Abstract
Purpose
We evaluated and compared kinematics of bilateral ankle, knee, and hip joints in patients with chronic unilateral ankle instability (CAI) with healthy controls.
Methods
Fifteen individuals diagnosed with CAI and a control group of 16 individuals were matched. Different peaks within the gait cycle (at different intervals) for the dorsiplantar, inversion/eversion, and abduction/adduction axis were compared between injured and uninjured sides of patients with CAI with a control group.
Results
Comparison of the uninjured ankle in CAI with the control group showed higher dorsiflexion in one peak of the stance phase (p = 0.003), higher inversion in one peak of the stance phase (p = 0.022), and the swing phase (p = 0.004). The hip joint of the uninjured side showed higher extension in one peak of the stance phase (p < 0.001), and two peaks of the swing phase (p < 0.05). Furthermore, it showed higher adduction in one peak of the foot flat to mid-stance phase (p = 0.001), higher abduction in one peak of the late swing phase (p = 0.047), and the swing phase (p = 0.032). The knee joint of the uninjured side showed higher flexion in all measured peaks of the gait cycle (p < 0.05) (except for one peak in the late swing phase) compared to the control group.
Conclusion
Chronic ankle instability results in altered biomechanics of the ipsilateral knee as well as the contralateral ankle, knee, and hip joints. The alterations caused by CAI may predispose patients to overuse and/or acute injuries of other joints of lower extremities during routine and sporting activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle sprains are among the most common types of injuries in sports worldwide [1]. Some patients experience residual symptoms and repeated sprains [2,3,4], and a number of these individuals go on to develop chronic ankle instability (CAI) [5]; it is well documented that CAI patients can be prone to long-term degenerative changes of the ankle joint [6]. What is less well understood or documented, however, is the fact that CAI may also be associated with multiple biomechanical changes in other lower extremity joints that predispose the individual to repeated sprain or other repetitive use injuries. Some of these changes which have been documented include alterations in muscle strength [7], postural control, increase in inversion of the ankle joint [8], and restrictions in dorsi/plantar flexion of the ankle joint [9]. Most studies to date have focused exclusively on the kinetic and kinematic changes at the injured side [10].
The purpose of this study was to evaluate and compare the kinematics of bilateral ankle and knee and hip joints in patients with unilateral CAI and compare these findings with healthy controls. We hypothesized that CAI not only affects biomechanics of the injured ankle but also affects biomechanics of the knee and hip joints of the ipsilateral and contralateral sides.
Methods
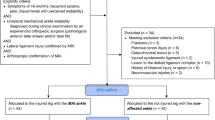
A total of fifteen individuals with CAI in their right leg who were above 18 years old and were randomly selected (using simple random sampling) to enter the study. Any individual who was pregnant, had fracture or surgery on the lower extremity, neuromuscular and musculoskeletal disorders, psychiatric disorders which would inhibit their cooperation with the researchers, or any individual receiving any treatment for their CAI during the study period was excluded from the study.
Chronic ankle instability was defined as having a history of at least one ankle sprain more than 12 months and having symptoms including giving way and/or recurrent sprains and/or a feeling of instability within their ankle joint for more than six months prior to inclusion in this study, according to the International Ankle Consortium [11]. These patients had no other injuries to the lower extremity other than the ankle joint. Ankle sprains were diagnosed according to physical examination, radiography, and MRI confirmation. These individuals were then referred to a biomechanics laboratory for gait assessment. A control group consisting of sixteen individuals older than 18 years old, without any history of injury or surgery to the lower extremity, was randomly selected.
Gait and motion analysis
After each individual gave their informed consent to enter the study, data on anthropometric indices and baseline characteristics of study participants were documented. Individuals were asked to walk on a straight path in their normal state wearing minimal clothing and bare-footed. Three-dimensional kinematic information during the gait cycle was collected using a 6 Vicon® motion capture system (Vicon, Oxford, UK). Fixed markers were placed on each individual anatomical landmarks according to the Vicon® Plug-in-Gait model [12].
