Abstract
Purpose
This study aims to assess the impact of repairing the hip joint capsule during posterior-lateral approach total hip arthroplasty (THA) on postoperative hip joint function and late dislocation incidence.
Methods
A retrospective cohort study included 413 patients, divided into experimental (hip joint capsule repair, n = 204) and control (hip joint capsule excision, n = 209) groups. Patients were followed for five years, evaluating postoperative hip range of motion (ROM), dislocation rate, VAS and HHS scores, inflammatory and coagulation markers, hospitalization, blood loss, and body composition. Statistical analysis included the Student’s t-test, Chi-square test, and logistic regression for dislocation risk factors.
Results
Joint capsule repair improved postoperative hip flexion and extension within six months and at two years postoperatively, internal and external rotation within three months, and abduction and adduction throughout the entire follow-up period (P < 0.05). Capsular repair also reduced early and late dislocation rates (P < 0.05). Significant differences in HHS and VAS scores, inflammatory and coagulation indicators, hospitalization, blood loss, and body composition were noted (P < 0.05). Multivariate logistic regression indicated hip joint repair, rheumatoid arthritis, epilepsy, and sarcopenia as dislocation risk factors (P < 0.05).
Conclusions
Capsular repair during posterior-lateral THA improves postoperative hip function and mobility while reducing dislocation rates, blood loss, pain, inflammation, and economic burden. Patients with rheumatoid arthritis, epilepsy, or sarcopenia require individualized planning and enhanced postoperative care to minimize complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is regarded as the most effective treatment for various end-stage hip joint diseases and is hailed as one of the most successful surgeries of the 20th century. Currently, in the United States, 116 individuals per 100,000 undergo THA, with an estimated population of 635,000 individuals expected to have undergone THA by 2030 [1]. THA is an effective method for alleviating hip pain, maintaining hip stability, and restoring functional hip motion [2].
The posterior-lateral approach is the most common surgical approach employed in THA. It is characterized by its technical simplicity, versatility, excellent exposure, reduced incidence of ectopic ossification, and preservation of abductor muscle strength [3]. However, its primary drawback, as reported, is the occurrence of early postoperative dislocation, with an incidence ranging from 1 to 9% [4]. Reasons for early dislocation may include lack of patient compliance, insufficient capsule support, abductor muscle laxity, bone or prosthesis impingement, eccentricity mismatch, and component malposition [5]. Studies have indicated that the direct-lateral or anterior-lateral approaches have lower dislocation rates compared to the posterior-lateral approach, possibly due to the preservation of normal joint capsule structure [6]. Previous research has demonstrated that hip capsule repair can effectively reduce the early dislocation rate following THA [3, 4, 7]. In the extended position, the posterior-lateral approach results in a smaller increase in range of motion (ROM) compared to the anterolateral approach. The ultimate goal for patients is to restore normal hip joint function through THA. Preserving the hip joint capsule may protect against hypermobility and associated adverse loading following arthroplasty [8]. This could be a beneficial factor for patients to smoothly engage in early postoperative rehabilitation exercises and improve joint mobility.
However, there is currently no evidence demonstrating whether hip capsule repair has a beneficial impact on postoperative range of motion for the hip joint in patients undergoing THA or whether it reduces the occurrence of late dislocation after surgery. A retrospective cohort study was conducted over a period of five years to compare the effects of complete hip capsule excision with hip capsule repair on patients undergoing THA.
Methods
Study design and ethical review
We retrospectively collected clinical data from patients who underwent THA at our center from January 2014 to January 2019. This study was approved by the ethics committee of our institution and registered with a unique identification number. (Research Registration Number: 2023-KLS-130-01)
Inclusion and exclusion criteria
Inclusion criteria: (1) patients undergoing their initial THA at our center; (2) patients voluntarily participating in this study and providing signed informed consent; (3) age > 18 years. Exclusion criteria: (1) concurrent haematologic disorders such as thrombocytopenia, haemophilia, etc.; (2) concurrent malignancies.
Data collection
All medical records and examination results were collected by a single physician from our electronic medical records system, with follow-ups conducted by the same physician. Another senior physician reviewed and confirmed the accuracy of the data. Recorded information included: age, height, weight, body mass index (BMI), medical history, hospital stay duration, surgery duration, preoperative haematocrit (HCT), hip ROM, harris hip score (HHS) score, visual analog scale (VAS) score, total blood loss (TBL), visible blood loss (VBL), occult blood loss (OBL), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), activated partial thromboplastin (APTT), d-dimer, erythrocyte count, haemoglobin (HB) level, and albumin level.
