Abstract
Background
The aim of this study is to analyze scientifically the results of a rhinoplasty is a difficult task because of the multiplicity of surgical procedures and the subjective nature of the nose’s beauty. Nevertheless, we wanted to evaluate open rhinoplasty by relying on objective and subjective criteria.
Methods
From 2004 to 2011, a total of 155 patients underwent open septorhinoplasty at our hospital. After excluding patients lost to follow-up and those who underwent orthognathic surgery, 55 patients were included in the study. The evaluation was based on the clinical record, the standardized photographs, and the consultation of control. We studied in particular the nasolabial angle (NLA), the Goode ratio (projection/length of nose), and patient satisfaction using the rhinoplasty outcome evaluation form.
Results
The columella–transalar incision tended to close the NLA (p = 0.001) and lowered the Goode ratio (p = 0.01), in contrast to the Réthi incision. The resection of the alar cartilages logically induced closure of the NLA (p = 0.02) and a decrease of nose projection (p = 0.001), whereas the use of a columellar strut induced a projection increase (p = 0.01).
Conclusion
Despite the existence of unavoidable measures bias, we confirmed a number of assumptions that had never been demonstrated statistically. Furthermore, we found that the incision used could affect the final result of a rhinoplasty.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The past century has seen the emergence and rapid development of new surgical techniques. Since the 1920s, many teams of plastic and maxillofacial surgeons have been interested in rhinoplasty, a surgical technique used to beautify the nose or to correct congenital defects or defects secondary to trauma [1–3].
The study of patient satisfaction after rhinoplasty remains a rather neglected area of research with few validated measurement tools [1–3]. It seems impossible to define the ideal nose; however, the surgeon as the artist cannot rely on his instinct alone to complete his work, he must submit to certain geometric measurements [4]. Indeed, beauty is not just a personal impression, it must meet a wide approval and lies in the accuracy of proportions despite the diversity of the human species. The aim of this study was to identify in the medical literature the most reliable objective and subjective means to scientifically evaluate the results of a rhinoplasty. Then we tried to compare different surgical procedures to better understand and anticipate the changes in the final appearance of the operated nose.
Materials and Methods
Patient Cohort
This is a retrospective study that included all patients who underwent an open septorhinoplasty between January 2004 and December 2011. Medical records allowed us to study the operative reports, the hospitalization reports, and pre- and postoperative photographs. To avoid selection bias, all patients who had associated surgical procedures in areas other than the nose that may have altered the results of the septorhinoplasty, e.g., maxillary osteotomy or upper-lip surgery, were excluded.
Data Collection
For each patient included in the study, epidemiological data (i.e., age, sex, duration of monitoring, and etiology) and the various surgical procedures performed during surgery (e.g., septoplasty, osteotomies, bump reduction, and tip modifications) were reported. Patients were contacted by telephone and invited to come for a consultation. They were met by the same observer who conducted a functional and aesthetic clinical examination and took standardized photographs, including face on, right profile, left profile, head back, three-quarter right and three-quarter left.
Rhinoplasty Evaluation Criteria
Each patient was evaluated by objective and subjective criteria. These criteria were selected by two independent sources. We searched through the PubMed in Medline databases for evaluation techniques of rhinoplasty results cited between 1960 and 2010, a date range recommended by Poynard et al. [5] who consider that the duration of a technical life in medicine is 50 years. No specific keywords were found using the index of keywords, MeSH (Medical Subjects Headings). Techniques for evaluating rhinoplasty results were identified from two empirical sources, as was the case in another study [6]. The first source was 50 publications between 1960 and 2010 found in PubMed by searching with the keyword “rhinoplasty outcome evaluation (ROE).” Of these 50, only 7 dealt with assessment techniques for rhinoplasty. From these seven articles we identified seven keywords: “nasolabial angle (NLA)” (6 times), “ROE” (4 times), “Goode ratio (GR)” (3 times), “nasofrontal angle” (2 times), “SF36 Questionnaire”(1 time), “visual analog scale of quality of life” (1), and “Vancouver scar scale” (1 time). The second source was a survey conducted of ten surgeons who regularly perform rhinoplasty. We asked them to tell us the keywords they would use to search for articles in PubMed on how to evaluate rhinoplasty results. They gave five keywords: “NLA” (5 times), “ROE” (4 times), “nasofacial angle” (3 times), “GR” (3 times), and “scar assessment” (2 times).
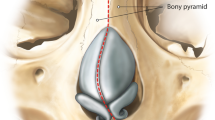
We chose the four common keywords from both sources and obtained two objective criteria and two subjective criteria. The objective criteria were (1) pre- and postoperative measurements of the NLA (Fig. 1) and (2) pre- and postoperative measurements of the GR (Fig. 2). The subjective criteria were (1) the evaluation of the pre- and postoperative satisfaction of the patient through a standardized questionnaire: the ROE, and (2) the scar assessment by patients themselves.
