Abstract
Purpose
This study aimed to identify factors related to collapse progression in Japanese Investigation Committee classification type B osteonecrosis of the femoral head (ONFH) and to identify patients who would benefit from surgical treatment.
Methods
This study included 41 patients (56 hips) with type B ONFH with a minimum follow-up of three years. Based on a ≥ 3 mm collapse progression in ONFH, we categorised patients into two groups: collapse progression and no collapse progression. Sagittal and coronal computed tomography images were used to measure the necrotic region relative to the intact femoral head diameter. The ratios of the necrotic regions of transverse and vertical diameter in coronal and sagittal images are defined as mediolateral transverse and mediolateral vertical, anteroposterior transverse and anteroposterior vertical, respectively. Demographic data and these imaging findings were compared between the two groups. We established a cut-off value for predicting collapse progression through receiver operating characteristic analysis and determined survival rates.
Results
Type B ONFH had a 17.8% collapse progression rate. The mediolateral transverse, mediolateral vertical, anteroposterior transverse, and anteroposterior vertical were significantly higher in the collapse progression group (P < 0.01). Mediolateral transverse was an independent risk factor of collapse progression (hazard ratio, 1.27; 95% confidence interval, 1.03–1.57; P = 0.03), with an optimal cut-off of 45.6%. The 5-year survival rates with collapse progression as the endpoints were 57.0 and 94.9% in the mediolateral transverse of ≥ 45.6 and < 45.6%, respectively.
Conclusion
A mediolateral transverse of ≥ 45.6% predicts collapse progression in patients with type B ONFH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteonecrosis of the femoral head (ONFH) is a rare disease characterized by ischaemic necrosis of the femoral head [1, 2]. ONFH progression to collapse of the femoral head is associated with worsening pain and affects the patients’ activities of daily living and quality of life [3]. Total hip arthroplasty (THA) is the most common treatment for patients with ONFH, with favourable long-term outcomes [4, 5]. However, ONFH is more common in younger patients; long-term implant preservation can be challenging in these patients, who may require THA revision [6]. Consequently, joint-preserving procedures are also considered for younger patients with ONFH, and favourable treatment outcomes have been reported when joint-preserving surgery is performed before ONFH progresses to femoral head collapse [7,8,9,10,11].
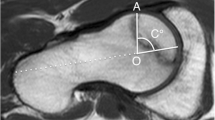
Previous reports have considered the size of the necrotic region as an important factor in ONFH collapse [12,13,14]. The Japanese Investigation Committee (JIC) classifies ONFH based on the relationship between the weight-bearing portion of the acetabulum and the lateral boundary of the necrotic region on anteroposterior (AP) radiographs (Fig. 1) [15, 16]. The femoral head collapse rates vary by classification type and have been reported as follows: type A, 0–9%; type B, 13–29%; and type C, 26–75% [17,18,19]. As type C has a high femoral head collapse rate, joint-preserving procedures should be performed early when indicated before the femoral collapse. Type B has a lower collapse rate, and it remains unclear whether intervention is necessary for these patients. It is essential to identify necrotic features of type B ONFH related to femoral head collapse to determine which patients should undergo early intervention.
The classification of the Japanese Investigation Committee of Health and Welfare (A) Type A regions occupy the medial third or less of the weight-bearing portion. (B) Type B regions occupy the medial two-thirds or less of the weight-bearing portion. (C) Type C regions occupy more than the medial two-thirds of the weight-bearing portion
In recent years, various reports have emphasised the importance of three-dimensional assessments in evaluating the volume of necrotic regions in ONFH or using plain lateral radiographs to assess the progression of femoral head collapse [20,21,22]. Therefore, this study aimed to use imaging of the necrotic region to assess the factors contributing to femoral head collapse in patients with type B ONFH and develop criteria that predict collapse progression.