Potential complications included hip dislocation, deep venous thrombosis (DVT), pulmonary embolism (PE), and postoperative infection. Doppler ultrasound was used to check for the DVT and PE.
The calculation for total blood loss involves the Eq. [9]: Preoperative blood volume (PBV) * (Preoperative HCT – Postoperative HCT)/ (Preoperative HCT + Postoperative HCT) * 2. PBV = k1 * height (m) 3 + k2 * weight (kg) + k3 (male: k1 = 0.3669, k2 = 0.03219, k3 = 0.6041; female: k1 = 0.3561, k2 = 0.03308, k3 = 0.1833). OBL = TBL – VBL.
ROM measurement: ROM (flexion-extension): The patient is positioned in the supine position. Goniometer placement: The fulcrum is positioned at the lateral aspect of the greater trochanter. The stationary arm points towards the lateral aspect of the pelvis, while the moving arm is aligned parallel to the long axis of the femur. ROM (internal-external rotation): The patient is positioned in the supine position. Goniometer placement: The fulcrum is located at the midpoint of the tibial plateau, with both the stationary arm and the moving arm aligned parallel to the long axis of the tibia. When the hip rotates internally, the stationary arm remains in its original position, perpendicular to the ground, while the moving arm follows the movement of the tibia. ROM (abduction-adduction): The patient is positioned in the supine position. Goniometer placement: The fulcrum is located at the anterior superior iliac spine. The stationary arm aligns with the line connecting both the anterior and superior iliac spines, while the moving arm is parallel to the long axis of the femur. Measurements were conducted by two orthopaedic doctors, and the consistency of the results was examined through Cronbach’s alpha test.
Perioperative management and operation method
All surgeries were performed by the same senior surgeon from our team. All patients underwent a posterior-lateral surgical approach. After anaesthesia induction, positioning adjustments, and surgical site sterilization, the skin, subcutaneous tissue, and fascia were incised. Blunt dissection of the gluteus maximus muscle was performed, followed by entry along the intermuscular plane and partial detachment of the external rotator muscles near their insertions. A “T”-shaped incision in the joint capsule exposed the hip joint. The hip joint was dislocated, and the femur was osteotomized approximately 1.5 cm from the trochanteric tip. The femoral head was then removed, and any osteophytes and synovial tissue around the acetabulum were cleared. The tear was identified, and the acetabulum was reamed to the appropriate position at 45° abduction and 15° anteversion, followed by the insertion of a polyethylene liner. The proximal femur was exposed, and the medullary canal was widened in a 15° anteversion direction for the implantation of a biological femoral stem. A short neck and ceramic head were installed, and the hip joint was reduced. In the experimental group, the hip joint capsule was preserved. After the joint was repositioned, non-absorbable sutures were used to stitch the ends of the capsule together. A 2 mm drill was then used to create a hole in the greater trochanter, through which the capsule and the piriformis tendon were reattached to the posterior edge of the greater trochanter. In the control group, the posterior hip joint capsule was removed, but all other steps were the same as in the experimental group (Fig. 1) (Fig. 2).
Surgical procedure. a: The patient was assumed with a lateral decubitus position. The incision of the posterior-lateral approach was labelled on the skin; b: Exposing the joint capsule. The tissue grasped by the hemostatic forceps in the figure is the joint capsule; c: Repair of the posterior moscle and capsule flaps; d: Repair of the external rotator muscles
Both groups received the same postoperative antibiotic regimen for infection prophylaxis, along with compression stockings and pneumatic compression devices to prevent thrombosis formation. All patients started rehabilitation on postoperative day five with the same rehabilitation program.
Statistical analysis
Data analyses were conducted using SPSS 25.0 (IBM, Armonk, NY, USA). Descriptive statistics were presented as mean ± standard deviation or frequencies (percentages). Normality was assessed with the Shapiro-Wilk test. Student’s t-test and Mann-Whitney U test were used for data accordingly. Chi-square test was applied for categorical variables. Logistic regression identified factors impacting hip dislocation. A p-value < 0.05 was considered statistically significant.
