Abstract
Purpose
The aims of this study are to summarize (1) the history of terrible triad injury (TTi) treatment and (2) the clinical and biomechanical data that engendered its evolution.
Methods
A literature search was performed using five electronic databases. Results were discussed as a chronologic review of the relevant literature between 1920 and 2022.
Results
In 1962, Osborne was the first to describe a link between elbow dislocation, radial head fracture, and lateral collateral ligament complex injury via a novel mechanism: posterolateral rotatory instability (PLRI). Given that untreated elbow instability leads to post-traumatic osteoarthritis (PTOA), there has been increasing interest in elbow biomechanics since the 1980s. Data from studies in that period revolutionized the approach to elbow instability. The authors demonstrated that TTi could occur via a PLRI mechanism with a disruption of the lateral collateral ulnar ligament and a functionally competent anterior medial collateral ligament (aMCL). Since the 1990s, due to the difficulty in identifying its pathoanatomic features, some began to speculate about a sequence of injuries and mechanisms leading to TTi. However, the clinical literature has largely been unable to reproduce in vitro findings describing the pathomechanics of TTi. Some aspects of treatment remain controversial including systematic coronoid and aMCL repair.
Conclusion
Despite a growing body of biomechanics data, there is no widely accepted surgical protocol for the treatment of TTi. Functional outcomes among patients have greatly improved. Better diagnosis and treatment of infra-clinical instability after a TTi may be an important stepping stone to prevent the onset of moderate/severe PTOA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
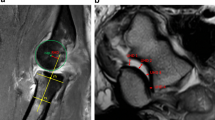
There has been lively debate regarding the injury mechanism and treatment rationale of terrible triad injuries for more than a century. Hotchkiss et al. [1] first defined an injury pattern involving the radial head and coronoid process in the setting of an elbow dislocation; they coined it “the terrible triad injury” (TTi) because of the poor treatment outcomes, including recurrent instability, stiffness, post-traumatic arthrosis, and chronic pain (Fig. 1).
Terrible triad injury of the elbow. In 1996, Hotchkiss et al. [1] defined an injury pattern involving fracture of radial head and coronoid process, in the setting of an elbow dislocation (black circles). The authors termed this injury “the terrible triad of the elbow.” Further study has led to the discovery that the lateral ulnar collateral ligament (LUCL), anterior band of the medial collateral ligament (aMCL), and/or the common flexor-pronator and extensor tendons (grey circles) are also frequently injured in TTs of the elbow. Furthermore, these latter injuries allow us to determine overall injury severity and can also help guide treatment
Improved understanding of the biomechanical contributions of ligaments and bones to elbow joint stability has led to improved midterm functional outcomes following treatment of TTi [2]. Based on the aforementioned biomechanical data, theories regarding injury sequence were developed, allowing surgeons to devise more reproducible treatment protocols [3]. However, clinical results following treatment of TTi have yet to reproduce in vitro findings, and no surgical protocol has been widely accepted.
There is a dearth of published literature to support surgical protocols and the mechanism leading to TTi. A more in-depth understanding of the injury mechanism would facilitate innovation with respect to therapeutic approach. Therefore, the aims of this study were to summarize (1) the history of TTi treatment, and (2) the clinical and biomechanical data that engendered its evolution.
Materials and methods
A literature search was performed using Ovid Medline, Ovid Embase, Scopus and Cochrane Library, and the Medical Subject Headings vocabulary. The search was limited to English and French language literature. The following terms were combined with “AND” and “OR”: “dislocation,” “terrible triad,” “unhappy triad,” “elbow,” “radial head fracture,” “coronoid,” and “elbow instability.” Due to the limited historical time frame inherent in these search engines, references from the existing literature were also queried. Results were reported as a chronologic review of the relevant literature between January 1920 and January 2022 (Fig. 2).
Results
Surgical discovery (1940–1980)
Treatment of the complex elbow dislocation at the beginning of the twentieth century was limited to closed reduction and non-surgical treatment, or radial head (RH) resection [4].
