Abstract
Purpose
The unique medial-pivot (MP) design of ADVANCE® system largely simulates the movement of a normal knee joint and a high mid- and long-term success rate has been reported in limited populations. The aims of this study are to investigate the mid-term clinical outcomes and survivorship based on a large cohort with 1128 cases.
Methods
One thousand seven patients received 1276 ADVANCE® MP TKAs from January 2011 to April 2016 in our institution were retrospectively investigated. The range of motion (ROM), the Knee Society Score (KSS), the Knee Society Function Score (KSFS), the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score, and the Forgotten Joint Score (FJS) were used to evaluate clinical outcomes and Kaplan-Meier survival curve was used to calculate the survivorship.
Results
In an averaged five year follow-up, the results of 879 patients (1128 knees) were successfully obtained and the clinical outcomes of 1107 knees were recorded. One hundred forty-eight knees (11.6%) were lost to follow-up. Excellent mid-term ROM, KSS, KSFS, and WOMAC score were recorded. A total of 53 complications were identified and most complications were related to the discordance of femoropatellar joint. Taking revision for any reason as end point, the overall survivorship was 99.2% at seven years. When taking all cases lost to follow-up as failures, the survivorship was 83.8% at five years and 50.6% at seven years.
Conclusion
For MP designs, the intermediate clinical outcomes are good to excellent and the mid-term survivorship related to reasons other than infection is also satisfactory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is the most effective surgical procedure for advanced knee osteoarthritis, aiming to relieve pain, correct malformations and reproduce normal functions of knee joint [1]. The clinical and radiological outcomes, as well as the survivorship, of TKA have been improved by novel prosthetic designs and refined surgical techniques. Satisfactory mid- and long-term outcomes have been confirmed in multiple studies and the survival rate exceeds 90% at 15-years’ follow-up [2,3,4]. However, most existing posterior-stabilized (PS) designs fail to simulate the normal kinematics of knee joint through their post-cam structure, leading to impingement of the central post, patellar clunk syndrome, and “paradoxical anterior slide” of femur during knee flexion, which decreases the patients’ satisfaction [5].
A medial pivotal (MP) design has been used in ADVANCE® prosthesis (MicroPort Orthopedics Inc., China) since 1998. The asymmetrical design of tibial insert constrains the movement of the medial compartment, while allowing the lateral compartment move relatively unrestrictedly, which largely reproduces the normal “medial-pivotal” movement of the knee [6]. With decreased anterior-posterior translation of femoral component, a more conformed intercondylar sagittal contact is expected to distribute the stress and lessen the polyethylene wear [7]. A study using explicit dynamic finite element method has also demonstrated the advantages of MP designs in mimicking the kinematics of a healthy knee, as well as a lowered contact pressure and an enlarged contact area [8]. Another analysis compared the polyethylene wear particles in synovial fluid between MP designs and PS designs, confirming a decrease in both total particle number and particle size generated by MP systems [9]. Despite the theoretical merits, excellent mid- and long-term clinical outcomes, as well as survivorships of the MP system, also have been confirmed in a few studies [10,11,12]. Controversially, there are also some studies stating that the functional outcomes, particularly the range of motion (ROM), of the MP system are worse than those of the press fit condylar (PFC) mobile-bearing prosthesis [13, 14]. Meanwhile, the postoperative complications after MP TKAs have not been fully investigated due to the limited sample size included in the previous studies. Taken together, a follow-up conducted in a large cohort is still needed to further investigate the clinical outcomes, as well as the implant survivorship of MP systems.
In this study, we provided excellent mid-term clinical outcomes in a large cohort, which contains 1128 MP knees performed on Chinese patients diagnosed with end-staged osteoarthritis or rheumatoid arthritis. We also categorized the postoperative complications and reported a satisfactory mid-term survivorship after MP TKAs.
Materials and methods
The review board of our institution approved this study. From January 2011 to September 2016, 1276 ADVANCE® designs (MicroPort Orthopedics Inc., China) were used in primary TKA procedures on 1007 patients diagnosed with end-staged osteoarthritis or rheumatoid arthritis. Demographic characteristics are listed in Table S1.
All procedures were done by six senior surgeons (YZW, HNZ, KS, JZL, CYL, and CYW) in our institution using standard technique. Briefly, knee exposure was achieved through medial parapatellar approach. Intramedullary resection was used for distal femur whereas extramedullary resection for proximal tibia. Intravenous antibiotics were used pre-operatively and 24 hours post-operatively. Post-operatively, low-molecular-weight heparin was used for post-operative prevention of deep venous thromboembolism for two weeks.
