Abstract
Purpose
Tourniquets are routinely used in high tibial osteotomy (HTO). However, research on the necessity of tourniquets during HTO is lacking. This study was designed to investigate the necessity of tourniquets in HTO.
Methods
This was a prospective study that included patients who underwent HTO at the same hospital. The patients were randomised into Group A (non-tourniquet, n = 45) and Group B (tourniquet, n = 45). Same surgical techniques and haemostatic methods were used in the two groups.
Results
All patients were followed up for more than three months. There was no difference in operation time, and no intra-operative vascular or nerve damage occurred in either group. The hospital stay was shorter in group A than in group B (p < 0.05). There was no difference in post-operative blood loss, haemoglobin or haematocrit (p > 0.05). The post-operative visual analogue scale (VAS) pain scores and calf swelling were lower in group A (p < 0.05), and the early knee range of motion was higher in group A (p < 0.05). The use of morphine and the incidence of thigh complications were also lower in group A (p < 0.05). There was no difference in the VAS and knee function between the two groups at three months post-operatively (p > 0.05).
Conclusion
Tourniquet use during HTO does not reduce post-operative blood loss, operation time or intra-operative complications, but not using a tourniquet shortens the hospital stay and reduces the post-operative usage of morphine and tourniquet-related complications, which promotes early recovery of knee function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) is an effective surgical treatment for knee osteoarthritis with varus deformity [1,2,3]. For HTO, peri-operative blood loss is inevitable due to exposure of the osteotomy surface and may exceed 800 ml [4,5,6,7]. Therefore, most surgeons routinely use a tourniquet during HTO to reduce intra-operative blood loss and improve the visibility of the surgical field.
Similarly, in the past, joint surgeons applied a tourniquet during total knee arthroplasty (TKA). They believed that the use of a tourniquet reduced intra-operative blood loss and operation time [8, 9]. However, the widespread use of a tourniquet during TKA has become controversial and can cause some issues, such as limb swelling, pain and delayed wound healing [10, 11]. As the management of perioperative blood loss continues to improve, a growing body of evidence shows that not using a tourniquet is superior to using a tourniquet in terms of overall TKA outcome [14,15,16]. A tourniquet is still routinely used during HTO, and few studies have been conducted to investigate the benefits and necessity of the tourniquet during HTO [15]. Previous studies have shown that tranexamic acid (TXA) reduces post-operative blood loss in patients undergoing HTO [4, 7, 16]. Gelatine sponges can absorb blood that is several times their own weight, and the blood then solidifies in the sponge, thus achieving haemostasis. Gelatine sponges also help to control blood loss during HTO [17].
This study was designed to evaluate the effect of the use of a tourniquet during HTO on post-operative blood loss, the complication rate and early functional recovery of the affected limb. The hypothesis is that the use of a tourniquet during HTO is unnecessary because it does not reduce post-operative blood loss but aggravates post-operative swelling and pain and impedes early functional recovery.
Materials and methods
Patients
This prospective, randomised controlled study was approved by the local institutional review board (KYLL-2019042) and registered at ClinicalTrials.gov (NCT-04992533). All participants signed informed consent before the surgery. Patients undergoing HTO at the same hospital between November 2019 and May 2021 were judged against the following inclusion criteria: (1) knee medial compartment osteoarthritis and (2) unilateral HTO. The exclusion criteria were as follows: (1) other knee surgery within six months prior to HTO; (2) pre-operative anaemia (Hb < 100 g/l); (3) severe cardiovascular, hepatic, renal or haematopoietic diseases; (4) pre-operative coagulation abnormalities and (5) allergy to any of the study materials, including TXA. A computer-generated random number list prepared by an investigator with no clinical involvement in the trial was used to randomly divide patients into two groups, and an independent doctor performed the simple balanced randomisation (1:1) using sequentially sealed envelopes that contained a paper on which was written Group A or Group B. In group A, a tourniquet was used only during pre-operative arthroscopic exploration. In group B, a tourniquet was used during arthroscopic exploration and osteotomy. Group assignment was blinded to the floor staff, physical therapy staff and any of the other physician extenders involved in patient care. Group assignment was also blinded to the research staff performing the assessments.