First, individuals were asked to walk in their usual state a few times after which each individual was asked to walk the path five times, and a mean of the total measurements was considered for that individual. Ankle changes were assessed in eversion-inversion and dorsi/plantar flexion. Knee joint changes were assessed in flexion–extension, abduction, and adduction; the hip joint changes were assessed in flexion–extension, abduction, and adduction.
After collection of kinematic data from the Vicon cameras, data were transferred to the MATLAB software, version R2015b (the MatchWorks, Inc., Natick, Massachusetts, USA).
Instruments
Six Vicon® three-dimensional cameras were set at 120 Hz using the Nexus software (version 2.5). Every kinematic data acquired was first normalized. Moreover, for calibration, an L-frame (Ergocal—14-mm markers; Vicon) and calibration wand (240-mm wand to 14-mm markers, Vicon, Oxford, UK) were utilized.
Explanatory and outcome variables
Data on age, sex, and body mass index was obtained from each individual. The primary outcome of this study was measured as peak, which indicates the degree of changes in a specified joint within a specific axis (dorsi/plantar flexion, inversion/eversion, or abduction/adduction) during the gait cycle. For the ankle joint, seven peaks were considered on the dorsi/plantar flexion axis of movement, and six peaks were considered in the inversion and eversion axis of movement within the gate cycle. As for the hip joint, five peaks were considered on the flexion–extension axis, and six peaks were considered on the abduction–adduction axis within the gate cycle. For the knee joint, six peaks were considered on the flexion–extension axis, and six peaks were considered on the abduction–adduction axis within the gate cycle.
Within the dorsi/plantar flexion axis of the ankle, the predefined peaks “a” and “b” represent heel contact to foot flat. Peaks “c” and “d” represent heal-off to toe-off. Peak “e” represents early swing. Peak “f” represents mid-swing, and peak “g” represents heal contact. Within the inversion eversion axis of the ankle, peak a represents heal contact to foot flat, and peak b foot flat to mid-stance. Peak c pushes-off phase (between heal-off and toe-off), peak d early swing, peak e mid-swing, and peak f heal contact of the gait cycle.
Within the hip joint, for the abduction–adduction axis, peak a represents heal contact, peak b is foot flat to mid-stance, peaks c and d are in the push-off phase (c is the toe-off), and e and f are in the late swing phase. For the flexion and extension axis, peak a represents heal contact, peak b is in the push-off, peak c is the toe-off phase, and peaks d and e are in the late swing phase of the gait cycle.
Within the knee joint, for the abduction and adduction axis, peak a represents heal contact, peak b is foot flat to mid-stance, peaks c and d are in the push-off phase (c is the toe-off), and e and f are in the late swing phase. For the flexion–extension axis, peak a represents heal contact to foot flat. Peak b is the push-off phase and peak c is the toe-off, and peaks d and e are in the late swing phase (Fig. 1).
Sample size calculation
In order to test the null hypothesis of our study, that there is no difference between dorsiplantar flexion in the ankle joint of individuals with CAI and the control group; a T-test was used with a patient to control ratio of 1:1. In order to achieve a 90% statistical power for detecting a difference of 7.2 (SD = 0.5) [13], degrees in dorsi/plantar flexion during gait between patients with CAI and healthy control, with a two-tailed type-1 error of 5%, we will need a minimum sample size of one individual in each group. As the required sample size was very small, we decreased the effect size (mean difference) to 2°, with the previous presumptions and a 20% loss to follow-up expected, and accordingly, we will need to achieve a minimum sample size of 22 individuals (11 in the CAI group and 11 in the control group).
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) for windows, version 26. Qualitative variables were compared between two groups using the chi-square test. Quantitative variables with normal distribution were compared using the independent T-test. A p-value of less than 0.05 was considered statistically significant.
Results
The CAI and control groups consisted of fifteen and sixteen individuals, respectively. Baseline characteristics of the two groups were similar and are shown in Table 1.
Ankle joint
The injured ankle among patients with CAI showed higher dorsiflexion in one measured peak (peak b, p = 0.024) of the stance phase and one peak of the swing phase (peak g, p = 0.049) and a higher plantar flexion in one peak of the stance phase (peak d) of the gate cycle compared to the ipsilateral ankle of a healthy individual. Moreover, the injured ankle showed higher eversion in all measured peaks of the gait cycle (< 0.05) except for one peak in the mid-swing phase (peak f, p = 0.062).