In this study, we addressed the following questions: (1) What imaging parameters are associated with femoral head collapse in patients with type B ONFH? (2) Is there a cut-off value in image evaluation that predicts collapse progression and therefore can aid in selecting the treatment strategy?
Materials and methods
Patients
We retrospectively reviewed the data of 335 patients diagnosed with ONFH at our hospital between January 2010 and December 2020. Among these, 48 were categorised as type B based on both plain radiographs and magnetic resonance imaging (MRI), according to the JIC Classification System [15, 16]. Necrotic regions were classified on AP radiographs based on the positional relationship between the weight-bearing portion of the acetabulum and the lateral boundary of the necrotic region, with type B regions occupying the medial one- to two-thirds of the weight-bearing portion. We excluded patients with a history of hip injuries and conservative follow-up periods of less than three years from the onset of hip pain. The final study population comprised 41 patients (56 hips) (Fig. 2). A previous study reported that hip joint function can be preserved even with conservative treatment in ONFH patients with collapse cessation < 3 mm [23]. Therefore, based on a ≥ 3-mm collapse progression in ONFH, we categorised these patients into two groups: the collapse progression and the no collapse progression group. Written informed consent was obtained from all patients, and the study was approved by our Ethics Committee and conducted in accordance with the principles outlined in the Declaration of Helsinki.
Data collection
Demographic and clinical data, including age, sex, body mass index (BMI), aetiology of OFNH, and follow-up period were collected retrospectively from medical records. All patients underwent radiography, computed tomography (CT), and MRI of the hip joint at the onset of hip pain. We diagnosed ONFH using radiography and MRI and applied the JIC classification. The extent of necrosis in the femoral head was determined using CT.
Radiological assessment
During each radiographic assessment, the extent of femoral head collapse was determined from AP radiographs. We measured the distance between an estimated circle that best fitted each femoral head and the deepest point of collapse along the line passing through the centre of the femoral head, with measurements recorded to 0.01 mm [24]. The maximum depth observed on the AP and lateral radiographs was used to calculate the extent of femoral head collapse. In this study, collapse progression was defined as the appearance of sphericity loss and its continuous worsening, with a progression of ≥ 3 mm in collapse depth from the onset of hip pain.
CT was performed at the onset of hip pain in each patient. CT scans were performed with a 1 mm slice thickness, and multiplanar reconstruction was performed to reconstruct the images. Necrotic regions were characterised by band-like sclerosis. Sagittal and coronal CT scans were used to measure the maximum transverse and vertical diameters of the necrotic region at the centre of the femoral head. These measurements were compared with the diameter of the intact femoral head to determine the ratio. Most cases did not exhibit femoral head collapse during the initial visit, and we defined the femoral head diameter of the ONFH side in CT slices at the centre of the femoral head as the intact femoral head size. As shown in Fig. 3, the ratios of the necrotic regions in the coronal and sagittal planes were calculated as (a-ii)/(a-i), (a-iv)/(a-iii), (b-ii)/(b-i), and (b-iv)/(b-iii) for the mediolateral (ML) transverse, ML vertical, AP transverse, and AP vertical, respectively. Nam et al. evaluated necrotic volumes using coronal and sagittal images of the centre of the femoral head [20]. The volumes were calculated using the ratios previously described, determined by ML transverse × AP transverse × 100.
(a) Coronal image at the centre of the femoral head. (b) Sagittal image at the centre of the femoral head. (i) maximum diameter of the femoral head (ii) maximum transverse diameter of the necrotic region (iii) maximum diameter of the femoral head (iv) maximum vertical diameter of the necrotic region
All imaging findings were assessed separately by two orthopaedic surgeons. Intra- and inter-observer reliabilities were assessed using intraclass correlation coefficients.
