Abstract
Purpose
The aim of our study was to determine the surgical outcomes of patients who underwent lateral femoral sliding osteotomy (LFSO) with total knee arthroplasty (TKA) for Ranawat’s type 2 fixed valgus deformity.
Methods
The consecutive patients who underwent primary TKA with posterior-stabilized implant and LFSO for fixed valgus deformity were reviewed. The radiological parameters analyzed were pre- and postoperative hip-knee-ankle (HKA) angle and tibio-femoral angle in varus-valgus stress views. The clinical outcome was measured by Oxford knee score (OKS), knee society score (KSS), and functional score (KSS-F). The complications and any reoperation were noted in the follow-up.
Results
There were total 28 patients included with an average follow-up time of 47.2 ± 24.9 months. The average arc of motion was 101.3 ± 23.8° preoperatively and 102.7 ± 11.8° postoperatively (p > 0.05). The average deformity in varus and valgus stress views was 196.6 ± 4.8 and 207.8 ± 7.4°, respectively. There was significant improvement in HKA from 205.2 ± 8.3° preoperatively to 181.9 ± 3.7° postoperatively (p < 0.05). At the final follow-up, bony union of the osteotomy fragment was noted in all the patients. There was significant improvement in OKS, KSS, and KSS-F score from a preoperative 15.1 ± 3.9, 35.1 ± 10.6, and 26.6 ± 12.6 to 40.3 ± 2.9, 85.6 ± 4.8, and 89.4 ± 7.7, postoperatively (p < 0.05), respectively. One patient had acute periprosthetic joint infection that was managed with debridement and polyethylene insert exchange.
Conclusion
Lateral femoral sliding osteotomy is an effective technique for optimal soft tissue balance in fixed valgus deformity. It provides satisfactory clinical outcome with restoration of knee alignment without using the constrained implants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Valgus deformity contributes to nearly 10% of the patients undergoing total knee arthroplasty (TKA). It is classified into three grades from mild to severe based on the magnitude of the deformity and status of medial soft tissue structures [1]. Fixed valgus deformity constitutes about 20% of the valgus deformity and it poses numerous technical challenges and has variable clinical results [1,2,3]. In severe valgus deformity, sequential release of lateral structures of the knee like iliotibial band, posterolateral capsule, popliteus, lateral collateral ligament, and hamstring muscles has been suggested for optimal balancing of flexion and extension gaps [1, 4,5,6]. If the releases were extensive, it might lead to mediolateral instability and warrants the need for constrained implants [1, 4].
Lateral femoral sliding osteotomy (LFSO) or lateral epicondylar osteotomy technique was initially described by Scuderi and Insall in 1995 and it was Brilhault and Burdin et al. in 2002 who first demonstrated a series of 13 patients with good to excellent functional results after LFSO [7, 8]. It was used as a part of sequential soft tissue release that allows precise and controlled lengthening of the lateral structures in fixed valgus deformity [5, 7]. It involves osteotomizing the lateral epicondyle with attached lateral collateral ligament (LCL) and popliteus tendon and shifting the bony fragment distally and/or posteriorly.
The advantages of LFSO were predictable soft tissue release, preservation of the integrity of lateral structures like LCL and popliteus tendon, avoiding a constrained implant, wider visualization of posterolateral structures, and reducing the risk of peroneal nerve palsy [4]. The limitations of using this technique were the potential risk of pseudarthrosis, residual pain at the osteotomy site, and chances of residual instability [8]. This technique cannot be performed if the sliding distance required is more than the distance from the distal femur resection bony surface to the attachment of ligaments [9]. This technique was not frequently performed and reports described in the literature were scarce [4, 5, 8]. The aim of our study was to determine the surgical outcomes of consecutive patients who underwent LFSO with TKA for fixed valgus deformity. The hypothesis of our study was LFSO helps in optimal clinical and radiological outcome in patients with fixed valgus deformity without using the constrained prosthesis.