Ligamentous laxity and the deficiency in depth of the trochlear notch—primarily due to coronoid process height—were the two most popular theories to explain the recurrent instability after complex or simple elbow dislocation [5]. Initial surgical interventions were inspired by those performed for shoulder instability prior to Bankart repairs [5]. These interventions consisted of transfer of the biceps tendon to the coronoid process, coronoid bone block augmentation, or direct capsular repairs via an anterior approach [5]. All aimed to improve mechanical stability of the coronoid and prevent the humerus from disengaging with the trochlea. However, this treatment methodology led to a high-rate post-traumatic osteoarthritis (PTOA) (38–63%) [6]. Furthermore, heterotopic ossification and painful wrist deformities were frequently observed, irrespective of treatment modality. In 1941, Speed [7] was the first to describe the use of a vitallium (65% Co, 30% Cr, 5% Mo) cap (Fig. 2), placed over the radial neck, in order to prevent heterotopic bone formation and shortening of the proximal radius. In 1951, Essex-Lopresti et al. [8] demonstrated the important contribution of the RH to forearm stability. Based on these observations, they recommended the use of a RH implant in patients sustaining a distal radio-ulnar joint injury as well as a RH fracture. This injury pattern was later coined the Essex-Lopresti lesion based on the authors’ work. During the same year, Carr and Howard [9] demonstrated that replacing the RH led to improved elbow stability and decreased wrist deformation when compared to RH resection.
In 1964, Gutierrez et al. [10] described the insertions of the anterior (aMCL), posterior, and transverse bands of the medial collateral ligament onto the proximal ulna and the distal humerus. They posited that the aMCL could be the primary contributor to the valgus stability by limiting the progressive angular opening of the humeroulnar articulation. Two years later, Osborne et al. [5] were the first to describe a link between elbow dislocation, radial head fracture, and lateral collateral ligament complex (LCLC) injury. Based on a case series and literature review, they provided the first description of the mechanism of posterolateral rotatory instability (PLRI). The authors hypothesized that axial loading of the incompletely extended elbow, typically due to a fall on an outstretched hand, produced posterolateral rotation of the trochlea with respect to the humerus. The force of the fall was first transmitted up the forearm to the trochlear notch and coronoid process which strike the trochlea of the humerus, potentially fracturing the coronoid. In this position, the laterally sloping surface of the inner two-thirds of the trochlea, described as a “cam” by the authors, converted the vertical thrust into lateral rotation and valgus strain. Subsequently, the coronoid disengaged and the RH and ulna were displaced posteriorly then laterally, swinging on the intact biceps’ tendon until the coronoid disengaged and the RH became trapped behind the humerus. The proximal attachment of the LCLC was stripped away and the posterolateral capsule tears as the RH rotated posteriorly from the capitellar surface. The same authors [5] also demonstrated that LCLC repair prevented persistent elbow instability following TTi. The LCLC’s role in preventing PLRI was reinforced by data from Hassman in 1975 [11]. Despite Osborne’s recognition of the MCL’s contribution to elbow stability, they did not feel its repair was necessary to restore posterolateral stability. Instead, they recommended repair of the aMCL in cases of recurrent dislocation or persistent valgus instability after LCLC repair [5].
Biomechanical revolution (1975–1995)
As a result of the inability to restore stability without inducing PTOA, there has been increasing interest in elbow biomechanics since the 1980s. Data uncovered during this period revolutionized the approach to elbow instability.
In 1981, Tullos et al. [12] re-defined the three main stabilizers of the elbow: the RH, the coronoid process, and the aMCL. In 1989, Morrey and Regan [13] developed a new classification describing the extent to which the height of the coronoid contributes to elbow. The classification was based on the size of the fractured coronoid fragment (tip avulsion (I), < 50% (II), and > 50% (III)). They demonstrated that a fracture involving > 50% of the coronoid height led to elbow instability and only recommended reduction/fixation for type III fractures. This recommendation, however, did not take associated ligamentous and bony injuries into consideration.