Measurement of Nasolabial Angle
The NLA is defined as the angle between the upper lip and columella (Fig. 1). Fitzgerald and Nanda [7] were the first to define the standards of NLA in the Caucasian population in 1992. The NLA is 105° [8] but it can range from 90° to 120°.
Measurement of Goode Ratio
The GR [9–11] is based on a trigonometric analysis of the dimensions of the entire nose (Fig. 2). A nose with a normal projection has a GR between 0.55 and 0.6. The ideal GR is 0.59 [12].
Measurement of Nose-specific Quality of Life with the ROE
The quantitative evaluation of pre- and postoperative quality of life has been a standard in medicine, including surgery, for a decade [3, 13, 14]. Alsarraf et al. [2, 15] were the first to introduce and test a consistently reliable tool for assessing outcomes of facial plastic surgery, including rhinoplasty. The ROE tool is a standardized questionnaire used to quantitatively measure the quality of life of patients who underwent rhinoplasty. This questionnaire consists of six questions covering three areas of quality of life: physical, emotional, and social. Each question is scored from 0 to 4. The score is reported on a scale of 0–100 [16] and the results are categorized as follows: 0–25 and 25–50 = failure of the procedure, 50–75 = good result, and 75–100 = excellent result. In our study, the ROE questionnaire was used twice during the same visit to measure pre- and postoperative patient satisfaction.
Evaluation of Incision Sequelae: Scar Score
The Vancouver scar scale does not apply here because of the small size of the scar and the scale does not properly assess inflammation and pigmentation [17]. Thus, we developed a simple rating scale to characterize the columellar scar: 0 = invisible scar, 1 = slightly visible scar, and 2 = very visible scar. The scar was assessed by the patient after the observer had explained the rating scale. We took into account only the rating of the patient, as recommended by several authors, because of the subjective nature of the data [14].
Comparability of Incision Subgroups and Statistical Analysis
For our three evaluation criteria (NLA, GR, and ROE), we held that the two incision subgroups analyzed each time were comparable (not statistically different) because of the comparison of preoperative epidemiological data (age, sex ratio, and follow-up) and surgical intraoperative data (osteotomies, septoplasties, tip work). Epidemiological data, preoperative data, and evaluation criteria were compared using nonparametric χ2 and Mann–Whitney statistical tests. We also used the biostatistics software R. Our results were checked by a hospital statistician.
All patients were informed about the study’s purpose and signed a consent form.
Results
Of the 155 patients who underwent a rhinoplasty at our hospital between January 2004 and December 2011, a total of 28 patients were excluded because their file was incomplete, 38 patients were excluded because associated surgical procedures were performed, including lip cleft palate and orthognathic surgery, which could affect the rhinoplasty evaluation, and 34 patients were lost to follow-up. Finally, 55 patients (39 women and 16 men) were reviewed during consultation and selected for our study. The average age of patients at surgery was 31.6 years (range = 16–67). The average age at the time of the study was 35.7 years. The average follow-up time since surgery was 4.2 years. Of the 55 rhinoplasties, 18 were post-traumatic, 16 were aesthetic, 7 were functional, 9 were included in a malformation syndrome, and 5 were secondary.
Seven different surgeons were identified: six used the Réthi incision (Fig. 3) and one used the columella–transalar incision (CT) exclusively (Fig. 4) [18]. The CT incision tended to close the NLA (p = 0.001) and lower the GR (p = 0.01) (Fig. 5), in contrast to Réthi incision (Table 1; Fig. 6). The interrupting resection of the alar cartilages tended to close the NLA (p = 0.02) and lower the GR (p = 0.001) (Table 2). The columellar strut increased the GR (p = 0.001) (Table 3). Thus, two parameters alter the NLA: the incision and the interrupting resection of alar cartilages. The Réthi incision favored the opening of the NLA and the CT incision favored the closing of the NLA. The interrupting resection of the alar cartilages logically was accompanied by a closing of the NLA.
We found that three elements influence the projection of the nose: the incision, the interrupting resection of the alar cartilages, and the columellar strut. The Réthi incision was associated with an increase in the projection of the nose, whereas the CT incision was accompanied by a reduction of this projection. Resection of alar cartilages caused a decrease in the GR, whereas the columellar strut increased it.
Discussion
Evaluating scientifically the results of a rhinoplasty is a very complex task due to the multitude of surgical procedures available and the total lack of consensus on tools to assess results, as evidenced by the poor medical literature on the subject. The use of a validated satisfaction questionnaire helped us standardize the assessment of patient satisfaction and to compare the different techniques used. However, the evaluation of preoperative satisfaction (ROE) was performed retrospectively at the consultation visit. This approach is a measurement bias because preoperative satisfaction is analyzed a long time after the procedure and the procedure may have altered the patient’s judgment. Nevertheless, it was the only way to get a reference point of satisfaction in a retrospective study. Other authors also used this approach in their studies [19].