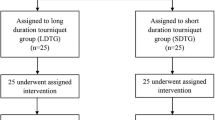
During this period, a total of 106 patients met the inclusion criteria, and 90 patients were eventually included in the study. Three months after the operation, there was no loss to follow-up in either group (see Fig. 1 for details).
Operation
All operations were performed by the same doctor, and all surgical procedures consisted of medial open wedge high tibial osteotomy (OWHTO). Before HTO, all patients underwent arthroscopic exploration to determine the need for partial meniscectomy. After general anaesthesia, an inflatable tourniquet was placed at the root of the thigh. The tourniquet system used was the Stryker Colour Cuff Dual Port inflated to 45 kPa. After proliferative synovia and meniscus tears were removed as needed, the tourniquet was then released in group A, while the tourniquet was kept in place in group B with the pressure maintained. OWHTO was performed according to the pre-operative plan, and biplane osteotomy was used. Artificial bone material beta-tricalcium phosphate (Olympus Terumo Biomaterials, Tokyo, Japan) was implanted at the osteotomy, and a TomoFix locking plate (DePuy Synthes, Zuchwil, Switzerland) was installed and fixed in place. One piece of an absorbable gelatine sponge (Xiangen, Jiangxi, China) was placed around the osteotomy. Before the incision was sutured, the tourniquet in group B patients was loosened.
Tranexamic acid protocol
In both groups, 30 min before surgery, 20 mg/kg TXA (KangEnbei Biopharmaceutical, Zhejiang, China) was dissolved in 100 ml of normal saline and administered intravenously. After the incision was closed, 2 g of TXA was dissolved in 30 ml of saline and injected into the osteotomy site. Three hours post-operatively, 2 g of TXA dissolved in 100 ml of natural saline was administered intravenously. The drainage tube was clamped for two hours after surgery and then opened.
Post-operative treatment
After the operation, all patients received the same pain management, including regular oral celecoxib (Ruihui, Dalian, China) and intravenous flurbiprofen axetil (Taide, Beijing, China). Morphine hydrochloride (Northeast Pharmaceutical Group, Shenyang, China) was given if there was still unbearable pain. The indications for patient discharge were as follows: (1) straight leg raise maintained for 30 s; (2) 90° knee flexion achievable and (3) no anaemia, fever, nausea, poor wound healing or other such complications.
Outcome measures
Intra-operative complications, opening angle, arthroscopic exploration time, tourniquet usage time, operation time and hospital stay were recorded. Total estimated blood loss was calculated by a formula described in previous studies [5, 18]. The drainage volume, haemoglobin and haematocrit on post-operative day three were assessed. Allogeneic blood was transfused if haemoglobin was < 80 g/L. The blood transfusion volume and the number of transfusions were recorded. Moreover, the number of patients who required morphine hydrochloride was also recorded. The knee range of motion (ROM), post-activity visual analogue scale (VAS) score for pain and maximum calf circumference were recorded on post-operative days one, three and five. Thigh complications (thigh pain, numbness and blisters), incision complications (incision infection, haematoma and delayed healing) and thrombotic complications were recorded. At post-operative month three, the VAS score and the Hospital for Special Surgery (HSS) knee score were obtained and recorded. All evaluations were conducted and reviewed by the same investigator who had received relevant training and was unaware of the allocation. Data analysts were also unaware of the allocation.
Statistical analysis
Sample size calculations were performed using the PASS 2011 (NCSS, LLC, Kaysville, UT) software. In a study by Li et al. [17], the post-operative VAS score was 5.47 on the day after surgery. To detect a 1.5-score difference in the primary outcomes, with a power of 0.90 and a significance level of 0.05, 18 patients per arm were needed. With the dropout rate assumed to be 20%, at least 23 patients per arm need to be included in the study. The SPSS 23.0 (SPSS, Chicago, IL, USA) software was used. The measurement data are expressed as the mean ± standard deviation, the count data are represented by the number of cases and the measurement data were subjected to the Levene variance equivalence test. The independent samples t test was used to compare the measurement data between groups, and the chi-squared test was used to compare the rates between groups. p < 0.05 was considered statistically significant.
