Abstract
Background
Keloid is a fibrotic skin disease for which immune cell infiltration is a primary pathological hallmark. Meanwhile, in autoimmune diseases, triggering of the inflammation response can lead to tissue injury and subsequent organ fibrosis. When the skin is involved in autoimmune disease, skin fibrosis such as that seen in scleroderma can occur. In this study, we propose that keloid possesses features of autoimmune disease.
Methods
To verify whether keloid possesses features of autoimmune disease, immune cell infiltration and immune complex deposits were detected with immunohistochemical staining and immunofluorescence, respectively, in keloid and normal skin tissues. A routine antinuclear antibody profile was tested in sera from 28 keloid patients and 28 healthy controls. Lastly, the anti-hnRNPA2B1 autoantibody in sera was evaluated by enzyme-linked immunosorbent assay.
Results
The numbers of CD1α+ Langerhans cells, CD3+ T lymphocytes, CD68+ macrophages, and CD20+ B lymphocytes increased in keloid tissues compared to normal skin. IgA, IgM, C3, and C1q deposits were found in keloid tissues but not in normal skin, while anti-hnRNPA2B1 levels in sera from keloid patients were elevated.
Conclusion
The above findings suggest that keloids have some characteristics that are similar to autoimmune disease and might be mediated by autoimmune responses.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The skin fibrotic disease keloid is characterized by excessive extracellular matrix accumulation. Unlike normal or hypertrophic scars, keloids do not regress with time but instead persist indefinitely and extend beyond the original wound margin boundaries to invade the surrounding normal tissue [1]. Keloids are not only aesthetically displeasing, but can also be both painful and functionally disabling, as well as cause physical and psychological distress for patients [2, 3]. Although a lot about the pathophysiology of keloids has been reported, the exact pathogenesis has not been completely elucidated, and its high recurrence makes keloid one of the major unsolved clinical challenges in wound healing [4]. In addition, there is no screening biomarker for keloid susceptible individuals, which increases the morbidity in surgery.
During its pathological process, inflammatory cell infiltration is commonly seen in keloid tissues [5]. In fibrosing organs, macrophages are a major source of TGF-β1, one of the most important fibrogenic cytokines, while T and B lymphocytes can facilitate secretion of other fibrogenic cytokines [6, 7]. Several studies demonstrated that in autoimmune diseases the inflammation response can cause tissue injury that leads to organ fibrosis seen in diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), autoimmune pancreatitis, and scleroderma (SD) [8]. SD is a systemic autoimmune disease that affects various organs, including skin, where it can lead to skin fibrosis [9], which shares similar pathology and microenvironments with keloid [5, 10, 11]. Therefore, keloid may have some characteristics that are similar to autoimmune disease.
Autoimmune diseases are characterized by the presence of autoantibodies that cause organ and tissue injury through various pathways, and can serve as predictive, diagnostic, and prognostic tools for some autoimmune diseases in clinical practice [12]. While many substances in the body can act as autoantigens that induce autoantibody production, the most common are components of the nucleus and cytoplasm. Antinuclear antibodies (ANAs) are defined as autoantibodies that recognize a broad spectrum of not only nuclear, but also cytoplasmic components, such as centriole and nucleosomes [13, 14]. Measurement of ANAs is one of the most well-known tests for autoimmune diseases, and is an antecedent of screening biomarkers that can potentially be very informative [15]. Moreover, in autoimmune disease lesional sites, immune complexes (ICs) are frequently formed following binding of antigens with antibodies. ICs that lodge in the capillaries, as well as the surrounding basement membrane and tissues, can trigger inflammatory responses, activate the complement system, promote accumulation of immune cells and lead to tissue injury [16].
To determine whether keloid possesses features of autoimmune diseases, immune cell infiltration in keloid tissue and normal skin was detected by immunohistochemical staining and IC deposits were evaluated using direct immunofluorescence. In addition, a routine ANA profile was screened in sera from 28 keloid patients and 28 healthy controls. Lastly, another autoantibody, anti-hnRNPA2B1, was also measured in sera by ELISA.