Results
Patient participation and demographics
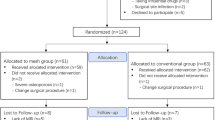
During the study, 449 patients underwent THA. Eight patients were lost to follow-up due to missing records. Six patients were lost to follow-up and considered dropouts. Twelve patients had blood disorders, and ten patients had tumour histories. Eventually, 413 patients were included and followed for up to five years. The experimental group (n = 204) had joint capsule repair, and the control group (n = 209) had capsule excision. The power analysis for both groups was 96%. Cronbach’s alpha test presented good consistency of the measurements (α > 0.75). Demographic data, including age, height, weight, BMI, medical history, and preoperative parameters, showed no significant differences between groups (P > 0.05) (Table 1).
Hip joint function and dislocation
Joint capsule repair improves postoperative hip joint ROM, notably in flexion-extension at 6 months and the second year (P < 0.05), internal-external rotation at three months (P < 0.05), and abduction-adduction throughout follow-up (P < 0.05) (Table 2).
Furthermore, it improves patients’ postoperative HHS scores at 6 months and the third year (P < 0.05). Additionally, it reduces postoperative hip joint dislocation rates, both early (within 6 months) and late (after 6 months) (P < 0.05) (Table 3).
Volume of blood loss, hospitalization and pain
Joint capsule repair reduces postoperative blood loss, with significant differences in TBL and OBL (P < 0.05), while VBL shows no significant difference (P > 0.05). It also alleviates early postoperative pain that persists within the first month (P < 0.05). Moreover, it shortens hospital stays and reduces costs (P < 0.05). Additionally, it does not prolong surgery duration (P > 0.05) (Table 3).
Inflammatory indicators and coagulation indicators
Inflammation levels were lower in the experimental group than in the control group, but CRP was statistically different between the two groups only on postoperative day seven, and ESR was statistically different between the two groups within seven days after surgery. Additionally, the experimental group exhibited shorter APTT times postoperatively, which persisted for up to seven days. At discharge, the experimental group exhibits lower d-dimer levels than the control group (Table 4).
Body composition and complications
Joint capsule repair reduces the postoperative decline in patients’ erythrocyte count, HB level, and albumin level. Significant differences in erythrocyte count were noted on the first day postoperatively, while HB levels differed significantly within four days. Albumin levels showed significant differences on the fourth day postoperatively and at discharge (Table 4). All patients remained free from DVT, PE, and infection during hospitalization.
Univariate and multivariate logistic regression
We conducted logistic regression analysis for dislocation and performed stepwise regression to screen variables including group, HB, APTT, rheumatoid arthritis, epilepsy, sarcopenia, ROM (flexion/extension), and OBL for multivariate logistic regression. The results indicated a significant correlation between hip joint capsule repair, rheumatoid arthritis, epilepsy, muscular dystrophy, and postoperative hip joint dislocation (P < 0.05) (Table 5).
Discussions
This study demonstrates that capsular repair in THA patients enhances hip mobility and function, reduces early and late dislocation rates, and mitigates postoperative pain, inflammation, and blood loss. Additionally, repairing the capsule can lead to shorter hospital stays and reduced hospitalization costs. This suggests that hip capsule repair may help patients receive high-quality rehabilitation earlier in the postoperative period, achieve better wound healing and joint function, contribute to improved patient satisfaction after surgery, and effectively prevent postoperative complications. To our knowledge, this is the first study to investigate the impact of capsular repair in posterior lateral approach THA on postoperative hip activity and late dislocation.
Hip joint mobility is a focal point of concern for us, and enhancing patient hip joint mobility is one of the primary objectives of THA. Hip joint mobility is influenced by a variety of factors, including prosthesis selection, prosthesis implant position, soft tissue tension, postoperative rehabilitation, and patient compliance [6]. Our research findings indicate that joint capsule repair can improve patient hip joint ROM. We attribute this improvement to early postoperative rehabilitation for patients. Hip capsule repair may provide a protective effect during rehabilitation exercises [10], allowing patients to engage in more effective training. This can lead to improved hip joint ROM, ultimately enhancing postoperative satisfaction and quality of life. Upon discharge, patients are advised to engage in long-term and consistent rehabilitation exercises. At the three month follow-up, there was a significant difference in hip ROM between the two groups. At the six month follow-up, there was no significant difference in hip internal and external rotation between the two groups. At the final follow-up, differences in hip joint ROM (adduction and abduction) persisted, possibly attributed to variations in early rehabilitation activities and patient comprehension of rehabilitation training (Fig. 2, Details can be found in the supplementary materials). Dislocation represents the primary complication of THA utilizing the posterior-lateral approach [11]. This approach is widely used in clinical practice because of its small incision, which provides a clear surgical field and allows femoral osteotomies. However, this approach is associated with a heightened risk of postoperative dislocation due to the trauma inflicted on the ligamentous structures and external rotator muscles. Pellicci et al. [12] proposed restoring the posterior hip structures to mitigate early dislocations. Early dislocations occur within 6 months postoperatively, while late dislocations manifest after this period. Our findings indicated no dislocations within the initial six months postoperatively in the experimental group, resulting in a dislocation rate of 0%, contrasting with five occurrences in the control group, yielding a 2.4%. This underscores the efficacy of joint capsule repair in reducing early dislocation, consistent with prior research. Subsequent to six months postoperatively, 5 patients in the experimental group and 14 in the control group experienced dislocations, resulting in rates of 2.5% and 6.9%, respectively. This indicates that joint capsule repair can also decrease the incidence of late dislocation. Repairing the hip joint capsule enhances soft tissue stability and joint integrity, thereby diminishing dislocation risk. Hence, we think of hip joint capsule repair as indispensable in the posterior-lateral approach to THA. Notably, among dislocated individuals in the experimental group, three incidents stemmed from falls, whereas the control group witnessed nine post-fall dislocations. Consequently, we emphasize the imperative of postoperative patient education on fall prevention in daily activities.