Results
Baseline characteristics were not significantly different (p > 0.05) between the two groups. See Table 1 for details.
Post-operative general assessments
No significant between-group difference was observed in the arthroscopic exploration time. The tourniquet usage time was 26.18 ± 6.10 minutes in group A and 98.07 ± 14.36 minutes in group B (p < 0.05). However, no significant between-group difference was observed in the operation time (p > 0.05). There was no difference in total blood loss, drainage volume, haemoglobin or haematocrit on the third day after the operation (p > 0.05). No transfusion events or intra-operative vascular or nerve damage occurred in either group. The hospital stay was shorter in group A than in group B (p < 0.05). See Tables 2 and 3 for details.
Recovery of knee function
The VAS score was significantly lower in group A on post-operative days one, three and five (p < 0.05). Correspondingly, only seven patients in group A required morphine, while 16 patients in group B required morphine (p < 0.05). Knee ROM was better in group A on post-operative days one, three and five (p < 0.05). Calf circumference was smaller in group A on post-operative days three and five (p < 0.05). At post-operative month three, no significant between-group difference was observed in calf circumference, knee ROM, VAS score or HSS score (p > 0.05). See Table 2 and Figs. 2, 3, 4 for details.
Changes in calf circumference during the peri-operative period. The calf circumference in both groups reached a peak on the third day after surgery. The calf circumference of group A was significantly less than that of group B on post-operative days 3 and 5 (p < 0.05). Group A = patients without tourniquets, group B = patients with tourniquets
Post-operative complications
The incidence of thigh complications in group A was lower than that in group B (p < 0.05). Two patients in each group developed deep vein thrombosis (DVT; intramuscular venous thrombosis based on lower limb vascular ultrasound), and no pulmonary embolisms occurred in this study (p > 0.05). No significant between-group difference was observed in incision complications (p > 0.05). In group A, one patient had delayed wound healing, and one patient had incision oozing and delayed healing due to suture hypersensitivity. In group B, six patients had incision complications, including four cases of delayed healing and two cases of subcutaneous haematoma. Group A patients with suture hypersensitivity were readmitted on day 20 after the operation to resuture the incision. See Table 3 for details.
Discussion
In this study, the most important finding is that tourniquet use during HTO did not reduce post-operative blood loss, operation time or hospital stay and that not using a tourniquet promotes early recovery of knee function and reduces tourniquet-related complications. While some researchers have investigated the effect of tourniquets on the incidence of DVT after HTO [15], this study is one of the few prospective, randomised, controlled studies on the effect of tourniquets on blood loss, knee function and complications after HTO.
Researchers are still debating whether the use of tourniquets reduces post-operative blood loss. Yi et al. [8] conducted a meta-analysis of 859 patients and found that the use of tourniquets significantly reduced operation times and intra-operative blood loss but increased drainage and post-operative blood loss in TKA patients. Matzioli et al. [19] retrospectively analysed the clinical data of 574 patients and found that the use of a tourniquet before closing the incision during TKA significantly reduced peri-operative total blood loss but had no effect on the post-operative transfusion rate. With the standardised use of TXA in orthopaedic surgery, an increasing number of researchers believe that the use of a tourniquet during TKA is not necessary for reducing surgical blood loss [12,13,14]. Previous studies have shown that TXA reduces blood loss after HTO [4,5,6,7]. In this study, we administered TXA intravenously and topically and found no significant between-group difference in total blood loss, drainage or post-operative haemoglobin or haematocrit, suggesting that the use of a tourniquet during HTO does not reduce blood loss. Another purpose of a tourniquet is to increase the visibility of the surgical field to improve surgical safety and speed [8, 9]. However, this study found that while the operation time was slightly longer in group A (no tourniquet use during HTO), the difference did not reach statistical significance. Moreover, no intra-operative vascular or nerve damage occurred in this study, suggesting that not using a tourniquet during HTO is safe and does not increase the operation time or affect the visibility of the surgical field or surgical safety.