Patients and methods
Preoperative data
The consecutive patients who underwent primary TKA with LFSO for fixed valgus deformity [1] from January 2014 to August 2021 were reviewed and included in the study. Ranawat et al. classified valgus deformity into three types, namely type I, where the valgus deformity is minimal with less than 10° tibio-femoral angle with intact medial collateral ligament (MCL); type II, where there is fixed deformity between 10 and 20° with attenuated MCL and stretching of medial soft-tissues; and type III, where the deformity is more than 20° and associated impaired medial soft tissue structures [1]. In our study, patients had severe deformity of more than 20° on varus stress but had intact medial collateral ligament. Since there is overlap in the classification types, we have included all the patients with fixed valgus deformity and intact MCL.
The patients with incomplete radiographs, previous surgeries in the same knee, post-traumatic arthritis, valgus knees with non-functional MCL requiring hinge prosthesis (n = 6) were excluded. The institutional ethical committee approval was obtained and conducted under the principles of the Helsinki Declaration. Informed written consent for publishing their data was obtained from all the patients. Clinical parameters like age, sex, BMI, diagnosis, prosthesis implanted, and knee range of motion were retrieved from medical records.
Radiographs taken were hip-knee-ankle anteroposterior (AP) weight-bearing radiographs (Fig. 1a), lateral view, skyline view for patella, and anteroposterior varus-valgus stress views (Fig. 1d, e) of the knee. The radiological parameters analyzed were hip-knee-ankle (HKA) angle or mechanical tibio-femoral angle, anatomical lateral distal femoral angle (LDFA), anatomical medial proximal tibial angle (MPTA)4, and tibio-femoral angle in varus-valgus stress AP radiographs.
a, b, c Preoperative radiographs showing severe valgus deformity with lateral femoral condylar hypoplasia. d, e Varus-valgus stress anteroposterior radiographs showing partially correctable valgus deformity. f Preoperative clinical picture showing severe valgus deformity on the right side. g Postoperative follow-up photo showing correction of the deformity. h, I, j Postoperative radiographs after total knee arthroplasty with lateral femoral sliding osteotomy (LFSO). The LFSO fragment has healed with restoration of neutral leg alignment
Hip-knee-ankle angle is the angle between the femoral and tibial mechanical axis. The anatomical lateral distal femoral angle (LDFA) and anatomical medial proximal tibial angle (MPTA) were measured from tangential of articular surface with their respective anatomical axis. The clinical outcome was measured by preoperative and postoperative Oxford knee score (OKS), knee society score (KSS), and functional score (KSS-F). The complications and any reoperation were noted in the follow-up.
The Oxford knee score (OKS) is a 12-item patient-reported outcome measure to assess function and pain after total knee arthroplasty [10]. The knee society score (KSS) had total score of 100 points with three components, namely pain, range of motion, and stability. The deductions were done if there was malalignment, flexion contracture, or extensor lag. The functional score also has 100 points and it has two components, namely walking capacity and stair climbing ability and deductions done if the patient uses any support [11].
Surgical technique
All the surgeries were performed by a fellowship trained high volume arthroplasty surgeon. Under tourniquet control, through anterior midline incision, lateral (Fig. 2b) or medial parapatellar arthrotomy was used to expose the knee. Conventional TKA was done in a standard manner. Individualized valgus correction angle for distal femur cuts and medialized tibial reference in case of tibia valga were taken. In case of hypoplastic lateral femoral condyle (Fig. 2c), the cartilage over the condyle was removed until the subchondral bone and the defect were addressed with augments. After confirming the adequate rotation with epicondylar axis as the reference, anterior, posterior, and chamfer cuts were done using four-in-one cutting block. Posterior cruciate ligament (PCL) acts as a central pivot and limits the lateral opening [7], and hence, we divided PCL in all the cases. Soft tissue balancing was first done in extension by releasing the iliotibial band from the Gerdy’s tubercle and posterolateral capsule subperiosteally.