In 1987, Josefsson et al. [14] identified MCL rupture in 100% of operatively treated simple elbow dislocations (n = 31). Shortly thereafter, Hotchkiss [15] and Morrey et al. [16] published additional data suggesting that the aMCL was the most critical stabilizer of elbow throughout the flexion–extension arc. Morrey et al. [17] also showed that its contribution to elbow stability increased in cases where the RH was resected. Conversely, TTi with comminuted RH fractures and a competent MCL could be treated with RH excision without the risk of altered elbow biomechanics. The authors recommended RH arthroplasty for non-reconstructable RH fractures with aMCL deficiency to prevent gross valgus instability. These results led the authors to classify the aMCL, LCLC, and humero-ulnar joint as the primary constraints to valgus stress, with the RH as a secondary constraint. However, this classification was based on uniplanar stress testing at a specific flexion–extension angle, and not combined or rotatory motions, thereby excluding PLRI.
In 1992, O’Driscoll et al. [3] showed that elbow dislocation through PLRI could occur via disruption of the lateral collateral ulnar ligament (LCUL) with a functionally competent aMCL. Based on a biomechanical study of 13 cadaveric upper extremities, the authors inferred that a deficient LCUL allowed for transient rotatory subluxation of the ulnohumeral joint, and secondary dislocation of the radio-humeral joint. The annular ligament and, therefore, the proximal radio-ulnar joint remained intact. This mechanism was consistent with that proposed by Osborne in 1968 [5]. O'Driscoll and colleagues [18] hypothesized that this pattern could be induced by an axial load combined with valgus (15°) stress, moderate internal rotation or hyper-supination (40°), and flexion (Fig. 3).
Controversies (1992–2020)
Based on their clinical experience, in 1996, Hotchkiss et al. [1] described an injury pattern involving the radial head and the coronoid process in the setting of a dislocated elbow and called it the terrible triad injury because of the poor reported outcomes, including recurrent instability, stiffness, post-traumatic arthrosis, and chronic pain (Fig. 1).
Unifying theories for TTI
As the result of the inability to explain pathoanatomic features of the TTi, some authors speculated about sequential injury to unify clinical finding and PRLI mechanism described by biomechanical studies. In 1992, O’Driscoll et al. [18] introduced the concept of the Horii circle to explain the spectrum of elbow instability. He described progressive soft tissue and bony injuries occurring sequentially from lateral to medial (Fig. 3). In stage 1 (PLRI), the LCUL was disrupted. In stage 2 (perched elbow), the other lateral ligamentous structures as well as anterior and/or posterior capsules were disrupted. In stage 3 (dislocated elbow), disruption of the posterior (a) and then anterior (b) MCL was identified. O’Driscoll posited that the aMCL remained intact in many TTi because fracture of the RH and coronoid process dissipated much of the energy prior to elbow dislocation. As a result, stabilization of the radio-capitellar joint via LCLC and RH reconstruction, along with coronoid repair, is almost always sufficient to restore stability following TTi. In 1998, Ring and Jupiter [23] re-classified the primary and secondary restraints of the elbow using a 4-column (i.e., anterior, posterior lateral, and medial columns) linkage theory (Figs. 2 and 3). The authors demonstrated decreasing elbow stability as more components of the ring were injured. They also speculated that, similar to pelvic ring injuries, if one part of the ring is injured, another injury (or break in the ring) should be sought. Based on this theory, repair of both injured columns is required to restore stability of the ring and prevent instability after TTi. Despite these observations, clinical and imaging studies reported a high incidence of MCL rupture in TTi [24]. Based on an online video investigation, Schreiber et al. [24] found that the most common injury mechanism involved a valgus moment applied to an extended elbow, which suggested a requisite primary disruption of the MCL. In 2012, Rhyou and colleagues [25] proposed a new unifying theory in which the injury began on the medial side, equivalent to a reverse Horii circle (Fig. 3). They hypothesized that an axial and valgus load was likely to rupture the MCL. This disruption, accompanied by pathologic hyper-supination, led to a lateral translational vector on the ulna. This vector led to elbow dislocation with simultaneous fracture of the RH and coronoid process. The stripping-type injury of the LCUL, induced by abutment of the RH against the posterior capitellum, ultimately ended in posterolateral (PL) dislocation. Five years later, a similar sequence was described by Robinson et al. [26]. In 2018, Luokkala et al. [27] proposed another potential injury sequence involving PL dislocation with soft tissue injuries progressing in a spiral pattern, starting on the medial side (Fig. 3). As the elbow went into hyperextension and valgus, the relatively stiff medial ligament complex failed. As the joint opened further, the lateral ligament complex, also stiffer than the tendons, failed next and then the common flexor origin. Further displacement led to failure of the anterior capsule and then the common extensor mass origin.