Comparison of the uninjured ankle of the patient with CAI with that of the ipsilateral ankle of a healthy individual showed a higher tendency towards dorsiflexion in one peak of the stance phase (peak b, p = 0.003)) and a higher tendency towards inversion in one peak of the stance phase (peak a) and one measured peak in the swing phase (peak e, p = 0.027)).
Comparing the injured ankle with the contralateral side showed that the injured joint had a higher dorsiflexion in three peaks of the stance phase, including one peak at the heel contact to foot flat (peaks a, p = 0.019), two peaks at the heal-off to toe-off (peak c, p = 0.046; peak d, p = 0.002), and two peaks of the swing phase including one peak at the swing phase (peaks e, p = 0.017), and one peak at heel contact (peak g, p < 0.001). However, the injured ankle had more plantar flexion in one measured peak of the swing phase (peak f, p = 0.001) (Table 2) (Fig. 2).
Hip joint
The ipsilateral hip joints of patients with CAI showed higher extension in one peak at heal contact (peaks a, p < 0.001), one peak in the foot flat to mid-stance phase (peak b, p < 0.001), one peak of the push-off phase (peaks d, p < 0.001), and one peak of the late swing phase (peak e, p < 0.001) (p < 0.001) compared to the control group. Moreover, the ipsilateral hip joints of patients with CAI showed higher abduction in all evaluated peaks of the gait cycle compared to the control group (p < 0.05).
On the uninjured sides of patients with CAI, the hip showed higher extension in one measured peak at heel contact (peak a, p < 0.001), one peak at the push-off phase (peak d, p = 0.032), and one peak in the late swing phase (peak e, p = 0.001) compared to the ipsilateral hip of a healthy individual. The uninjured hip further showed higher adduction in one of the evaluated peaks of the foot flat to mid-stance phase (peak b, p = 0.001) and higher abduction in one peak of the late swing phase (peak f, p = 0.047) and showed higher abduction in one evaluated peak of the swing phase (peak d, p = 0.032).
Ipsilateral sided hip joints showed higher abduction in measured points of the gait cycle compared to those on the contralateral side of patients with CAI (p < 0.05) (Table 3) (Fig. 3).
Knee
The ipsilateral knee of the patient with CAI showed higher flexion in one measured peak at heel contact (peak a, p < 0.001), one peak at foot flat to mid-stance (peak b, p < 0.001), and two peaks of the push-off phase (peak c, p < 0.001; peak d, p = 0.002), and one peak of the late swing phase (peak f, p = 0.023) compared to the ipsilateral knee of a control group. Moreover, it showed higher abduction in all measured peaks of the gait cycle (except for one peak in the late swing phase) (peak e, p = 0.317).
The knee on the uninjured side showed higher flexion in all measured peaks of the gait cycle (except for one peak in the late swing phase) (peak f, p = 0.091) compared to the ipsilateral knee of a control group.
The injured knee showed higher abduction in all measured peaks (p < 0.05), except for two peaks measured in the push-off and late swing phase (peak d, p = 0.220; and peak e, p = 0.342), of the gait cycle, compared to the uninjured knee (Table 4) (Fig. 4).
Discussion
The purpose of this study was to evaluate and compare the kinematics of bilateral ankle, knee, and hip joints in patients with isolated, unilateral CAI and compare these findings to those of healthy controls. The results suggest that the presence of unilateral CAI alters kinematics not only in other major adjacent joints of the ipsilateral lower extremity but also of those in the uninjured side when compared to the kinematics of otherwise healthy, unaffected individuals.
