported outcome measures: use in medical product development to support labeling claims. Document availiability: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm
Brazier JE, Harper R, Jones NM et al (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Azin A, Zhou C, Jackson T, Cassin S, Sockalingam S, Hawa R (2014) Body contouring surgery after bariatric surgery: a study of cost as a barrier and impact on psychological well-being. Plast Reconstr Surg 133:776e–782e
van der Beek ES, Geenen R, de Heer FA, van der Molen AB, van Ramshorst B (2012) Quality of life long-term after body contouring surgery following bariatric surgery: sustained improvement after 7 years. Plast Reconstr Surg 130:1133–1139
Balagué N, Combescure C, Huber O, Pittet-Cuénod B, Modarressi A (2013) Plastic surgery improves long-term weight control after bariatric surgery. Plast Reconstr Surg 132:826–833
Staalesen T, Fagevik Olsén M, Elander A (2013) Experience of excess skin and desire for body contouring surgery in post-bariatric patients. Obes Surg 23:1632–1644
Singh D, Zahiri HR, Janes LE, Sabino J, Matthews JA, Bell RL, Thomson JG (2012) Mental and physical impact of body contouring procedures on post-bariatric surgery patients. Eplasty 12:e47
Modarressi A, Balagué N, Huber O, Chilcott M, Pittet-Cuénod B (2013) Plastic surgery after gastric bypass improves long-term quality of life. Obes Surg 23:24–30
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG (2010) Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67(3):220–229
Herva A, Laitinen J, Miettunen J, Veijola J, Karvonen JT, Läksy K, Joukamaa M (2006) Obesity and depression: results from the longitudinal Northern Finland 1966 Birth Cohort Study. Int J Obes 30(3):520–527
Department of Mental Health and Substance Dependence, World Health Organization (2012). gender disparities in mental health: the facts. http://apps.who.int/iris/bitstream/10665/66539/1/WHO_MSD_MDP_00.1.pdf. Accessed 1 Oct 2015
Chaker Z, Chang FM, Hakim-Larson J (2015) Body satisfaction, thin-ideal internalization, and perceived pressure to be thin among Canadian women: the role of acculturation and religiosity. Body Image 14:85–93
Lev-Ari L, Baumgarten-Katz I, Zohar AH (2014) Mirror, mirror on the wall: how women learn body dissatisfaction. Eat Behav 15(3):397–402
Nerini A, Matera C, Stefanile C (2014) Psychosocial predictors in consideration of cosmetic surgery among women. Aesthet Plast Surg 38(2):461–466
Yean C, Benau EM, Dakanalis A, Hormes JM, Perone J, Timko CA (2013) The relationship of sex and sexual orientation to self-esteem, body shape satisfaction, and eating disorder symptomatology. Front Psychol 27(4):887
ISAPS International Survey on Aesthetic/Cosmetic Procedures Performed in 2014. http://www.isaps.org/Media/Default/global-statistics/2015%20ISAPS%20Results.pdf. Accessed 1 Oct 2015
Piccinelli M, Wilkinson G (2000) Gender differences in depression critical review. Br J Psychiatry 177:486–492
Acknowledgments
The authors acknowledge Dr. Graeme Perks for his enthusiastic and unconditional support, Dr. David Streiner for his wise advice, Cristina Di Silvestre M.Sc. for her help in the qualitative design and running phase 1a of the study, Solange Cortes R.N. for her hard work in performing, collecting, and transcribing the forms, and all of the General Surgery and Plastic Surgery residents at the University of Chile, who spent many hours filling forms and databases.
Financial disclosure
Stefan Danilla owns intellectual proprietary patent registry for Body-QoL®™ and Body-PROM®™. The Body-PROM® and its modules (Body-QoL, Body-PSSOAS and Body-PPDS) are free to use for academic and non-profit organization.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Danilla, S., Cuevas, P., Aedo, S. et al. Introducing the Body-QoL®: A New Patient-Reported Outcome Instrument for Measuring Body Satisfaction-Related Quality of Life in Aesthetic and Post-bariatric Body Contouring Patients. Aesth Plast Surg 40, 19–29 (2016). https://doi.org/10.1007/s00266-015-0586-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-015-0586-5