Surgical protocols
In 2005, McKee et al. [19] proposed a surgical protocol that would provide sufficient elbow stability to allow for early motion and faster functional recovery. Based on the principles of the Horii circle, the protocol included a systematic repair of coronoid fractures (regardless of size), then the RH fracture and finally LCLC were addressed via a single lateral approach. In cases of persistent instability, repair of the aMCL (and the flexor pronator mass if disrupted) or application of a hinged external fixator was recommended. This protocol led to excellent midterm functional outcomes [20]. Other protocols inspired by McKee’s work were also published [28]. These modifications included varied approaches (e.g., supplementary medial approach for coronoid fixation), differing definitions of persistent instability, and additional procedures (systematic ulnar nerve transposition, postoperative radiotherapy or indomethacin), none of which led to clinically improved outcomes when compared to McKee’s original strategy. Despite the success of an “all surgical” approach, biomechanical data challenged the belief that all coronoid fractures in TTi must be fixed [29]. O’Driscoll proposed a new classification system of coronoid fractures [21] that included the amount of coronoid fractured, as well as the anatomic location. In this system, a type 1 fracture involved the tip of the coronoid, a type 2 involved a fracture of the anteromedial facet of the coronoid, and type 3 involved a fracture of the coronoid at the base. This modified classification system directs treatment. Doonberg et al. [30] showed that 97% of TTi included coronoid fractures involving < 50% of the coronoid height. In 2012, Jeon et al. [22] demonstrated that coronoid fractures involving < 50% of the height with a competent LCLC and RH were clinically stable. This was confirmed by Papatheodorou et al. [31] in 2014. The same year, Hartzler et al. [29] demonstrated that fixation of a transverse coronoid fracture, involving 50% of the bony height, improved varus and internal rotatory laxity but was unlikely to meaningfully improve valgus or external rotation laxity. Based on these biomechanical findings, fixation of coronoid fractures was indicated using clinical (varus stress test) and/or radiographic (fracture > 50% of the coronoid height) parameters. Despite the use of biomechanically driven guidelines, the prevalence PTOA remained elevated at 11.2% and 66% at three and nine years, respectively [32]. Several studies have suggested that the development of PTOA could simply be due to the amount of energy dissipated by the joint at the time of injury [32]. Recently, Jung et al. [33] found that failing to repair a ruptured MCL significantly increased the risk of developing PTOA. Despite clinical studies demonstrating minimal impact of MCL repair at short- to midterm follow-up, some authors suggested that it may reduce the risk of PTOA in the long term [33]. In a biomechanical study by Eygendaal et al. [34], rupture of the MCL resulted in a 5.9-mm increase in medial joint space opening during valgus stress with the elbow at 90° of flexion. This could result in the development of PTOA due to sub-clinical elbow instability, as our clinical examinations have low sensitivity [35]. Jeong et al.’s [36] data support this hypothesis. They reported no cases of moderate or severe PTOA in 13 patients who underwent primary MCL repair at the time of surgical treatment of TTi. Literature describing the long-term clinical outcomes of TTi and the pathogenesis of PTOA was scarce. Further studies are necessary to assess the long-term effects of soft tissue and bony reconstruction on the development of PTOA.