For post-operative function, Guler et al. followed up patients for a month after TKA and found that in the tourniquet group, there was a 20% loss of quadriceps muscle mass in the affected limb relative to the unaffected limb; this did not occur in the non-tourniquet group [20]. Dennis et al. found that in patients with bilateral TKA, muscle weakness lasted three months after operation in the limb on which a tourniquet was used but did not occur in the limb on which a tourniquet was not used [21]. Moreover, the use of tourniquets leads to the release of a large quantity of cytokines, thus aggravating post-operative pain and increasing incision complications [13]. TXA, by contrast, reduces fibrinolytic activity and surgical trauma due to blood loss. TXA also has anti-inflammatory effects that help reduce adverse outcomes due to the use of a tourniquet [22].
A growing body of evidence indicates that the use of a tourniquet contributes to postoperative limb pain. This study showed that the VAS score was lower on days one, three and five in group A (no tourniquet use) than in group B and that few patients in group A required morphine hydrochloride, suggesting that not using a tourniquet during HTO helps reduce pain during early recovery. Huang et al. conducted a prospective randomised controlled trial and found that not using a tourniquet reduced the VAS score on early post-operative days [13]. The use of a tourniquet causes prolonged lower limb vascular ischaemia and hypoxia, which stimulate the release of endothelial plasminogen activator, resulting in massive fibrinolysis and impeded thrombosis. Fibrinolysis continues even after a tourniquet is released, and the high fibrinolytic state may last for an extended period of time. Moreover, sudden venous perfusion of the lower limb greatly increases post-operative blood loss and aggravates limb swelling [23]. This study showed that calf circumference was larger on post-operative days three and five in group B than in group A, with no significant between-group difference on post-operative day one, a finding that may be related to the use of a drainage tube on post-operative day one. Previous studies have shown that a drainage tube significantly reduces limb swelling after HTO; however, the prolonged use of a drainage tube increases the risk of deep infections and affects post-operative functional exercise [17].
Tourniquet compression may cause damage to the vascular endothelium of the compressed area, block venous return and cause blood stasis, thereby aggravating the hypercoagulable state [24]. Hernandez et al. showed that the prolonged use of a tourniquet for more than 120 minutes during TKA increased the risk of proximal DVT [25]. Incision complications are common after HTO [26]. This study found that the incidence of incision complications was higher in group B than in group A; the difference did not reach statistical significance, but we believe that this was due to the small sample size in this study. In group A, a tourniquet was used only during arthroscopic exploration and for a short period of time. As a result, the incidence of tourniquet-related thigh complications was significantly lower in group A.
This study has some limitations. First, the sample size was small, with many comparative analyses, which increases the chance of errors. Second, the surgeons were aware of the allocation due to the nature of this study, which is a common issue in orthopaedic studies. Third, some patients did not undergo post-operative lower limb vascular ultrasound due to cost or insurance coverage. The exam was performed only in patients with suspected thrombosis, which may affect the results for the actual incidence of thrombosis. Moreover, due to the short follow-up period, we did not perform detailed analyses of infections, delayed healing at the osteotomy site, long-term knee function or survival.