Materials and Methods
Patients and Samples
Twenty-eight patients (10 men and 18 women; mean age 30.0 years; range 19–59 years) were recruited for this study. They fulfilled the currently accepted criteria for keloid, defined as the presence of typical skin lesions confirmed by two plastic surgeons. Duration of disease ranged from 1.5 to 17 years. Lesions were located on the anterior chest wall (11), shoulder (3), chin (3), ear (3), abdomen (2), neck (1), arm (1), and two or more sites (4). Lesions caused pain or itching in 21 patients and displayed redness in 15 patients. Patients did not have laser, radiation, cryotherapy or intralesional treatment within the previous 6 months. In addition, 28 age- and gender-matched healthy subjects (8 men and 20 women; mean age 32.6 years; range 18–57 years) who displayed no keloid, hypertrophic scars or current infections were enrolled as controls. No subject had received hormone, immunosuppressant, or antitumor drugs in the last 1 year. Blood samples were collected into evacuated specimen collection tubes by clean puncture of an antecubital vein. Sera obtained after centrifuging the blood samples at 2500×g for 15 min were frozen in small aliquots and stored at −80 °C prior to use. Keloid specimens were harvested from patients at the time of surgical excision, while normal skin specimens were obtained from patients who underwent surgical procedures for cosmetic reasons.
The study protocol was approved by the Ethical Committee of the Institution, and in accordance with the Declaration of Helsinki Principles. Written informed consent was obtained from all subjects.
Immunohistochemistry
Skin samples were fixed in 10 % formalin solution and then processed for paraffin sectioning. Mouse monoclonal antibodies directed against Langerhans cells, T and B lymphocytes and macrophage CD1α, CD3, CD20, and CD68 (Zhongshan, Beijing, China) were used as primary antibodies. Horseradish peroxidase-conjugated rabbit anti-mouse IgG acted as the secondary antibody and was purchased from Abcam (Hong Kong, China). Staining was achieved using a DAB Stain kit (Zhongshan, Beijing, China). Sections were counterstained with hematoxylin. The numbers of Langerhans cells, T lymphocytes, B lymphocytes, and macrophages were counted in one random high power field (400× total magnification) five times.
Immunofluorescence Studies
Direct immunofluorescence for IgA, IgM, IgG, C1q, and C3 was performed as described previously [8]. Briefly, the skin specimens to be examined were snap frozen in liquid nitrogen, cut with a cryostat at about −20 °C, air-dried and fixed in cold acetone. The sections were incubated with a fluorescein isothiocyanate (FITC)-conjugated polyclonal rabbit antibody directed against C1q (Dako, Glostrup, Denmark, working dilution 1:40), C3c (Dako, Glostrup, Denmark, working dilution 1:30), IgA (Dako, Glostrup, Denmark, working dilution 1:20), IgG (Dako, Glostrup, Denmark, working dilution 1:80) or IgM (Dako, Glostrup, Denmark, working dilution 1:40). After the unbound antibodies were removed by washing, the slides were examined by two independent experienced pathologists with a fluorescence microscope. Pathologists determined the slides were positive or negative through comparing with blank control.
Line Immunoassays
Routine-specific ANAs were examined by a line immunoassay purchased from Euroimmun® Lübeck, Germany. The assay contains the following antigens: centriole, PCNA, nucleosomes, Ro 52, PM-Scl, CENP-B, histones, cytoplasm, AMA M2, nRNP/Sm, Sm, SS-A, SS-B, Scl-70, Jo-1, and ribosomal P protein on nylon strips coated with recombinant and purified antigens in discrete lines on a plastic backing. The nylon strip was incubated with serum at a 1:101 dilution in a test trough. Next, goat anti-human IgG labeled with alkaline phosphatase was overlaid on the strip to bind the autoantigen-autoantibody complex. 5-bromo-4-chloro-3-indolyl phosphatase added into the test trough reacted with enzyme substrate to produce a dark brown color in proportion to the amount of specific autoantibody in the test sample. Last, each line of the test strip was scanned and analyzed using image analysis software (EUROLineScan).
Enzyme-Linked Immunosorbent Assay (ELISA)
An ELISA kit (CUSABIO, Wuhan, China) was used to analyze the titer of autoantibodies to hnRNPA2B1. Human sera were diluted 1:200 in sample buffer and incubated. The liquid from each well was then removed and the bound antibodies were detected by incubation with a Biotin-conjugate working solution. Horseradish peroxidase-avidin solution was added to react with the Biotin-conjugate antibody. Incubation of a tetramethylbenzidine substrate resulted in an enzyme-substrate reaction indicated by a change in color. The optical density was read at 450 nm.
Statistics Analysis
Statistical analyses were performed using the SPSS version 16.0 (SPSS, Chicago, IL, USA). Data are expressed as mean ± SD. Student’s t test and the χ 2 test were used to compare group continuous and categorical variables, respectively. The level of statistical significance was set at p < 0.05.