Lesson learned
Many approaches to the treatment of TTi have been proposed and followed, but with little scientific evidence to support them. The clinical literature has been largely unable to reproduce in vitro findings regarding the injury mechanism that leads to TTi. However, for the last ten years, it has been widely accepted that the primary goal of surgery is to stabilize the radiocapitellar joint by repairing the lateral structures (RH and LCUL), and then to fix the coronoid fracture according to clinical (varus stress test) and/or radiographic (i.e., > 50% coronoid fracture) parameters. This management protocol allows surgeons to prevent immediate gross instability and has led to critical improvements in the functional outcomes. The terrible triad has become the sneaky triad of the elbow.
Data herein suggest that infra-clinical valgus instability, due to a deficient MCL, may explain the late onset of PTOA. Given the poor sensitivity of physical examination maneuvers, this subtle instability may be difficult to diagnose clinically. We reason, therefore, that the aMCL and coronoid fractures must be addressed in younger patients and overhead athletes to prevent late-onset PTOA. Protocols [19] focused only on the LCLC should be reserved for elderly and/or sedentary patients to allow for immediate gross elbow stability and faster functional recovery (Fig. 4).
Future directions
Understanding the link between soft tissue injuries and the onset of PTOA following TTi continues to be a challenge for elbow surgeons. The present review suggests that persistent subclinical instability may explain the observed PTOA in clinically stable elbows. We hypothesize that dynamic stabilizers of the elbow (muscles) may minimize the impact of MCL deficiency, and thus explain the apparent contradiction between its critical contribution to valgus stability in biomechanical studies [37], and the small impact of repair found in clinical studies [38]. Biomechanical studies have demonstrated that muscles crossing the elbow joint (FCU, ECU, brachialis, and anconeus) contribute to its dynamic stability [39]. However, most biomechanical models utilize static conditions and constant muscle forces. Improvement in the accuracy of these models, similar to what had been studied in the hip/knee literature, is necessary if we wish to better reproduce the in vivo environment. A variety of methods to deal with muscle redundancy (static or dynamic optimization, proportional-integral-derivative control, and electromyography) and ligament forces (deformable models and elastic foundation models) have been used to understand the dynamic structures that contribute to hip and knee stability [40]. A similar rigorous approach to elbow model validation needs to occur. In the future, computational models may aid us to better understand the in vivo loads under various dynamics conditions, and thus describe the dynamic attenuator effect of the elbow’s muscles.
Conclusions
In conclusion, despite a growing body of biomechanical evidence, there is no widely accepted surgical protocol for the treatment of TTi. Despite important improvements in functional outcomes, we have failed to prevent the onset of PTOA at long-term follow-up. A more detailed understanding of the dynamic contributions to elbow stability would allow for enhancements in our surgical protocols. Finally, better diagnosis and treatment of infra-clinical instability may be an important stepping stone to improved long-term clinical outcomes following treatment of TTi.