Logistic regression analysis indicates that hip joint capsule repair, rheumatoid arthritis, epilepsy, and sarcopenia are associated with dislocation. This reaffirms the beneficial role of hip capsule repair in preventing postoperative dislocation. Some studies have found that rheumatoid arthritis patients undergoing THA are at a higher risk of hip prosthesis dislocation [13,14,15,16]. Anatomical differences in the hip joint between rheumatoid arthritis and osteoarthritis patients may be the cause of the increased risk of postoperative dislocation in rheumatoid arthritis patients. Research indicates that rheumatoid arthritis patients have an increased likelihood of developing protrusio acetabula. Anterior acetabular protrusion may elevate the risk of hip impingement and posterior dislocation [17]. Previous studies have found that patients with epilepsy have a higher incidence of dislocation after THA, which may be related to an increased risk of falls [18]. Previous studies suggest that patients with sarcopenia have a higher risk of complications following THA [19, 20]. This may be due to reduced skeletal muscle mass and insufficient tension in soft tissues among sarcopenic patients. Furthermore, surgical-induced muscle damage in sarcopenia patients may exacerbate the decline in muscle strength, thereby increasing the risk of dislocation occurrence. In the future, it is imperative to devise personalized surgical plans for patients with rheumatoid arthritis, epilepsy, and sarcopenia undergoing THA. Enhanced postoperative precautions are essential to mitigate risks like falls. Tailored postoperative rehabilitation programs are recommended to enhance muscle strength and reduce the risk of postoperative dislocation.
Perioperative pain management is also a crucial aspect of THA [21]. Studies have indicated that severe postoperative pain significantly affects patients’ early rehabilitation training and surgical satisfaction [22]. There is a correlation between postoperative pain and postoperative bleeding, as well as the level of postoperative inflammation [23]. In the early postoperative period, patients typically experience significant pain, which makes early rehabilitation exercises difficult. Our study indicates that capsular repair of the hip joint can alleviate early postoperative pain in patients, primarily observed within the first day to one month after surgery (Details can be found in the supplementary materials). This indicates that patients can achieve better rehabilitation outcomes in the early stages. Additionally, the experimental group exhibited lower levels of TBL, OBL, and inflammatory markers compared to the control group (Details can be found in the supplementary materials). During our follow-up period, neither group of patients experienced postoperative infections. We think that the reduction in postoperative blood loss may have reduced the stress response to surgical trauma, thereby leading to a decrease in postoperative inflammatory levels. Postoperative anaemia is a common adverse event following surgery. Research indicates that postoperative anemia is associated with adverse events [24]. Albumin is linked to wound healing postoperatively. Postoperative nutritional status is considered an essential aspect of surgical recovery [25]. Our study found a higher postoperative erythrocyte count, HB level, and albumin level in the experimental group compared to the control group. We think this may be related to reduced postoperative bleeding. This indicates that joint capsule repair may reduce postoperative loss of body composition and contribute to early recovery in patients. DVT and PE are among the risks following THA [26]. Our study found that the experimental group had shorter APTT times compared to the control group, and this difference persisted for up to seven days postoperatively. Additionally, the experimental group had lower levels of D-dimer at discharge compared to the control group. However, the APTT and D-dimer levels for both groups remained within the normal range. During hospitalization, we did not observe any cases of DVT or PE in either group.