Results
Infiltrated Immune Cells Increased in Keloid Tissues Compared to Normal Skin
To examine the infiltration of immune cells in tissues, CD1α+ Langerhans cells, CD3+ T lymphocytes, CD68+ macrophages, and CD20+ B lymphocytes were evaluated using immunohistochemical staining; the results showed that there were more infiltrated immune cells in keloid lesions compared to normal skin. The keloid tissues also showed a significantly higher presence of Langerhans cells than normal skin (Fig. 1a–c). In keloid lesions, CD3+ T lymphocytes were mainly found in close association with vessels, and in the upper dermis as aggregates with scattered single cells also present (Fig. 1e). Meanwhile, in normal skin only a few T lymphocytes were occasionally observed in the perivascular region of blood vessels (Fig. 1d). CD68+ macrophages varied greatly in shape and were scattered throughout the dermis of both keloid and normal skin samples, although the number of macrophages was significantly increased in keloid skin compared to normal skin (Fig. 1g–i).
Immunostaining of immune cells in keloid tissues and normal skin. Representative immunostaining from normal skin (a, d, g, j) and keloid (b, e, h, k). Sections were stained with specific antibodies to CD1α (a, b), CD3 (d, e), CD68 (g, h), and CD20 (j, k) using the streptavidin biotin complex/horseradish peroxidase method and counterstained with hematoxylin. Bars 10 μm. The rate of CD1α+ (c), CD3+ (f) and CD68+ (i) cells were calculated. Mean ± SD values are indicated (*p < 0.05, **p < 0.01, ***p < 0.001)
Interestingly, in keloid skin CD20+ B lymphocytes formed large and compact aggregates located in the upper dermis, with a few B lymphocytes found in the deep dermis (Fig. 1k). However, in normal skin, only occasional scattered single B lymphocytes were observed, and aggregates formed by B lymphocytes were completely absent (Fig. 1j).
Immunoglobulin and Complement Deposits were Found in Keloid Tissues but Not in Normal Skin
To detect immunoglobulin and complement deposition in tissues from keloid patients and healthy controls, direct immunofluorescence for IgA, IgM, IgG, C1q, and C3 was performed. IgA deposits were detected in keloid tissues (3 in 8 specimens), which were lumpy and located in the papillary dermis, but similar IgA deposits were absent in normal skin (Fig. 2a, b). Neither tissues showed IgG-positive deposits (Fig. 2c, d). IgM (4 in 8 specimens), C1q (6 in 8 specimens), and C3 (6 in 8 specimens) deposits were found in keloid tissues, with dense C3-positive deposits being present in particular at large diameter vessels (Fig. 2f, h, j). In contrast, no IgM-, C1q- or C3-positive deposits were present in normal skin (Fig. 2e, g, i).
Immunofluorescence staining of immunoglobulin and complement deposits in keloid tissues and normal skin. IgA (a, b), IgG (c, d), IgM (e, f), C1q (g, h), and C3 (i, j) were detected by direct immunofluorescence with DAPI nuclear staining. White dotted lines indicate basal membrane. Arrows indicate immune complexes. Bars 10 μm
Levels of Anti-hnRNPA2B1 in Sera from Keloid Patients Increased Compared to Normal Control with a Similar Antinuclear Antibody Profile
A line immunoassay was used to measure ANAs in sera from keloid patients and healthy controls (Table 1). The results showed that one was anti-Ro 52 positive, one was anti-histone positive and one was positive for anti- SS-A in 28 keloid patients. One of 28 healthy controls was positive for anti-AMA M2, one for anti-nRNP/Sm and two for anti-SS-B. The differences did not achieve statistical significance.
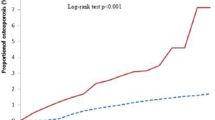
To detect anti-hnRNPA2B1 in sera samples, ELISA was performed. Interestingly, sera from patients with keloid had mean anti-hnRNPA2B1 levels (149.32 ± 83.22 mU/ml) that were significantly higher than that in normal controls (70.47 ± 37.98 mU/ml) (p < 0.05) (Fig. 3). A titer higher than the cut-off value (146.43 mU/ml), which was calculated as the mean ± 2SD of the normal control samples, was considered a positive high antibody index. Thirteen patients were found positive for anti-hnRNPA2B1, and only one normal control was positive.