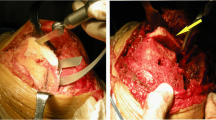
a Preoperative radiographs showing severe valgus deformity of the right leg and varus-valgus stress anteroposterior radiographs showing partially correctable valgus deformity. b Intraoperative picture showing lateral parapatellar arthrotomy. c Exposure of knee showing the lateral femoral hypoplasia and lateral tibial condyle bone defect. d Completion of lateral femoral sliding osteotomy. e Osteotomy fragment distalised and posteriorized and fixed with two cancellous screws. f Postoperative radiographs after total knee arthroplasty with lateral femoral sliding osteotomy and showing neutral leg alignment
LFSO was considered when there was significant soft tissue imbalance after preliminary release with lateral tightness in extension and flexion with asymmetrical gaps with difference more than 5 mm. The osteotomy was done on the lateral one-third of femoral condyle with good bony chunk (Fig. 2d) to facilitate subsequent fixation with screws [4, 5, 7]. The osteotomy was started with an oscillating saw from distal to proximal with knee in 90° of flexion achieving a precise cut. After inserting the spacer block, the bony fragment was shifted distally and/ or posteriorly until the equal flexion and extension gaps were achieved. Then, the fragment was fixed at that isometric position with K wires and overhanging fragment was trimmed (Fig. 2e).
The definitive components were cemented and the bony fragment was finally fixed with two or three screws and washer (Fig. 2e). We have used posterior-stabilized prosthesis (PFC Sigma - DePuy, Indianapolis, IN) in all our patients. The PFC sigma posterior stabilized design prosthesis was versatile and allows addition of augments and stem even if there is hypoplastic lateral femoral condyle, and hence, the necessity for revision implants is avoided. If the residual lateral femoral condyle bone stock was small or if there was concomitant osteoporosis or when augments size more than 4 mm were used for lateral condyle bone defect, a femoral stem augmentation was done. We have used computer-assisted navigation for two patients with concomitant severe extra-articular deformity (Fig. 2).
Postoperatively, patients were mobilized with full weight bearing walking with walker support for two weeks and gradually weaned off with the walker. A knee immobilizer was given as a support for one month. Patients were encouraged to do static quadriceps exercises and active knee bending exercises as tolerated from first postoperative day. Aspirin and intermittent pneumatic compression device were used for deep vein thrombosis prophylaxis.
Follow-up
Among the 28 patients, 24 patients completed the scheduled follow-up. Two foreign patients and other two patient’s functional outcome reviewed near their local hospital and the functional scores were obtained through the telephonic interview. The patients were reviewed at three months, six months, and every year thereafter. The LFSO osteotomy union time is calculated from the date of index surgery to the radiological evidence of union noted in the follow-up. The surgical outcomes were assessed and compared between preoperative period and the final follow -up. Patients were enquired about the subjective instability especially while climbing downstairs and comprehensive physical examination including instability, patellar tracking, and functional scores was evaluated. Postoperative correction in HKA angle was calculated from the long leg films.
Statistical analysis
The data were entered in Microsoft Excel in codes and analysis was done using SPSS for Windows Inc. version 22 (IBM Inc., Chicago, IL). The categorical variables like preoperative diagnosis, approach, and patellar resurfacing were reported as frequencies and percentages. The continuous variables were reported as mean (standard deviation) for BMI, arc of motion, and radiological parameters like LDFA, MPTA, tibial slope and tibio-femoral angle in stress views. Comparison of means between preoperative and postoperative mechanical tibio-femoral angle, Oxford knee score, knee society, and knee society functional score were done using unpaired Student t-test. p values less than 0.05 was considered significant.
Results
There were total 28 patients included in the study with an average age of 64.3 years (range, 45 to 80 years). The average follow-up time was 47.2 ± 24.9 months (range, 12 to 92 months). The preoperative diagnosis was osteoarthritis in 24 (85.7%) patients and rheumatoid arthritis in four (14.3%) patients. The average body mass index (BMI) was 26.5 ± 6.7. There were seven males and 21 females in this series. All the patients had severe valgus deformity without medial collateral ligament incompetence in the coronal plane. In the sagittal plane, five knees had hyperextension and eight knees had fixed flexion deformity. The average arc of motion was 101.3 ± 23.8° preoperatively and 102.7 ± 11.8° postoperatively which was not statistically significant (p > 0.05).