Furthermore, we found that the experimental group had shorter hospital stays and lower hospitalization costs compared to the control group, with no difference in surgical duration between the two groups. Some studies indicate that reducing hospitalization time can alleviate patients’ financial burden [27, 28]. This implies that hip capsule repair may alleviate patients’ financial burden, potentially easing government economic pressures. Additionally, our study has several limitations. Firstly, it is a retrospective study; hence, the data collected is limited. Secondly, we only conducted a five year follow-up, and a longer follow-up period might be needed to assess the impact of hip capsule repair.
Conclusions
In posterior-lateral THA, repairing the joint capsule is crucial. It improves postoperative hip joint function and mobility, reducing early and late dislocation risks. This method also lowers postoperative blood loss, pain, inflammation, and economic burden. For patients with rheumatoid arthritis, epilepsy, or sarcopenia undergoing THA, personalized evaluations, surgical plans, protective measures, and rehabilitation programs are vital to minimizing complications, including dislocations.
References
Sloan M, Premkumar A, Sheth NP (2018) Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 100(17):1455–1460. https://doi.org/10.2106/jbjs.17.01617
Abdel MP et al (2016) What safe zone? The vast majority of dislocated THAs are within the Lewinnek Safe Zone for Acetabular component position. Clin Orthop Relat Res 474(2):386–391. https://doi.org/10.1007/s11999-015-4432-5
Chiu FY et al (2000) The effect of posterior capsulorrhaphy in primary total hip arthroplasty: a prospective randomized study. J Arthroplasty 15(2):194–199. https://doi.org/10.1016/s0883-5403(00)90220-1
White RE Jr. et al (2001) Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res 393:163–167. https://doi.org/10.1097/00003086-200112000-00019
Rowan FE et al (2018) Prevention of Dislocation after total hip arthroplasty. J Arthroplasty 33(5):1316–1324. https://doi.org/10.1016/j.arth.2018.01.047
Sheth D et al (2015) Anterior and anterolateral approaches for THA are Associated with Lower dislocation risk without higher revision risk. Clin Orthop Relat Res 473(11):3401–3408. https://doi.org/10.1007/s11999-015-4230-0
Chivas DJ, Smith K, Tanzer M (2006) Role of capsular repair on dislocation in revision total hip arthroplasty. Clin Orthop Relat Res 453:147–152. https://doi.org/10.1097/01.blo.0000238857.61862.34
Ng KCG, Jeffers JRT, Beaule PE (2019) Hip joint capsular anatomy, mechanics, and Surgical Management. J Bone Joint Surg Am 101(23):2141–2151. https://doi.org/10.2106/JBJS.19.00346
Shen SN et al (2022) Hidden blood loss of total knee arthroplasty in hemophilia arthritis: an analysis of influencing factors. BMC Musculoskelet Disord 23(1):587. https://doi.org/10.1186/s12891-022-05535-y
Logishetty K et al (2019) Hip capsule biomechanics after arthroplasty: the effect of implant, approach, and surgical repair. Bone Joint J 101–b(4):426–434. https://doi.org/10.1302/0301-620x.101b4.Bjj-2018-1321.R1
Gillinov SM et al (2022) Incidence, timing, and predictors of hip dislocation after primary total hip arthroplasty for Osteoarthritis. J Am Acad Orthop Surg 30(21):1047–1053. https://doi.org/10.5435/JAAOS-D-22-00150
Pellicci PM, Bostrom M, Poss R (1998) Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res 355:224–228. https://doi.org/10.1097/00003086-199810000-00023
Taylor-Williams O, Nossent J, Inderjeeth CA (2020) Incidence and Complication Rates for Total Hip Arthroplasty in rheumatoid arthritis: a systematic review and Meta-analysis Across Four decades. Rheumatol Ther 7(4):685–702. https://doi.org/10.1007/s40744-020-00238-z
Jiang W et al (2023) More complications and higher transfusion rate in patients with rheumatoid arthritis than osteoarthritis undergoing total hip arthroplasty. Int Orthop 47(5):1189–1196. https://doi.org/10.1007/s00264-023-05728-7
Wooster BM et al (2023) Contemporary outcomes of primary total hip arthroplasty in patients with inflammatory arthritis. Bone Joint J. 105-b(7):768–774. https://doi.org/10.1302/0301-620x.105b7.Bjj-2023-0220.R1