Statistical analysis
Differences between groups were assessed using the Student's t-test for normally distributed continuous variables. The Chi-squared test was used to compare categorical variables. The Cox proportional hazards model was used to identify risk factors for femoral head collapse in patients with JIC type B ONFH. A receiver operating characteristic (ROC) curve was generated, and the area under the curve (AUC), sensitivity, and specificity of each factor were calculated. Kaplan–Meier survival curves were generated with the occurrence of collapse progression (≥ 3 mm) as the endpoint and analysed using the log-rank test. All statistical analyses were performed using EZR software version 1.38 (64-bit). P < 0.05 was considered indicative of statistical significance [25].
Results
Table 1 presents the demographic and clinical characteristics of the study population. The mean age of the patients in the overall cohort was 38.7 years, and 21 patients (51.2%) were male. The aetiology of ONFH was alcohol-induced in six cases (14.6%), idiopathic osteonecrosis in four cases (9.8%), and steroid-induced in 31 cases (75.6%). In the collapse progression group, there were ten hips and three males (30.0%), and in the no collapse progression group, there were 46 hips and 22 males (47.8%). The prevalence of collapse progression of ≥3 mm in the study cohort was 17.8%, while the prevalence of collapse progression characterised by a loss of femoral head sphericity of <3 mm was 8.9%. No significant differences were observed between the two groups regarding age, sex, BMI, or ONFH aetiology. A significant difference was observed in the ML transverse (31.3±16.0% in the no collapse progression group vs. 49.9±8.3% in the collapse progression group; P = 0.001), ML vertical (29.0±19.5% in the no collapse progression group vs. 54.6±22.3% in the collapse progression group; P = 0.001), AP transverse (39.4±21.1% in the no collapse progression group vs. 69.4±16.8% in the collapse progression group; P < 0.001), AP vertical (36.7±17.6% in the no collapse progression group vs. 60.4±22.3% in the collapse progression group; P = 0.002), and necrotic volume (13.4±12.2 in the no collapse progression group vs. 37.0±11.9 in the collapse progression group; P < 0.001) (Table 2).
Variables including age, sex, BMI, ML transverse, ML vertical, and AP transverse were entered into the Cox proportional hazards model; only ML transverse (hazard ratio, 1.27; 95% confidence interval [CI], 1.03–1.57; P = 0.03) was an independent risk factor for the collapse of the femoral head in patients with JIC type B ONFH (Table 3). The ROC analysis showed that the optimal cut-off value for the ML transverse to predict femoral head collapse in type B ONFH was 45.6% (sensitivity, 0.800; specificity, 0.804; AUC, 0.857) (Fig. 4). The Kaplan–Meier survival curves, with the endpoint defined as the occurrence of collapse progression of ≥ 3 mm, showed a significant difference in the survival rate between ML transverse < 45.6% and ≥ 45.6% (P < 0.001) (Fig. 5). The 5-year survival rate was 94.9% (95% CI, 81.0–98.7%) %, and 57.0% (95% CI, 30.1–76.9%). Representative cases are shown in Figs. 6 and 7, where ML transverse was < 45.6% and ≥ 45.6%, respectively.
(a) Radiograph showing the symptomatic right ONFH of a 37-year-old woman at the first visit. (b) T1 MRI, coronal section. (c) CT, coronal section, showing 53.7% (≥ 45.6%) of ML transverse and 73.4% of ML vertical. (d) CT, sagittal section, showing 82.5% of AP transverse and 73.6% of AP vertical. (e) Radiograph showing collapse progression (≥ 3 mm) of the right ONFH 1.5 years after the first visit. ONFH, osteonecrosis of the femoral head; MRI, magnetic resonance imaging; CT, computed tomography; ML, mediolateral; AP, anteroposterior
(a) Radiograph showing symptomatic right ONFH of a 32-year-old woman at the first visit. (b) T1 MRI, coronal section. (c) CT, coronal section, showing 34.7% (< 45.6%) of ML transverse and 68.4% of ML vertical. (d) CT, sagittal section, showing 30.3% of AP transverse and 51.8% of AP vertical. (e) Radiograph showing no collapse progression of the right ONFH 3 years after the first visit. ONFH, osteonecrosis of the femoral head; MRI, magnetic resonance imaging; CT, computed tomography; ML, mediolateral; AP, anteroposterior
Discussion
In this study, we evaluated the progression rate of femoral head collapse and the factors that contributed to this collapse by analysing the imaging findings of necrotic regions in patients with JIC type B ONFH and investigated the criteria for predicting femoral head collapse. Over a follow-up period of more than three years, the progression rate of femoral head collapse in patients with type B ONFH was 17.8%. The ML transverse, ML vertical, and AP transverse, calculated from imaging the necrotic regions, were associated with femoral head collapse, and the ML transverse was an independent risk factor for femoral head collapse. The optimal cut-off value was 45.6%, and patients with an ML transverse < 45.6% had a significantly higher survival rate than those with an ML transverse ≥ 45.6%, with femoral head collapse as the endpoint.