It is interesting to note that all objective evaluation criteria are measured using the profile view of the nose because photographs of the face straight on cannot be used for an accurate assessment of the proportions of a nose, as highlighted by Polselli et al. [20]. According to those authors, evaluating the nose from the front is based on morphological criteria of beauty and if the shape of the tip of the nose and the nostrils are in harmony with the face. Despite a methodology based on a literature review and a survey of experimented surgeons, we cannot be sure that we have selected the best criteria for rhinoplasty evaluation. We chose some of the measures described by Powell and Humphries [21] because they are frequently used in the literature. Another moot point is the use of an “ideal” reference for each parameter [8]. The ideal is often defined as a range of values but we used unique values to simplify statistical analysis.
The amount of septum resected at each rhinoplasty was not taken into account because it was not specified in the operating notes. This limits finer analysis of the projection and the NLA. In addition, we were not able to study the effect of suturing the triangular and alar cartilages to the septum because the procedure is surgeon-dependent and there is a lack of detail in operation reports.
The Incision
The Réthi incision contributes to opening the NLA by +4.2° on average, whereas the CT incision tends to close it by −6.4° on average. This result is very interesting because usually the incision is not considered a therapeutic gesture in rhinoplasty. In addition to allowing access to deep structures of the nose, it seems that the incision has a real effect on the final outcome of a septorhinoplasty. We hypothesize that CT incisions close the NLA because the scar retracts the soft tissue and alar cartilages at the base of the columella. Postoperatively, the GR increased 0.03 on average in the Réthi group and decreased 0.05 on average in the CT group, with a statistically significant difference between the two (p = 0.02). This result suggests that the Réthi incision could contribute to increasing the projection of the nose whereas the CT incision could decrease it. We found no difference in patient satisfaction between the two incision groups (p = 0.34). In conclusion, the two incisions appear to have opposite effects on the morphology of the nose profile, with the CT incision tending to close the NLA and lower the Goode index.
Interrupting Resection of Alar Cartilages
Postoperatively, the NLA decreased an average of −4.1° in those patients who underwent interrupting resection of the alar and it decreased an average of −0.9° in those who did not undergo interrupting resection of the alar (p = 0.02). In addition, the GR decreased an average of 0.05 in those patients who underwent a resection of the alar and decreased an average of 0.01 those who did not have alar resection (p = 0.001). It can therefore be argued that interrupting alar resection contributes to the closure of the NLA and lowers the projection of the nose. Few works have studied the effect of alar resection on the NLA. We found only one [22], which claimed that a 20 % interrupting resection of alar cartilages would result in an average decrease in the NLA of 2.6°. However, comparing this value with our results must be done with caution because the authors did not specify exactly where the alar was resected and once again the reproducibility of this surgery and its consequences are difficult to assess.
Columellar Strut
In our series, the columellar strut did not significantly influence the NLA. However, it changes the projection of the nose after rhinoplasty. The GR increased 0.03 in those patients who got a columellar strut and decreased 0.02 in those who did not (p = 0.01). The columellar strut therefore helps to maintain or increase the projection of the nose but in less so than we imagined. The actual role of the columellar strut would be more to maintain the projection, fighting against a secondary collapse or excessive scar retraction, rather than increase it. Two recent studies confirm our results. Akkus and Guneren [23] demonstrated in a prospective study of 36 patients that the columellar strut increases nasal projection. Carron and Pastorek [24], in their retrospective study of 15 patients, concluded that the columellar strut induces an increase in projection of 15 % (p < 0.05). However, little information is provided on the size of the grafts used and their implementation, which further limits the power of these findings and their applicability in the operating room.
Thus, we found that two parameters statistically alter the NLA: the incision and interrupting resection of alar cartilages. The Réthi incision contributed to the opening of the NLA (+4.2° on average), unlike the CT incision which tended to close it (−6.4° on average) (p = 0.001). Postoperatively, the NLA was more closed in patients who had undergone interrupting resection of alar cartilages: 100.5° versus 104.3° (p = 0.01). We also found that three factors influence the projection of the nose: the incision, the interrupting resection of alar cartilages, and the columellar strut. The Réthi incision was associated with an increase in the projection of the nose (GR increased 0.03 on average), whereas the CT incision was accompanied by a reduction of the projection (GR decreased 0.05 on average) (p = 0.02). Resection of alar cartilages caused a decrease in the GR of 0.05 (p = 0.001), whereas the columellar strut increased it by 0.03 (p = 0.01).
Despite all our precautions to eliminate bias, the conclusions of our work are questionable for several reasons. In this series, seven different surgeons performed the operations. The amount of septum resected for each patient was not known. Finally, how the alar and the triangular cartilages between them and the septum were fixed is an important factor that was not possible to study in a systematic way.