References
Hotchkiss RN (1996) Fractures and dislocations of the elbow In Rockwood CA. Jr, Green DP, Bucholz RW, Heckman JD. (eds) Rockwood and Green’s fractures in adults. 4th ed. Philadelphia, PA: Lippincott-Raven, vol 1, pp.929–1024
Chen H, Liu G, Wu L (2014) Complications of treating terrible triad injury of the elbow: a systematic review. PLoS One 9:e97476. https://doi.org/10.1371/journal.pone.0097476
O’Driscoll SW, Morrey BF, Korinek S, An KN (1992) Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res 280:186–197
Cutler CW (1926) Fractures of the head and neck of the radius. Ann Surg 83:267–278. https://doi.org/10.1097/00000658-192602000-00015
Osborne G, Cotterill P (1966) Recurrent dislocation of the elbow. J Bone Joint Surg Br 48-B:340–346. https://doi.org/10.1302/0301-620X.48B2.340
Josefsson PO, Gentz CF, Johnell O, Wendeberg B (1989) Dislocations of the elbow and intraarticular fractures. Clin Orthop Relat Res 246:126–130. https://doi.org/10.1097/00003086-198909000-00020
Speed K (1941) Ferrule caps for the head of the radius. Surg Gynecol Obstet 73:845–850
Essex-Lopresti P (1951) Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. J Bone Joint Surg Br 33B:244–247
Carr CR, Howard JW (1951) Metallic cap replacement of radial head following fracture. West J Surg Obstet Gynecol 59:539–546
Gutierrez LS (1964) A contribution to the study of the limiting factors of elbow extension. Cells Tissues Organs 56:146–156. https://doi.org/10.1159/000142499
Hassmann GC, Brunn F, Neer CS (1975) Recurrent dislocation of the elbow. J Bone Joint Surg Am 57:1080–1084
Tullos HS, Schwab G, Bennett JB, Woods GW (1981) Factors influencing elbow instability. Instr Course Lect 30:185–199
Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71:1348–1354
Josefsson PO, Johnell O, Wendeberg B (1987) Ligamentous injuries in dislocations of the elbow joint. Clin Orthop Relat Res 221:221–225
Hotchkiss RN, Weiland AJ (1987) Valgus stability of the elbow. J Orthop Res 5:372–377. https://doi.org/10.1002/jor.1100050309
Morrey BF, Tanaka S, An KN (1991) Valgus stability of the elbow. a definition of primary and secondary constraints. Clin Orthop Relat Res 265:187–195
Morrey BF, An K-N (1983) Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med 11:315–319. https://doi.org/10.1177/036354658301100506
O’Driscoll SW, Morrey BF, Korinek S, An KN (1992) Elbow subluxation and dislocation. a spectrum of instability. Clin Orthop Relat Res 280:186–197
McKee MD, Pugh DMW, Wild LM, et al (2005) Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg Am. 87 Suppl 1(Pt 1):22–32. https://doi.org/10.2106/JBJS.D.02933
Pugh DMW, Wild LM, Schemitsch EH et al (2004) Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 86:1122–1130. https://doi.org/10.2106/00004623-200406000-00002
O’Driscoll SW, Jupiter JB, Cohen MS et al (2003) Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 52:113–134
Jeon IH, Sanchez-Sotelo J, Zhao K et al (2012) The contribution of the coronoid and radial head to the stability of the elbow. J Bone Joint Surg Br 94-B:86–92. https://doi.org/10.1302/0301-620X.94B1.26530
Ring D, Jupiter JB (1998) Fracture-dislocation of the elbow. J Bone Joint Surg Am 80:566–580
Schreiber JJ, Warren RF, Hotchkiss RN, Daluiski A (2013) An online video investigation into the mechanism of elbow dislocation. J Hand Surg 38:488–494. https://doi.org/10.1016/j.jhsa.2012.12.017
Rhyou IH, Kim YS (2012) New mechanism of the posterior elbow dislocation. Knee Surg Sports Traumatol Arthrosc 20:2535–2541. https://doi.org/10.1007/s00167-011-1872-7
Robinson PM, Griffiths E, Watts AC (2017) Simple elbow dislocation. Shoulder Elb 9:195–204. https://doi.org/10.1177/1758573217694163
Luokkala T, Temperley D, Basu S et al (2019) Analysis of magnetic resonance imaging–confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elbow Surg 28:341–348. https://doi.org/10.1016/j.jse.2018.08.010