Levels of anti-hnRNPA2B1 elevated in sera from keloid patients and healthy controls. The anti-hnRNPA2B1 levels in sera from patients with keloid were significantly higher than that found in normal controls tested by ELISA. Each symbol represents one subject. KS, sera from patients with keloid; NS, sera from normal controls
Discussion
Many studies have focused on the immune response of keloid formation [17, 18]. Although some serum complements and immunoglobulins were found higher in keloid patients than that in nonkeloid patients [19, 20], these complements and immunoglobulins also can change in different inflammatory and tumor diseases, and are not specific for autoimmune diseases. Besides, there were also other studies that reported the levels of serum immunoglobulin and complement were normal in keloid patients [21, 22]. Thus, keloid has been considered to be associated with immune reactivity, not with autoimmune reactivity. Few studies have regarded keloid as an autoimmune disease. In 1979, Yagi et al. [23] proposed that keloids might be related to an immune reaction to some antigenic components of sebum secreted from cut or damaged sebaceous glands and ducts. In 1982, Janssen de Limpens et al. [24] reported the presence of autoantibodies in lymphocyte eluates, but not in sera, from patients with keloid. However, there is no report showing that autoantibodies against specific autoantigens in sera from keloid patients were detected. Our study demonstrated that the anti-hnRNPA2B1 titer was elevated in sera from keloid patients and IC deposits were detected in keloid tissues, suggesting that keloid was mediated by autoimmune responses and has similar characteristics with autoimmune diseases.
hnRNPA2B1 belongs to heterogeneous nuclear ribonucleoproteins (hnRNPs) with a predominantly nuclear localization and playing important roles in precursor mRNA processing [25]. A growing number of autoantibodies to RNA-associated proteins have been indentified in autoimmune diseases, representing valuable tools for their diagnosis and prognosis. HnRNP A2, hnRNP B1, and hnRNP B2 are alternatively spliced variants generated from a single gene and anti-hnRNPA2B1 antibody targets these three variants [26]. In 1988, Dangli et al. [27] documented SLE sera containing anti-hnRNP autoantibodies that specifically reacted with cellular hnRNP A2, B1, and B2. Anti-hnRNPA2B1 was also detected in other autoimmune diseases, such as RA, mixed connective tissue disease and Sjögren’s syndrome [28]. Recently, anti-hnRNPA2B1 was detected in sera from patients with SD [29]. In the current study, we firstly observed significantly elevated anti-hnRNPA2B1 levels in sera from patients with keloid. Although we also detected other anti-hnRNP in preliminary experiments, such as anti-hnRNP I, no difference between sera from keloid patients and healthy controls was found. Anti-hnRNPA2B1 might be a diagnostic and screening tool for keloid patients, for example, to assess keloid susceptible individuals before surgery in the future.
ANAs occur frequently in sera from patients with a wide variety of autoimmune diseases, including SLE, SD, RA, and mixed connective tissue disease [30, 31]. In addition, certain autoantibodies are strictly associated with certain disease states, such as anti-PCNA and anti-Sm in SLE, Jo-1 in polymyositis, and ACA and Scl-70 in SD [30]. In the study, we also screened routine ANA profiles in sera from keloid patients and found that while a few patients were positive for ANAs, the incidence was negligible.
ICs are formed from the integral binding of immunoglobulins (antibodies) to soluble antigens. IC deposits in tissues underlie the pathogenesis of a range of autoimmune diseases from glomerulonephritis, SLE, arthritis, and transplantation rejection to rheumatic fever [16]. In autoimmune diseases, immunoglobulin deposition is frequently accompanied by complement deposition, such as the formation of IgG and C3 deposits at the basement membrane of pancreatic ducts in autoimmune pancreatitis and IgA, IgM, and C3 deposition in cutaneous vessels in dermatitis herpetiformis [8, 32]. In the present study, depositions of immunoglobulins IgA and IgM, as well as complement proteins C1q and C3 were observed in keloid tissues, which suggest that keloid might be a skin disease mediated by ICs that are similar to those that occur in other autoimmune diseases.
Immune cell infiltration is another hallmark of keloid pathology [4, 33–35] that can be attributed in part to IC deposits [16]. Surprisingly, the infiltration of CD20+ B lymphocytes in keloid tissues was more obvious than that of other immune cells. An increasing body of evidence suggests that B lymphocytes are critical in the development of autoimmune disease, even in certain diseases that were initially thought to be B cell independent [36]. For example, in a transgenic mouse model of RA, a disease initially was thought to be mediated by T cells; the pathogenic role of IgG arthritogenic antibodies was confirmed even in the absence of T cells [37]. Recently, B cell depletion with a CD20 antibody was found to be effective in autoimmune diseases and rituximab, a chimeric monoclonal antibody against CD20, was licensed in 2006 for the treatment of RA [38]. Since then, interest in B-cell targeted therapies has increased significantly and a number of new B cell-targeting therapies are now in clinical development [39]. B cell depletion strategies could thus provide new avenues for the treatment of keloids.