Ravi B et al (2014) Increased risk of complications following total joint arthroplasty in patients with rheumatoid arthritis. Arthritis Rheumatol 66(2):254–263. https://doi.org/10.1002/art.38231
Matsuno H et al (2000) Cementless cup supporter for protrusio acetabuli in patients with rheumatoid arthritis. Int Orthop 24(1):15–18. https://doi.org/10.1007/s002640050004
Cole MW et al (2023) The impact of Epilepsy on Complication Rates after Total Joint Arthroplasty: a propensity score-matched cohort study. J Arthroplasty 38(2):209–214e1. https://doi.org/10.1016/j.arth.2022.08.022
Ogawa T et al (2018) Soft tissue tension is four times lower in the unstable primary total hip arthroplasty. Int Orthop 42(9):2059–2065. https://doi.org/10.1007/s00264-018-3908-9
Chang K et al (2023) Sarcopenia Is Associated with an Increased Risk of Postoperative Complications Following Total Hip Arthroplasty for Osteoarthritis. Biology (Basel). 12(2). https://doi.org/10.3390/biology12020295
Panzenbeck P et al (2021) Procedure-specific acute pain trajectory after elective total hip arthroplasty: systematic review and data synthesis. Br J Anaesth 127(1):110–132. https://doi.org/10.1016/j.bja.2021.02.036
Li JW, Ma YS, Xiao LK (2019) Postoperative Pain Management in total knee arthroplasty. Orthop Surg 11(5):755–761. https://doi.org/10.1111/os.12535
Xiang SC et al (2024) Intra-articular injection of tranexamic acid in patients with haemophilia arthritis: retrospective controlled study in total knee arthroplasty. Int Orthop 48(3):683–692. https://doi.org/10.1007/s00264-023-05983-8
Myles PS et al (2022) Postoperative anaemia and patient-centred outcomes after major abdominal surgery: a retrospective cohort study. Br J Anaesth 129(3):346–354. https://doi.org/10.1016/j.bja.2022.06.014
Hirsch KR, Wolfe RR, Ferrando AA (2021) Pre- and Post-surgical Nutrition for Preservation of Muscle Mass, Strength, and functionality following orthopedic surgery. Nutrients 13(5). https://doi.org/10.3390/nu13051675
Sidhu VS et al (2022) Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL Randomized Trial. Jama 328(8):719–727. https://doi.org/10.1001/jama.2022.13416
Chavez MA et al (2022) Length of stay and trauma center finances: a disparity of payer source at a Level I trauma center. J Trauma Acute Care Surg 92(4):683–690. https://doi.org/10.1097/ta.0000000000003529
Wohlgemut JM et al (2021) Current and projected Financial Burden of Emergency General surgery for adults in Scotland’s single Payer Healthcare System: a cost analysis of Hospital admissions. Ann Surg 274(6):e522–e528. https://doi.org/10.1097/sla.0000000000003769
Acknowledgements
We thank all patients who participated and allowed their data to be anonymously used for the present study. Also, we would like to thank all staff from the participating departments and clinics.
Funding
The research were supported by Traditional Chinese Medicine Science and Technology Program of Zhejiang Province (No. 2023ZL367) and National Nature Science Foundation of Zhejiang Province (No.LY24H270001).
Author information
Authors and Affiliations
Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, H.S. and S.X.Y.; Methodology, H.S. and H.H.; Investigation, H.H. and Z.Y.Z.; Formal Analysis, H.S.; Resources, T.T.X. and P.J.T.; Writing - Original Draft, H.S. and Y.S.X.; Writing - Review & Editing, S.N.L, X.Y.H, S.C.X., Y.C.G. H.J.Z., L.C., T.T.X., and P.J.T.; Visualization, H.S., S.N.L, X.Y.H., J.Y.L., and J.L.; Supervision, T.T.X.; Funding Acquisition, T.T.X. and P.J.T.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Zhejiang Chinese Medical University (the study registration number is 2023-KLS-130-01). This study did not involve direct contact with humans or animals.
Informed consent
Informed consent was obtained from all participants. All research was performed in accordance with relevant guidelines/regulations.
Conflict of interest
The author(s) declare no potential competing interests in the research, authorship, and/or publication of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Su, H., Yu, S., Huang, H. et al. Importance of hip capsular repair in total hip arthroplasty (THA) via the posterior lateral approach: a five year retrospective cohort study. International Orthopaedics (SICOT) (2024). https://doi.org/10.1007/s00264-024-06293-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00264-024-06293-3