The average preoperative LDFA was 81 ± 4.2°. The average preoperative MPTA was 94.9 ± 3.9°. The average preoperative tibial slope was 7.6 ± 3.4°. The residual valgus deformity in varus stress views was 196.6 ± 4.8° which is called surgical valgus and the average deformity in valgus stress views was 207.8 ± 7.4°. There were no patients with medial collateral ligament incompetence in this series. Nine knees had HKA less than 200° and 19 knees had severe valgus deformity with HKA more than 200°. There was significant improvement in HKA from 205.2 ± 8.3° preoperatively to 181.9 ± 3.7° postoperatively (p < 0.05).
Lateral parapatellar approach was used in 25 patients (89.2%) and medial parapatellar approach was used in three patients (10.8%). In patients with surgical valgus, less than 10° was operated upon through a medial parapatellar approach. All the patients underwent posterior stabilized prosthesis of PFC Sigma implants (DePuy, Indianapolis, IN). Patellar resurfacing was done in 22 (78.6%) knees. None of the patients had constrained implants. For managing the bone defects on femoral side, augments with femoral stem were used in 6 patients. On tibial side, stem extension alone was required in two knees, screws alone were used in five knees, and screws with tibial stem were used in three knees. For one patient, tibial diaphyseal osteotomy and plate osteosynthesis was done for associated extraarticular tibial deformity.
The mean union time of LFSO osteotomy fragment was 114 ± 19.1 days. At the final follow-up, bony union was noted in all the patients. There was a significant improvement in Oxford knee score from 15.1 ± 3.9 preoperatively to 40.3 ± 2.9 postoperatively (p < 0.05). There was significant improvement in preoperative KSS and KSS-F from 35.1 ± 10.6 and 26.6 ± 12.6 to 85.6 ± 4.8 and 89.4 ± 7.7 postoperatively (p < 0.05), respectively. One patient had acute periprosthetic joint infection, three weeks from the date of index surgery. She had culture negative prosthetic joint infection and was managed by debridement and polyethylene insert exchange with broad spectrum IV antibiotics for two months. There was no deep vein thrombosis, peroneal nerve palsy, postoperative periprosthetic fracture, or revision noted in the final follow-up.
Discussion
The key finding in our study was that LFSO helps in achieving the mediolateral balance in a predictable manner for fixed valgus deformity. It helps in deformity correction and also achieves satisfactory clinical and radiological outcome without the need for constrained implants.
Multiple techniques were described in the literature for the soft tissue balancing in valgus deformity. These include a lateral parapatellar approach that provides direct exposure of lateral and posterolateral structures, pie-crusting of lateral structures, lateral retinacular release, medial collateral ligament advancement, and use of constrained components [1, 2, 6]. Conjeski et al. reported that pie-crusting technique might not be adequate for achieving soft tissue balance for severe valgus deformities [2]. LCL and popliteus were the primary lateral stabilizers of the knee and its release leads to overcorrection and lateral instability in flexion [5,6,7]. LFSO allows controlled lengthening of the lateral tight structures, prevents over-release, and helps in achieving soft tissue balance [5].
The main indication for LFSO technique is Ranawat’s grade 2 valgus deformity, and it is insufficient in grade 3 deformity where there is incompetency of MCL [9]. Many authors used primary implants like cruciate-retaining [12] or posterior stabilized prosthesis [5, 7] after LFSO. Brilhault et al. suggested to use deep dish ultra-congruent TKA without post-cam box in osteopenic bone that allows to increase the thickness of bone block and subsequent screw fixation [13]. Conjeski et al. reported five out of twelve knees in their series had condylar lift-off in flexion and required semi-constrained prosthesis to avoid postoperative flexion instability [2]. In our series, we have used posterior stabilized knee in all the patients and we have not used any constrained implants.