A systematic review of 16 papers focusing on ONFH revealed that in radiographic images, small-sized necrotic regions (< 25%) had a 7% progression rate, medium-sized regions (25–50%) had a 25% progression rate, and large-sized regions (> 50%) had an 84% progression rate. This indicates a correlation between the extent of femoral head necrosis and the progression of femoral head collapse [19]. Recent reports have also shown that the extent of anterior necrotic regions on lateral radiographs is associated with a higher risk of femoral head collapse [21, 22]. Additionally, necrotic volume (an index obtained by multiplying the ratio of the coronal necrotic region and the sagittal necrotic region at the centre of the femoral head on MRI) has been identified as a significant prognostic factor [20]. Therefore, the evaluation of lateral radiographs (to measure AP necrotic regions) in addition to AP radiographs (to measure ML necrotic regions) is crucial. In this study, we used the transverse and vertical diameters of the necrotic regions at the centre of the femoral head in coronal and sagittal CT images as a simple indicator of the extent of the ML (coronal images) and AP (sagittal images) necrotic regions. In our study, the ML transverse, ML vertical, and AP transverse necrotic regions were associated with femoral head collapse, even in type B ONFH with its low collapse rate. These were considered important indicators to assess the potential for femoral head collapse. Following adjustments for age, BMI, and sex, only ML transverse remained an independent risk factor for femoral head collapse. ML necrotic regions have previously been shown to be particularly important in femoral head collapse, with a study suggesting that the lateral pillar of the femoral head plays a crucial role in preventing femoral head collapse in ONFH [26]. This is consistent with the results of our study.
Joint-preserving procedures for type B ONFH often involve core decompression or curved intertrochanteric varus osteotomy (CVO), depending on the size of the necrotic region. Core decompression has been reported to have a strong preventive effect against femoral head collapse, particularly in early-stage cases (Ficat stage I) [27, 28]. Furthermore, a ten year survival rate of 91.0% to 91.8% has been reported for CVO when using the surgical procedure as the endpoint, indicating favourable treatment outcomes [8, 9, 29]. Both procedures require intervention before femoral head collapse occurs. However, owing to the lower collapse rate in patients with type B ONFH, it is crucial to select appropriate candidates for these joint-preserving procedures. In this study, the optimal cut-off value for ML transverse to predict femoral head collapse in type B ONFH was 45.6%. In 2021, the Association Research Circulation Osseous (ARCO) introduced a novel CT-based classification for early-stage ONFH [30], where necrotic regions are classified into three types: types 1 and 2 at the centre of the femoral head and types 2 and 3 extending laterally to the acetabular edge. They reported femoral head collapse rates of 0%, 29%, and 58% for types 1, 2, and 3, respectively. The 45.6% cut-off value in this study is equivalent to, and supports, the novel ARCO classification. The survival rate with collapse as the endpoint was significantly higher in cases with the ML transverse < 45.6% than in those with the ML transverse ≥ 45.6%. Therefore, the results of this study may offer valuable criteria for assessing surgical indications for type B ONFH and predicting patient prognosis.