Previous studies have reported neuromuscular and biomechanical changes that occur within the lower extremity joints of patient with CAI on the side of injury. In a gait analysis study, Koldenhoven et al. [10] evaluated and compared gait kinematics of the ankle, knee, and hip joints between 18 individuals with CAI and 18 copers. Kinematic outcomes were measured using a Vicon motion analysis system and compared between the two groups. The authors found that those with CAI showed higher inversion in the ankle joint during initial contact (3.3 ± 3.4 and − 1.1 ± 4.6 for the CAI and cooper groups, respectively; p = 0.048) through the swing phase of the gait cycle (5.6 ± 5.1 and 1.4 ± 4.3 for the CAI and coper groups, respectively; p = 0.039). Moreover, they found that individuals with CAI have higher inversion during 71–10% of the gait cycle. For the hip, they found that CAI resulted in higher adduction during the swing phase and had higher adduction during 61 to 84% of the gait cycle. In another study by Gribble and colleagues [14], authors aimed to evaluate the biomechanics of the knee and hip joints after performing a jumping task for evaluation of dynamic stability among patients with CAI. The authors found that the control group had higher flexion in the knee joint during landing on the ground compared to the CAI group (p = 0.008). The current study demonstrated, for the first time, the effects of CAI on lower extremity kinematics during a landing task. Similarly [15], another study evaluated and compared 22 patients with CAI with 22 control and 22 ankle sprain copers, using motion capture cameras. They found that kinetics including ankle joint power in the CAI group compared to the control group had 3.5 W/kg more and 7.9 W/kg less eccentric ankle power during the 0 to 8% and 10 to 50% of the stance phase, respectively (p < 0.05). Moreover, the CAI group had 4.1 W/kg less eccentric ankle power during the 56% to the 89% of the stance phase (p < 0.05). Regarding ankle stiffness, the ankle of the CAI group showed less ankle stiffness compared to the control (0.049 ± 0.013 vs. 0.054 ± 0.014 Nm/kg, p < 0.05). Ground reaction force during a jump landing task was also significantly different in the ankle joint with the control group. Specifically, the ankle joint of patients with CAI had 8% of body weight more medial ground floor reaction during 0–10% of the eccentric stance and 2% of body weight more during 88–95% of the eccentric stance. Moreover, the CAI group had 16% of body weight less medial ground floor reaction during 15–8% of eccentric and concentric stances. The study concluded that this outcome could have been caused due to neuromechanical alterations occurring following CAI. In a recent study by Moisan and colleagues [16], authors compared lower limb biomechanics between patients with CAI and controls. They found that the CAI group showed higher inversion in the ankle joint during 14–48% of the stance phase (p = 0.008); however, they did not find any difference between the knee joints, which was similar to that of our study. Furthermore, the authors found significant differences in ankle eversion moments during the stance phase within the knee and ankle joints with a control group.
After comprehensively evaluating the kinematics of the lower extremity, this investigation found that unilateral CAI not only influences the injured ankle but also alters the biomechanics of the remaining major joints of the uninjured side during normal gait. Moreover, the behavioral gait changes promulgated by CAI appear to also negatively affect the kinematics of other major joints in the ipsilateral side as well. Individuals with CAI tend to alter their gait and posture in order to compensate for the injured ankle, and this also takes effect on the otherwise seemingly uninjured lower extremity. These data would indicate that strong consideration should be given to more aggressive rehabilitative and potentially even surgical management of patients with unilateral CAI in order to prevent progressive biomechanical changes within nearby healthy joints of the lower extremity on both the injured and otherwise healthy sides. Our findings indirectly support the potential benefit of prompt surgical intervention—when proper rehabilitative measures fail—for patients with CAI given the fact that unmitigated CAI appears to continuously impair natural host biomechanics of both lower extremities.
A few limitations should be considered. First, we only assessed patients with the preferred walking speed and did not define any speed restrictions. Some studies have shown that kinematic indices may vary in different walking speeds during the gait cycle [10], although this was not required to test our primary hypothesis. Second, it was that we did not differentiate between athletes and non-athletes’ individuals who referred to us with CAI, as some athletes may have been copers, and this may have affected our results.
Conclusion
Unilateral chronic ankle instability appears to have the capacity to substantially alter the biomechanics of the ipsilateral knee as well as the contralateral ankle, knee, and hip joints in affected patients. Left unchecked, the chronic kinematic alteration and gait compensation caused by CAI may predispose to repetitive overuse and other acute injuries of the musculoskeletal system, with the capacity to affect longevity of other major lower extremity joints as well as day-to-day function in routine as well as sporting activities.