Some authors described the role of computer navigation in precision and controlled release of lateral epicondylar block and accurate reposition of the fragment to allow equalization of medial and lateral gaps [5, 9, 12]. The concomitant extraarticular deformity was expected if preoperative LDFA was found to be less than 81° [4]. It was associated with valgus deformity due to hypoplasia of lateral femoral condyle or metaphyseal remodeling. It aggravates the existing valgus deformity and necessitates the need for extended release [14]. We also noted that extra-articular femoral deformity was commonly associated with valgus knees and needs to be compensated intra-articularly. If the extra-articular deformity is severe, it may need osteotomy at the center of rotation to obviate the need for extensive intra-articular soft tissue release [6].
The fixation technique of LFSO is varied in the literature. Internal fixation by screws gives immediate stability and prevents the displacement of bony fragment [4, 5, 7, 12]. Brilhault et al. suggested one-third tubular plate as a tension band if there is severe osteoporosis [7]. Some authors released only a shingle or sliver of lateral epicondylar bone, relied on the preserved periosteum and proximal soft tissues, and used no fixation for the osteotomy fragment [2, 8, 15]. They elucidated that the fragment displaces and stabilizes itself and has made no modification in the postoperative physical rehabilitation. We have always used screws to fix the fragment that helps in achieving immediate stability and allowing earlier full weight bearing mobilization. Also, after extensive posterolateral capsular release, the LFSO fragment becomes unstable and fixation of the fragment becomes necessary. In addition, the fixation of the fragment prevents lateral condylar lift-off in flexion.
The LFSO achieved an optimal soft tissue balance and excellent to good functional results and this has been described in the literature [2, 4, 5, 7,8,9, 12]. Conjeski et al. reported 12 knees with significant improvement in objective knee society score and functional score from 71 and 30 points preoperatively to 88 and 64 points postoperative period at a mean follow-up of 34 months [2]. Li et al. reported in 25 patients with significant improvement in knee society score from 36.5 to 89.1 and functional score from 40.8 to 86.3 postoperatively at a mean follow-up of 3.3 years [4]. Both reported transient peroneal nerve palsy in one patient in their series. Like previous studies, our series also showed a significant improvement in the functional scores at an average follow-up of 3.9 years in 28 patients. We have not noticed any peroneal nerve palsy in our series.
The complications reported are displacement of the osteotomized fragment that required revision surgery [9], transient peroneal nerve palsy [2, 4], wound complications [4, 9], deep vein thrombosis [2], infection [9], instability [9], and periprosthetic femur fracture [14]. In our experience, the factors which preclude the LFSO are the small bones in the short obese patients with concomitant osteoporosis where the osteotomy will compromise the stability of the lateral femoral condyle and in profound valgus deformity where the fragment needs to be mobilized distally beyond the distal femoral cut surface to achieve mediolateral balance [9]. One patient had acute prosthetic joint infection in our series which was managed by debridement and polyethylene insert exchange. This patient had no recurrence of infection and has good functional outcome in the follow-up.
The limitation of the study was the analysis of small cohort of patients. However, considering the relatively rare incidence and nature of the procedure, our series was equivalent to the reported case series in the literature. The follow-up is limited and further long-term follow-up of these patients is required to analyze the long-term outcomes with this procedure. Although the data was collected prospectively from our institution, the radiological parameters were calculated retrospectively. We have not taken any control group with usual sequential lateral release for analyzing the comparative outcomes. Nevertheless, we have analyzed the clinical and radiological outcomes of consecutive patients who underwent TKA with LFSO for severe valgus deformity from a single institution.
Conclusion
Lateral femoral sliding osteotomy is an effective technique for optimal soft tissue balance in fixed valgus deformity. It provides satisfactory clinical outcome with restoration of knee alignment without using the constrained implants.
Data availability
Not applicable.
Code availability
Not applicable.