Despite these biases, we highlight issues that may affect the projection of the nose and the NLA. The CT incision deserves a particular place in our armamentarium because it tends to reduce the projection of the nose and to close the NLA.
References
Anderson JR, Johnson CM Jr, Adamson P (1982) Open rhinoplasty: an assessment. Otolaryngol Head Neck Surg 90:272–274
Alsarraf R, Anderson S, Murakami CS, Johnson CM Jr (2001) Measuring cosmetic facial plastic surgery outcomes: a pilot study. Arch Facial Plast Surg 3(3):198–201
Bergman S, Feldman LS, Barkun JS (2006) Evaluating surgical outcomes. Surg Clin North Am 86:129–149
Baud C (1978) Harmonie d un visage: étude scientifique de la beauté, appliquée en chirurgie esthétique. Maloine, Paris
Poynard T, Munteanu M, Ratziu V, Benhamou Y, Di Martino V, Taieb J, Opolon P (2002) Truth survival in clinical research: an evidence-based requiem? Ann Intern Med 136:888–895
Abbou R, Beck M, Zemirline A, Facca S, Liverneaux P (2011) Techniques of peripheral nerves repair: evolution of the literature from 1950 to 2010. Chir Main 30(36):363–367 (article in French)
Fitzgerald JP, Nanda RS, Currier GF (1992) An evaluation of the nasolabial angle and the relative inclinations of the nose and upper lip. Am J Orthod Dentofacial Orthop 102:328–334
Mahajan AY, Marcus BC (2009) Analysis of patient-determined preoperative computer imaging. Arch Facial Plast Surg 11(15):290–295
Armijo BS, Brown M, Guyuron B (2012) Defining the ideal nasolabial angle. Plast Reconstr Surg 129:759–764
Goode R (1984) Personal communications. In: Powell N, Humphrey B (eds) Proportions of the aesthetic face. Thieme Medical Publishing, New York, p 72
Crumley R, Lanser M (1988) Quantitative analysis of nasal tip projection. Laryngoscope 98:202–208
Sporri S, Simmen D, Briner HR, Jones N (2004) Objective assessment of tip projection and the nasolabial angle in rhinoplasty. Arch Facial Plast Surg 6:295–298 discussion 299–300
Patrick DL (1993) Health status and health policy: quality of life in health care evaluation and resource allocation. Oxford University Press, New York
Rhee JS, McMullin BT (2008) Measuring outcomes in facial plastic surgery: a decade of progress. Curr Opin Otolaryngol Head Neck Surg 16:387–393
Alsarraf R (2000) Outcomes research in facial plastic surgery: a review and new directions. Aesthetic Plast Surg 24(23):192–197
Faidiga GB, Silveira F, Lago T, Leite MG, Anselmo-Lima WT (2010) Long-term evaluation in aesthetic rhinoplasty in an academic referral center. Braz J Otorhinolaryngol 76(74):437–441
Baryza MJ (1995) The Vancouver scar scale: an administration tool and its interrater reliability. J Burn Rehabil 16(15):535–538
Wilk A, Herman D, Rodier-Bruant C, Kolbe R, Chekkoury H, Lesage F (1992) Mini-forum: rhinoplasty by external approach. Collumello-trans-alar approach of open rhinoplasty: advantages. Ann Chir Plast Esthet 37(5):479–487 (article in French)
Izu SC, Kosugi EM, Brandao KV (2012) Normal values for the rhinoplasty outcome evaluation (ROE) questionnaire. Braz J Otorhinolaryngol 78:76–79
Polselli R, Saban Y (2007) Artistic anatomy of the nose: proposals for a simplified project of rhinoplasty. Rev Laryngol Otol Rhinol (Bord) 128(4):239–242 (article in French)
Powell N, Humphries B (1984) Proportions of the aesthetic face. Thieme Medical Publishing, New York, p 72
Hazani R, Rao AJ, Wilhelmi BJ (2013) Caudal resection of the upper lateral cartilages and its measured effect on tip rotation. Ann Plast Surg 71(5):450–452
Akkus AM, Guneren E (2013) Comparison of the effects of columellar strut and septal extension grafts for tip support in rhinoplasty. Aesthetic Plast Surg 37(4):666–673
Carron MA, Pastorek NJ (2013) Measured gain in projection with the extended columellar strut-tip graft in endonasal rhinoplasty. JAMA Facial Plast Surg 15(13):187–191
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abbou, R., Bruant-Rodier, C., Wilk, A. et al. Open Rhinoplasty: Influence of Incisions, Alar Resection, and Columellar Strut on Final Appearance of the Tip. Aesth Plast Surg 38, 1077–1082 (2014). https://doi.org/10.1007/s00266-014-0395-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-014-0395-2