Despite these limitations, the results from this study demonstrate that not using a tourniquet during HTO does not increase post-operative blood loss, operation time or intra-operative complications. It reduces the hospital stay, post-operative morphine use and tourniquet-related complications, which contribute to early knee recovery. Therefore, tourniquets should not be routinely used during HTO.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
19 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00264-021-05297-7
References
Hernigou P, Giber D, Dubory A, Auregan JC (2020) Safety of simultaneous versus staged bilateral opening-wedge high tibial osteotomy with locked plate and immediate weight bearing. Int Orthop 44(1):109–117. https://doi.org/10.1007/s00264-019-04385-z
Lee SH, Seo HY, Lim JH, Kim MG, Seon JK (2021) Higher survival rate in total knee arthroplasty after high tibial osteotomy than that after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06641-5
Schuster P, Gesslein M, Schlumberger M, Mayer P, Mayr R, Oremek D, Frank S, Schulz-Jahrsdorfer M, Richter J (2018) Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med 46(6):1362–1370. https://doi.org/10.1177/0363546518758016
Kim KI, Kim HJ, Kim GB, Bae SH (2018) Tranexamic acid is effective for blood management in open-wedge high tibial osteotomy. Orthop Traumatol Surg Res 104(7):1003–1007. https://doi.org/10.1016/j.otsr.2018.07.019
Palanisamy JV, Das S, Moon KH, Kim DH, Kim TK (2018) Intravenous tranexamic acid reduces postoperative blood loss after high tibial osteotomy. Clin Orthop Relat Res 476(11):2148–2154. https://doi.org/10.1097/CORR.0000000000000378
Li S, Lu Q, Guo X, Zhang M, Miao Z, Luo D, Liu P (2020) Intravenous combined with topical tranexamic acid administration has no additional benefits compared with intravenous administration alone in high tibial osteotomy: a retrospective case-control study. Orthop Surg 12(2):515–523. https://doi.org/10.1111/os.12652
Yao RZ, Gao WQ, Wang BW, Wang GL, Wu CX, A-Mu YD, (2019) Efficacy and safety of tranexamic acid in reducing blood loss of lower extremity osteotomy in peri-acetabulum and high tibia: a systematic review and meta-analysis. Orthop Surg 11(4):545–551. https://doi.org/10.1111/os.12515
Yi S, Tan J, Chen C, Chen H, Huang W (2014) The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 134(10):1469–1476. https://doi.org/10.1007/s00402-014-2056-y
Ozkunt O, Sariyilmaz K, Gemalmaz HC, Dikici F (2018) The effect of tourniquet usage on cement penetration in total knee arthroplasty: a prospective randomized study of 3 methods. Medicine (Baltimore) 97(4):e9668. https://doi.org/10.1097/MD.0000000000009668
Ryu KJ (2016) CORR Insights((R)): Does tourniquet use in TKA affect recovery of lower extremity strength and function? A randomized trial. Clin Orthop Relat Res 474(1):78–80. https://doi.org/10.1007/s11999-015-4436-1
Heller S, Chen A, Restrepo C, Albert E, Hozack WJ (2015) Tourniquet release prior to dressing application reduces blistering following total knee arthroplasty. J Arthroplasty 30(7):1207–1210. https://doi.org/10.1016/j.arth.2015.02.035
Xie J, Ma J, Yao H, Yue C, Pei F (2016) Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss after primary total knee arthroplasty without tourniquet: a randomized clinical trial. J Arthroplasty 31(11):2458–2464. https://doi.org/10.1016/j.arth.2016.04.034
Huang Z, Xie X, Li L, Huang Q, Ma J, Shen B, Kraus VB, Pei F (2017) Intravenous and topical tranexamic acid alone are superior to tourniquet use for primary total knee arthroplasty: a prospective, randomized controlled trial. J Bone Joint Surg Am 99(24):2053–2061. https://doi.org/10.2106/JBJS.16.01525
Yue C, Kang P, Yang P, Xie J, Pei F (2014) Topical application of tranexamic acid in primary total hip arthroplasty: a randomized double-blind controlled trial. J Arthroplasty 29(12):2452–2456. https://doi.org/10.1016/j.arth.2014.03.032
Motycka T, Eggerth G, Landsiedl F (2000) The incidence of thrombosis in high tibial osteotomies with and without the use of a tourniquet. Arch Orthop Trauma Surg 120(3–4):157–159. https://doi.org/10.1007/s004020050034