Conclusion
This study examined immune cell infiltration and IC deposition in keloid lesions, as well as autoantibodies in keloid patient sera. The results showed increased numbers of infiltrating immune cells and IC deposition in lesional tissue and increased titers of anti-hnRNPA2B1 in keloid patient sera, which together support the possibility that keloid is a skin fibrosis disease mediated by autoimmune responses. A future study involving a larger number of cases is needed to determine whether anti-hnRNPA2B1 could provide new approaches for the prediction, diagnosis, and prognosis of keloids.
References
Bran GM, Goessler UR, Hormann K, Riedel F, Sadick H (2009) Keloids: current concepts of pathogenesis (review). Int J Mol Med 24:283–293
Bayat A, McGrouther DA, Ferguson MW (2003) Skin scarring. BMJ 326:88–92
Brown BC, McKenna SP, Siddhi K, McGrouther DA, Bayat A (2008) The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg 61:1049–1058
Bagabir R, Byers RJ, Chaudhry IH, Muller W, Paus R, Bayat A (2012) Site-specific immunophenotyping of keloid disease demonstrates immune upregulation and the presence of lymphoid aggregates. Br J Dermatol 167:1053–1066
Verhaegen PD, van Zuijlen PP, Pennings NM, van Marle J, Niessen FB, van der Horst CM, Middelkoop E (2009) Differences in collagen architecture between keloid, hypertrophic scar, normotrophic scar, and normal skin: an objective histopathological analysis. Wound Repair Regen 17:649–656
Kisseleva T, Brenner DA (2008) Mechanisms of fibrogenesis. Exp Biol Med (Maywood) 233:109–122
Stramer BM, Mori R, Martin P (2007) The inflammation-fibrosis link? A Jekyll and Hyde role for blood cells during wound repair. J Invest Dermatol 127:1009–1017
Detlefsen S, Brasen JH, Zamboni G, Capelli P, Kloppel G (2010) Deposition of complement C3c, immunoglobulin (Ig)G4 and IgG at the basement membrane of pancreatic ducts and acini in autoimmune pancreatitis. Histopathology 57:825–835
Peterson LS, Nelson AM, Su WP (1995) Classification of morphea (localized scleroderma). Mayo Clin Proc 70:1068–1076
Denton CP, Black CM, Abraham DJ (2006) Mechanisms and consequences of fibrosis in systemic sclerosis. Nat Clin Pract Rheumatol 2:134–144
Butler PD, Longaker MT, Yang GP (2008) Current progress in keloid research and treatment. J Am Coll Surg 206:731–741
Huo AP, Lin KC, Chou CT (2010) Predictive and prognostic value of antinuclear antibodies and rheumatoid factor in primary Sjogren’s syndrome. Int J Rheum Dis 13:39–47
De Rycke L, Baeten D, Kruithof E, Van den Bosch F, Veys EM, De Keyser F (2005) The effect of TNFalpha blockade on the antinuclear antibody profile in patients with chronic arthritis: biological and clinical implications. Lupus 14:931–937
Marin GG, Cardiel MH, Cornejo H, Viveros ME (2009) Prevalence of antinuclear antibodies in 3 groups of healthy individuals: blood donors, hospital personnel, and relatives of patients with autoimmune diseases. J Clin Rheumatol 15:325–329
Pisetsky DS (2011) Antinuclear antibodies in healthy people: the tip of autoimmunity’s iceberg? Arthritis Res Ther 13:109
Mayadas TN, Tsokos GC, Tsuboi N (2009) Mechanisms of immune complex-mediated neutrophil recruitment and tissue injury. Circulation 120:2012–2024
McCarty SM, Syed F, Bayat A (2010) Influence of the human leukocyte antigen complex on the development of cutaneous fibrosis: an immunogenetic perspective. Acta Derm Venereol 90:563–574
Seifert O, Mrowietz U (2009) Keloid scarring: bench and bedside. Arch Dermatol Res 301:259–272
Kazeem AA (1988) The immunological aspects of keloid tumor formation. J Surg Oncol 38:16–18