This study has several limitations. First, this was a retrospective study with a relatively small sample size of 56 hips. Expanding the patient cohort could enhance the statistical power of the results. Additionally, the relatively short mean follow-up period in this study raises the possibility that further progression of collapse or osteoarthritic changes could occur in the natural history of the condition.
In conclusion, the ML transverse was identified as an independent risk factor for femoral head collapse in patients with JIC type B ONFH. Setting the cut-off value of the ML transverse at 45.6% may provide an effective criterion for determining the need for surgical treatment of type B ONFH.
Data availability
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Mankin HJ (1992) Nontraumatic necrosis of bone (osteonecrosis). N Engl J Med 326:1473–1479
Arbab D, König DP (2016) Atraumatic femoral head necrosis in adults. Dtsch Arztebl Int 113:31–38
Osawa Y, Seki T, Takegami Y et al (2018) Do femoral head collapse and the contralateral condition affect patient-reported quality of life and referral pain in patients with osteonecrosis of the femoral head? Int Orthop 42(7):1463–1468
Osawa Y, Seki T, Takegami Y et al (2018) Cementless total hip arthroplasty for osteonecrosis and osteoarthritis produce similar results at ten years follow-up when matched for age and gender. Int Orthop 42:1683–1688
Kim HS, Park JW, Ha JH et al (2022) Third-generation ceramic-on-ceramic total hip arthroplasty in patients with osteonecrosis of the femoral head: a 10- to 16-year follow-up study. J Bone Joint Surg Am 104:68–75
Hartofilakidis G, Karachalios T, Karachalios G (2005) The 20-year outcome of the charnley arthroplasty in younger and older patients. Clin Orthop Relat Res 434:177–182
Wang B-L, Sun W, Shi Z-C et al (2010) Treatment of nontraumatic osteonecrosis of the femoral head with the implantation of core decompression and concentrated autologous bone marrow containing mononuclear cells. Arch Orthop Trauma Surg 130:859–865
Ito H, Tanino H, Yamanaka Y et al (2012) Long-term results of conventional varus half-wedge proximal femoral osteotomy for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Br 94:308–314
Osawa Y, Seki T, Okura T et al (2021) Long-term outcomes of curved intertrochanteric varus osteotomy combined with bone impaction grafting for non-traumatic osteonecrosis of the femoral head. Bone Joint J 103-B:665–671
Liang D, Pei J, Zhang X, Chen X (2023) Clinical outcomes of autologous platelet-rich plasma and bone marrow mononuclear cells grafting combined with core decompression for Association Research Circulation Osseous II-IIIA stage non-traumatic osteonecrosis of the femoral head. Int Orthop 47:2181–2188
Hernigou P, Verrier S, Homma Y et al (2023) Prognosis of hip osteonecrosis after cell therapy with a calculator and artificial intelligence: ten year collapse-free survival prediction on three thousand and twenty one hips. Int Orthop 47:1689–1705
Hernigou P, Lambotte JC (2000) Bilateral hip osteonecrosis: influence of hip size on outcome. Ann Rheum Dis 59:817–821
Hernigou P, Habibi A, Bachir D, Galacteros F (2006) The natural history of asymptomatic osteonecrosis of the femoral head in adults with sickle cell disease. J Bone Joint Surg Am 88:2565–2572
Hernigou P (2023) Revisiting prediction of collapse in hip osteonecrosis with artificial intelligence and machine learning: a new approach for quantifying and ranking the contribution and association of factors for collapse. Int Orthop 47:677–689
Ando W, Sakai T, Fukushima W et al (2021) Japanese Orthopaedic Association 2019 Guidelines for osteonecrosis of the femoral head. J Orthop Sci 26:46–68
Sugano N, Atsumi T, Ohzono K et al (2002) The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci 7:601–605