Gupta A, Barei D, Khwaja A, Beingessner D (2014) Single-staged treatment using a standardized protocol results in functional motion in the majority of patients with a terrible triad elbow injury. Clin Orthop Relat Res 472:2075–2083. https://doi.org/10.1007/s11999-014-3475-3
Hartzler RU, Llusa-Perez M, Steinmann SP et al (2014) Transverse coronoid fracture: when does it have to be fixed? Clin Orthop Relat Res 472:2068–2074. https://doi.org/10.1007/s11999-014-3477-1
Doornberg JN, Ring D (2006) Coronoid fracture patterns. J. Hand Surg 31:45–52. https://doi.org/10.1016/j.jhsa.2005.08.014
Papatheodorou LK, Rubright JH, Heim KA et al (2014) Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res 472:2084–2091. https://doi.org/10.1007/s11999-014-3471-7
Heijink A, Vanhees M, van den Ende K et al (2016) Biomechanical considerations in the pathogenesis of osteoarthritis of the elbow. Knee Surg Sports Traumatol Arthrosc 24:2313–2318. https://doi.org/10.1007/s00167-015-3518-7
Jung S-W, Kim D-H, Kang S-H et al (2019) Risk factors that influence subsequent recurrent instability in terrible triad injury of the elbow. J Orthop Trauma 33:250–255. https://doi.org/10.1097/BOT.0000000000001425
Eygendaal D, Olsen BS, Jensen SL et al (1999) Kinematics of partial and total ruptures of the medial collateral ligament of the elbow. J Shoulder Elbow Surg 8:612–616. https://doi.org/10.1016/S1058-2746(99)90099-X
Zwerus EL, Somford MP, Maissan F et al (2018) Physical examination of the elbow, what is the evidence? A systematic literature review. Br J Sports Med 52:1253–1260. https://doi.org/10.1136/bjsports-2016-096712
Jeong W-K, Oh J-K, Hwang J-H et al (2010) Results of terrible triads in the elbow: the advantage of primary restoration of medial structure. J Orthop Sci 15:612–619. https://doi.org/10.1007/s00776-010-1515-
Pichora JE, Fraser GS, Ferreira LF et al (2007) The effect of medial collateral ligament repair tension on elbow joint kinematics and stability. J Hand Surg 32:1210–1217. https://doi.org/10.1016/j.jhsa.2007.05.025
Pierrart J, Bégué T, Mansat P (2015) Terrible triad of the elbow: treatment protocol and outcome in a series of eighteen cases. Injury 46:S8–S12. https://doi.org/10.1016/S0020-1383(15)70004-5
Lin F, Kohli N, Perlmutter S et al (2007) Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg 16:795–802. https://doi.org/10.1016/j.jse.2007.03.024
Li J (2021) Development and validation of a finite-element musculoskeletal model incorporating a deformable contact model of the hip joint during gait. J Mech Behav Biomed Mater 113:104136. https://doi.org/10.1016/j.jmbbm.2020.104136
Author information
Authors and Affiliations
Contributions
• O. Bozon: conception and design, critical revisions, manuscript review
• S. Chrosciany: data acquisition, manuscript review.
• M. Loisel: data acquisition, manuscript review.
• Dellestable: data acquisition, manuscript review.
• L. Gubbiotti: data acquisition, manuscript review.
• R. Dumartinet-Gibaud: data acquisition, manuscript review.
• E. Obrecht: data acquisition, manuscript review.
• ME. Tibbo: data acquisition, manuscript review
• Sos: data acquisition, manuscript review.
• P. Laumonerie: conception and design, critical revisions, manuscript review, approved final version of paper, administration, study supervision
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. Informed consent was not needed for this literature review.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer None of the authors (Bozon Olivier, Chrosciany Sacha, Loisel Marie, Dellestable Arthur, Gubbiotti Laura, Dumartinet-Gibaud Raphaëlle, Obrecht Elise, Tibbo Meagan, Sos Clara, Laumonerie Pierre), or any member of their family, have received any financial remu-neration related to the subject of the article.
Rights and permissions
About this article
Cite this article
Bozon, O., Chrosciany, S., Loisel, M. et al. Terrible triad injury of the elbow: a historical perspective. International Orthopaedics (SICOT) 46, 2265–2272 (2022). https://doi.org/10.1007/s00264-022-05472-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05472-4