Bloch EF, Hall MG Jr, Denson MJ, Slay-Solomon V (1984) General immune reactivity in keloid patients. Plast Reconstr Surg 73:448–451
Cohen IK, McCoy BJ, Mohanakumar T, Diegelmann RF (1979) Immunoglobulin, complement, and histocompatibility antigen studies in keloid patients. Plast Reconstr Surg 63:689–695
Kischer CW, Shetlar MR, Shetlar CL, Chvapil M (1983) Immunoglobulins in hypertrophic scars and keloids. Plast Reconstr Surg 71:821–825
Yagi KI, Dafalla AA, Osman AA (1979) Does an immune reaction to sebum in wounds cause keloid scars? Beneficial effect of desensitisation. Br J Plast Surg 32:223–225
Janssen de Limpens AM, Cormane RH (1982) Keloids and hypertrophic scars–immunological aspects. Aesthetic Plast Surg 6:149–152
Dreyfuss G, Matunis MJ, Pinol-Roma S, Burd CG (1993) hnRNP proteins and the biogenesis of mRNA. Annu Rev Biochem 62:289–321
Caporali R, Bugatti S, Bruschi E, Cavagna L, Montecucco C (2005) Autoantibodies to heterogeneous nuclear ribonucleoproteins. Autoimmunity 38:25–32
Dangli A, Guialis A, Vretou E, Sekeris CE (1988) Autoantibodies to the core proteins of hnRNPs. FEBS Lett 231:118–124
Hassfeld W, Steiner G, Hartmuth K, Kolarz G, Scherak O, Graninger W, Thumb N, Smolen JS (1989) Demonstration of a new antinuclear antibody (anti-RA33) that is highly specific for rheumatoid arthritis. Arthritis Rheum 32:1515–1520
Siapka S, Patrinou-Georgoula M, Vlachoyiannopoulos PG, Guialis A (2007) Multiple specificities of autoantibodies against hnRNP A/B proteins in systemic rheumatic diseases and hnRNP L as an associated novel autoantigen. Autoimmunity 40:223–233
Neri R, Tavoni A, Cristofani R, Levanti C, Sodini G, d’Ascanio A, Vitali C, Ferri C, Bombardieri S (1992) Antinuclear antibody profile in Italian patients with connective tissue diseases. Lupus 1:221–227
Guevara-Gutierrez E, Yinh-Lao J, Garcia-Gutierrez P, Tlacuilo-Parra A (2010) Frequency of antinuclear antibodies in mestizo Mexican children with morphea. Clin Rheumatol 29:1055–1059
Preisz K, Sardy M, Horvath A, Karpati S (2005) Immunoglobulin, complement and epidermal transglutaminase deposition in the cutaneous vessels in dermatitis herpetiformis. J Eur Acad Dermatol Venereol 19:74–79
Shaker SA, Ayuob NN, Hajrah NH (2011) Cell talk: a phenomenon observed in the keloid scar by immunohistochemical study. Appl Immunohistochem Mol Morphol 19:153–159
Onodera M, Ueno M, Ito O, Suzuki S, Igawa HH, Sakamoto H (2007) Factor XIIIa-positive dermal dendritic cells in keloids and hypertrophic and mature scars. Pathol Int 57:337–342
Boyce DE, Ciampolini J, Ruge F, Murison MS, Harding KG (2001) Inflammatory-cell subpopulations in keloid scars. Br J Plast Surg 54:511–516
Lim PL, Zouali M (2006) Pathogenic autoantibodies: emerging insights into tissue injury. Immunol Lett 103:17–26
Benoist C, Mathis D (2000) A revival of the B cell paradigm for rheumatoid arthritis pathogenesis? Arthritis Res 2:90–94
Leandro MJ (2013) B-cell subpopulations in humans and their differential susceptibility to depletion with anti-CD20 monoclonal antibodies. Arthritis Res Ther 15(Suppl 1):S3
Bluml S, McKeever K, Ettinger R, Smolen J, Herbst R (2013) B-cell targeted therapeutics in clinical development. Arthritis Res Ther 15(Suppl 1):S4
Acknowledgments
This study was funded by National Natural Science Foundation of China (30871433, 31071305).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Jiao, H., Fan, J., Cai, J. et al. Analysis of Characteristics Similar to Autoimmune Disease in Keloid Patients. Aesth Plast Surg 39, 818–825 (2015). https://doi.org/10.1007/s00266-015-0542-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-015-0542-4