Availability of data and material
Data will be accessible for authors and institutional by directly contacting the corresponding author upon reasonable request.
Code availability
N/A.
References
Herzog MM, Kerr ZY, Marshall SW, Wikstrom EA (2019) Epidemiology of ankle sprains and chronic ankle instability. J Athl Train 54(6):603–610
Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA (2017) The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med 45(1):201–209
McKay GD, Goldie P, Payne WR, Oakes B (2001) Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med 35(2):103–108
Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT-P, Hertel J, Hiller CE, Kaminski TW, McKeon PO (2016) Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med 50(24):1496–1505
Attenborough AS, Hiller CE, Smith RM, Stuelcken M, Greene A, Sinclair PJ (2014) Chronic ankle instability in sporting populations. Sports Med 44(11):1545–1556
Hintermann B, Boss A, Schäfer D (2002) Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 30(3):402–409
Witchalls J, Blanch P, Waddington G, Adams R (2012) Intrinsic functional deficits associated with increased risk of ankle injuries: a systematic review with meta-analysis. Br J Sports Med 46(7):515–523. https://doi.org/10.1136/bjsports-2011-090137
Hubbard TJ, Kramer LC, Denegar CR, Hertel J (2007) Contributing factors to chronic ankle instability. Foot Ankle Int 28(3):343–354. https://doi.org/10.3113/fai.2007.0343
de Noronha M, Refshauge KM, Herbert RD, Kilbreath SL, Hertel J (2006) Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain? Br J Sports Med 40 (10):824–828; discussion 828. https://doi.org/10.1136/bjsm.2006.029645
Koldenhoven RM, Hart J, Saliba S, Abel MF, Hertel J (2019) Gait kinematics & kinetics at three walking speeds in individuals with chronic ankle instability and ankle sprain copers. Gait Posture 74:169–175
Gribble PA, Delahunt E, Bleakley CM, Caulfield B, Docherty CL, Fong DT-P, Fourchet F, Hertel J, Hiller CE, Kaminski TW, McKeon PO, Refshauge KM, van der Wees P, Vicenzino W, Wikstrom EA (2014) Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train 49(1):121–127. https://doi.org/10.4085/1062-6050-49.1.14
Meine MH, Zanotelli ML, Neumann J, Kiss G, de Jesus GT, Leipnitz I, Schlindwein ES, Fleck A Jr, Gleisner AL, de Mello BA, Marroni CA, Cantisani GP (2006) Randomized clinical assay for hepatic grafts preservation with University of Wisconsin or histidine-tryptophan-ketoglutarate solutions in liver transplantation. Transplant Proc 38(6):1872–1875. https://doi.org/10.1016/j.transproceed.2006.06.071
Chinn L, Dicharry J, Hertel J (2013) Ankle kinematics of individuals with chronic ankle instability while walking and jogging on a treadmill in shoes. Phys Ther Sport 14(4):232–239
Gribble PA, Robinson RH (2009) Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train 44(4):350–355
Kim H, Son SJ, Seeley MK, Hopkins JT (2019) Altered movement biomechanics in chronic ankle instability, coper, and control groups: energy absorption and distribution implications. J Athl Train 54(6):708–717
Moisan G, Mainville C, Descarreaux M, Cantin V (2021) Lower limb biomechanics in individuals with chronic ankle instability during gait: a case-control study. J Foot Ankle Res 14(1):36. https://doi.org/10.1186/s13047-021-00476-6
Acknowledgements
The authors would like to thank all the patients and their families for kindly taking part in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Iran University of Science and Technology.
Consent to participate
All participants gave the written and informed consent to enter the study.
Consent for publication
All participants gave their consent for their data to be published.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ziabari, E.Z., Razi, M., Haghpanahi, M. et al. Does ipsilateral chronic ankle instability alter kinematics of the other joints of the lower extremities: a biomechanical study. International Orthopaedics (SICOT) 46, 241–248 (2022). https://doi.org/10.1007/s00264-021-05139-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05139-6