Nakamura J, Harada Y, Oinuma K et al (2010) Spontaneous repair of asymptomatic osteonecrosis associated with corticosteroid therapy in systemic lupus erythematosus: 10-year minimum follow-up with MRI. Lupus 19:1307–1314
Shimizu K, Moriya H, Akita T et al (1994) Prediction of collapse with magnetic resonance imaging of avascular necrosis of the femoral head. J Bone Joint Surg Am 76:215–223
Mont MA, Zywiel MG, Marker DR et al (2010) The natural history of untreated asymptomatic osteonecrosis of the femoral head: a systematic literature review. J Bone Joint Surg Am 92:2165–2170
Nam KW, Kim YL, Yoo JJ et al (2008) Fate of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg Am 90:477–484
Utsunomiya T, Motomura G, Yamaguchi R et al (2023) Effects of the location of both anterior and lateral boundaries of the necrotic lesion on collapse progression in osteonecrosis of the femoral head. J Orthop Sci. https://doi.org/10.1016/j.jos.2023.01.011
Fan Y, Zhang J, Chen M et al (2022) Diagnostic value of necrotic lesion boundary in bone collapse of femoral head osteonecrosis. Int Orthop 46:423–431
Osawa Y, Takegami Y, Kato D et al (2023) Hip function in patients undergoing conservative treatment for osteonecrosis of the femoral head. Int Orthop 47:89–94
Kubo Y, Motomura G, Ikemura S et al (2018) The effect of the anterior boundary of necrotic lesion on the occurrence of collapse in osteonecrosis of the femoral head. Int Orthop 42:1449–1455
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Sun W, Li Z-R, Wang B-L et al (2014) Relationship between preservation of the lateral pillar and collapse of the femoral head in patients with osteonecrosis. Orthopedics 37:e24–e28
Lavernia CJ, Sierra RJ (2000) Core decompression in atraumatic osteonecrosis of the hip. J Arthroplasty 15:171–178
Yoon TR, Song EK, Rowe SM, Park CH (2001) Failure after core decompression in osteonecrosis of the femoral head. Int Orthop 24:316–318
Zhao G, Yamamoto T, Ikemura S et al (2010) Radiological outcome analysis of transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head at a mean follow-up of 12.4 years. J Bone Joint Surg Br 92:781–786
Koo K-H, Mont MA, Cui Q et al (2022) The 2021 Association Research Circulation Osseous Classification for Early-Stage Osteonecrosis of the Femoral Head to Computed Tomography-Based Study. J Arthroplasty 37:1074–1082
Acknowledgements
We thank the following people for their contributions: Takamune Asamoto, Shinya Tanaka and Keiji Otaka.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Hiroaki Ido [1] substantial contributions to research design, or the acquisition, analysis or interpretation of data; [2] drafting the paper or revising it critically; [3] approval of the submitted and final versions.
Yusuke Osawa: [1] substantial contributions to research design, or the acquisition, analysis or interpretation of data; [2] drafting the paper or revising it critically; [3] approval of the submitted and final versions.
Yasuhiko Takegami: [2] drafting the paper or revising it critically; [3] approval of the submitted and final versions.
Hiroto Funahashi: [2] drafting the paper or revising it critically; [3] approval of the submitted and final versions.
Yuto Ozawa: [1] the acquisition of data; [2] approval of the submitted and final versions.
Shiro Imagama: [1] drafting the paper or revising it critically; [2] approval of the submitted and final versions.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the institutional review board, and it conforms to the provisions of the Declaration of Helsinki.
Consent to publish
Patients signed informed consent regarding publishing their data.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ido, H., Osawa, Y., Takegami, Y. et al. Factors related to collapse progression in Japanese Investigation Committee classification type B osteonecrosis of the femoral head. International Orthopaedics (SICOT) 48, 2033–2040 (2024). https://doi.org/10.1007/s00264-024-06221-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-024-06221-5