References
Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S (2005) Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg 87:271–84. https://doi.org/10.2106/JBJS.E.00308
Conjeski JM, Scuderi GR (2018) Lateral femoral epicondylar osteotomy for correction of fixed valgus deformity in total knee arthroplasty: a technical note. J Arthroplasty 33(2):386–390. https://doi.org/10.1016/j.arth.2017.09.018
Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M (2014) Total knee arthroplasty in the valgus knee. Int Orthop 38(2):273–83
Li F, Liu N, Li Z, Wood KB, Tian H (2019) Lateral femoral sliding osteotomy in total knee arthroplasty with valgus deformity greater than twenty degrees. Int Orthop (SICOT) 43(11):2511–2517. https://doi.org/10.1007/s00264-019-04295-0
Mullaji AB, Shetty GM (2010) Lateral epicondylar osteotomy using computer navigation in total knee arthroplasty for rigid valgus deformities. J Arthroplasty 25(1):166–169. https://doi.org/10.1016/j.arth.2009.06.013
Lange J, Haas SB (2017) Correcting severe valgus deformity: taking out the knock. Bone Joint J 99-B(1_Supple_A):60–64. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0340.R1
Brilhault J, Lautman S, Favard L, Burdin P (2002) Lateral femoral sliding osteotomy. J Bone Joint Surg 84(8):7
Bustamante F, Correa-Valderrama A, Stangl-Herrera W et al (2021) Lateral epicondyle osteotomy for correction of valgus deformity during total knee arthroplasty: surgical technique and clinical outcomes. J Arthrosc Joint Surg 8(2):122–128. https://doi.org/10.1016/j.jajs.2020.11.001
Scior W, Hilber F, Hofstetter M, Graichen H (2018) Short-term and mid-term results of lateral condyle sliding osteotomy in the treatment of valgus total knee arthroplasty: a successful therapy option in Grade 2 valgus total knee arthroplasty. Knee 25(3):466–472. https://doi.org/10.1016/j.knee.2018.03.007
Murray DW, Fitzpatrick R, Rogers K et al (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89(8):1010–1014. https://doi.org/10.1302/0301-620X.89B8.19424
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13e4
Hadjicostas PT, Soucacos PN, Thielemann FW (2008) Computer-assisted osteotomy of the lateral femoral condyle with non-constrained total knee replacement in severe valgus knees. J Bone Joint Surg Br Vol 90-B(11):1441–1445. https://doi.org/10.1302/0301-620X.90B11.20092
Brilhault J, Burdin P (2012) TKA in the severe valgus knee: lateral epicondyle sliding osteotomy technique. In: The knee joint. Springer Paris; 907–913. https://doi.org/10.1007/978-2-287-99353-4_86
Stafeev DV, Chugaev DV, Lasunsky SA, Korniliv NN, Sineoky AD (2017) Efficiency and safety of sliding osteotomy of the lateral femoral condyle in total knee arthroplasty in patients with fixed valgus deformity (Krackow type III). Genij Ortopedii 23(3):314–322. https://doi.org/10.18019/1028-4427-2017-23-3-314-322
Raut V, Matar HE, Singh A (2020) Satisfactory medium-term outcomes with lateral condylar sliver osteotomy to correct valgus deformity in total knee replacements. Knee Surg Sports Traumatol Arthrosc 28(5):1394–1399. https://doi.org/10.1007/s00167-019-05488-1
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dhanasekararaja Palanisami, Soundarrajan Dhanasekaran, and Sandeep Kumar Kanugula. The first draft of the manuscript was written by Dhanasekararaja Palanisami and Soundarrajan Dhanasekaran and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Ethics Committee (IRB approval No: 13/12/2021).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1 and 2.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Palanisami, D., Dhanasekaran, S., Kanugula, S.K. et al. Outcomes of lateral femoral sliding osteotomy in primary total knee arthroplasty for type two fixed valgus deformity. International Orthopaedics (SICOT) 48, 111–117 (2024). https://doi.org/10.1007/s00264-023-05950-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05950-3