Suh DW, Kyung BS, Han SB, Cheong K, Lee WH (2018) Efficacy of tranexamic acid for hemostasis in patients undergoing high tibial osteotomy. J Knee Surg 31(1):50–55. https://doi.org/10.1055/s-0037-1600091
Li S, Yang J, Watson C, Lu Q, Zhang M, Miao Z, Luo D, Liu P (2020) Drainage relieves pain without increasing post-operative blood loss in high tibial osteotomy: a prospective randomized controlled study. Int Orthop 44(6):1037–1043. https://doi.org/10.1007/s00264-020-04530-z
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Matziolis D, Perka C, Hube R, Matziolis G (2011) Influence of tourniquet ischemia on perioperative blood loss after total knee arthroplasty. Orthopade 40(2):178–182. https://doi.org/10.1007/s00132-010-1727-9
Guler O, Mahirogullari M, Isyar M, Piskin A, Yalcin S, Mutlu S, Sahin B (2016) Comparison of quadriceps muscle volume after unilateral total knee arthroplasty with and without tourniquet use. Knee Surg Sports Traumatol Arthrosc 24(8):2595–2605. https://doi.org/10.1007/s00167-015-3872-5
Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE (2016) Does tourniquet use in TKA affect recovery of lower extremity strength and function? A randomized trial. Clin Orthop Relat Res 474(1):69–77. https://doi.org/10.1007/s11999-015-4393-8
Jimenez JJ, Iribarren JL, Lorente L, Rodriguez JM, Hernandez D, Nassar I, Perez R, Brouard M, Milena A, Martinez R, Mora ML (2007) Tranexamic acid attenuates inflammatory response in cardiopulmonary bypass surgery through blockade of fibrinolysis: a case control study followed by a randomized double-blind controlled trial. Crit Care 11(6):R117. https://doi.org/10.1186/cc6173
Zhou K, Wang H, Li J, Wang D, Zhou Z, Pei F (2017) Non-drainage versus drainage in tourniquet-free knee arthroplasty: a prospective trial. Anz J Surg 87(12):1048–1052. https://doi.org/10.1111/ans.14183
Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M (2000) Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res 371:169–177. https://doi.org/10.1097/00003086-200002000-00021
Hernandez AJ, Almeida AM, Favaro E, Sguizzato GT (2012) The influence of tourniquet use and operative time on the incidence of deep vein thrombosis in total knee arthroplasty. Clinics (Sao Paulo) 67(9):1053–1057. https://doi.org/10.6061/clinics/2012(09)12
Martin R, Birmingham TB, Willits K, Litchfield R, Lebel ME, Giffin JR (2014) Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 42(5):1118–1126. https://doi.org/10.1177/0363546514525929
Acknowledgements
The authors are grateful to the patients that were willing to participate in the study.
Funding
This work was funded by the Natural Science Foundation of Shandong Province (ZR2020MH278), the Horizontal project of Shandong University (12671818) and the Rongxiang Regenerative Medicine Foundation of Shandong University (2019SDRX-17).
Author information
Authors and Affiliations
Contributions
All authors contributed to either the conception, design, data collection or analysis. Songlin Li, Wenwei Qian and Peilai Liu were responsible for conception and design of the study. Songlin Li, Xiangshuai Zhang and Qunshan Lu drafted the manuscript. Mingxing Liu, Desu Luo, Kaifei Han and Lei Li contributed to data collection. Songlin Li, Mingxing Liu, YangYu and Zhuang Miao contributed to manuscript preparation and data analysis. Peilai Liu and Wenwei Qian contributed to revision of the manuscript. All authors read and approved the final manuscript. Wenwei Qian and Peilai Liu contribute equally to the work and should be regarded as co-corresponding authors.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This trial was approved by the ethics committee of a local hospital (KYLL-2019042) and registered at ClinicalTrials.gov, number NCT-04992533.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised. The correct copyright should be “The Author(s) under exclusive licence to SICOT aisbl.”
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, S., Zhang, X., Liu, M. et al. Not using a tourniquet is superior to tourniquet use for high tibial osteotomy: a prospective, randomised controlled trial. International Orthopaedics (SICOT) 46, 823–829 (2022). https://doi.org/10.1007/s00264-021-05246-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05246-4