Pre-operatively, the range of motion (ROM), the Knee Society Score (KSS), the Knee Society Function Score (KSFS), and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score were recorded to evaluate the function of the knee. Post-operatively, routine follow-ups were conducted at three, 12 months and the final follow-up, which was conducted at December, 2019. Patients were informed to come to the outpatient department and five senior residents (SX, XPX, PCG, ZAZ, and TL) independently conducted all physical examinations and evaluated the clinical outcomes using the ROM, the KSS, the KSFS, and the WOMAC score. Self-reported outcomes were also evaluated using the Forgotten Joint Score (FJS). One hundred twenty-eight patients (12.7%) and 148 knees (11.6%) were lost to follow-up. The final results of 879 patients (1128 knees) were acquired in this averaged five year follow-up. Seventeen deaths were recorded including one death due to cardiovascular complications relevant to TKA procedure. The functional outcomes were successfully recorded in 862 patients (1107 knees), including 726 females and 136 males. In this population, there were 828 patients (1070 knees) diagnosed with osteoarthritis and 32 rheumatoid arthritis. The average age was 67.24 ± 7.13 years and BMI were 27.71 ± 3.64. Table 1 displays the demographic data of patients who finished the last follow-up.
Statistical analysis
The statistical analysis was done by SPSS 15.0 (SPSS Inc, Chicago, IL). Clinical data were presented as mean ± standard deviation (SD). Student t tests were used to compare the difference in continuous variables, for instance, ROM, KSS, WOMAC score, and FJS. Fisher exact test or chi-square test were used to determine the difference in categorical variables. The Kaplan-Meier survivorship analysis was used to calculate the survival rate and revision of any component for any reason was considered the endpoint. The survival time of unrevised TKAs was recorded as the date of last follow-up or date of death. P < 0.05 was considered statistically significant.
Results
The post-operative functional outcomes were significantly improved (Table 2). The ROM was significantly improved from 97.26 ± 17.73 pre-operatively to 108.53 ± 12.05 post-operatively (P < 0.0001), while the KSS increased from 24.49 ± 7.12 pre-operatively to 84.71 ± 10.00 at the last follow-up (P < 0.0001). The pre-operative KSS functional score in this population was 29.74 ± 15.62, which increased to 74.56 ± 14.76 post-operatively (P < 0.0001). The WOMAC score was decreased by more than 52 points, from 72.79 ± 9.80 pre-operatively to 20.09 ± 13.07 post-operatively (P < 0.0001), indicating a remarkable relieve of pain. Moreover, at the last follow-up, the FJS in this population was 67.29 ± 21.05.
A total of 53 complications were recorded (4.8%, Table 3). There are six systemic complications related to TKA containing one death due to cardiac arrest on post-operative day (POD) 1, one case of cardiac infarction on POD2, one case of pulmonary embolism (PE) on POD2, one case of gastrointestinal perforation on POD 4, one case of deep venous thrombosis (DVT), and one case of respiratory failure (RF) on POD4. Ten cases were diagnosed with deep infection, including seven early deep infection and three delayed deep infections. Complications of patellofemoral joint contained 23 cases of continuous joint clicking and seven cases of persistent anterior patellar pain. Other complications included one case of delayed healing of skin incision, two cases of joint instability, two cases of rupture of drainage tube, one dislocation of the insert, and one aseptic loosening due to collision.
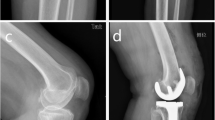
Twelve re-operations of all cause were recorded (1.1%). Two re-operations were performed to retrieve the broken ends of the drainage tube. Ten revision procedures were performed. One-stage revisions were used in five cases with early deep infection and one case of insert dislocation. For the three cases of delayed deep infection, two-stage exchanges were performed. Notably, a reconstruction of medial collateral ligament was performed to treat a severe instable knee 1 year after TKA; however, a revision procedure was still needed due to valgus laxity (Fig. 1).
The peri-operative images of the only patient who received a revision TKA due to reasons other than infection. a Pre-operative anterior-posterior (AP) knee image showing a severe valgus deformity of the knee. b AP knee image taken on post-operative day (POD) 2. c AP knee image taken at 1 year after the primary TKA and before the reconstruction of medial collateral ligament. d AP knee image taken on POD2 of the reconstruction of medial collateral ligament. e AP knee image taken at 2 months after the reconstruction of medial collateral ligament. f AP knee image taken at 1 year after the reconstruction of medial collateral ligament. g AP knee image taken at 3 years after the reconstruction of medial collateral ligament and 4 years after the primary TKA, before the revision procedure. h AP knee image taken on POD4 of the revision procedure
A mid-term cumulative survival rate of 99.2% (95% CI, 99.6–98.4%, Fig. 2a) was demonstrated by survivorship analysis when considering the revision for any reason as an end point, and 99.9% with revision for aseptic reasons as an end point (Fig. 2b). However, when taking all cases lost to follow-up as failures, the survivorship was 83.8% at five years and 50.6% at seven years. (Fig. 2c)
Discussion
The ADVANCE® MP system has been used for more than 20 years in TKA procedures. The unique medial-pivotal design largely simulates the kinematics of a healthy knee, which attracts intensive attention. Recently, satisfactory mid- and long-term outcomes, as well as survivorship, have been reported in several studies, indicating a high success rate in MP TKA [15]. However, the small sample size in previous studies compromised the reliability of their conclusions and some issues related to MP system were not fully investigated. Thus, in this study, we aimed to demonstrate the intermediate clinical outcomes and survivorship of the MP TKA based on a large Chinese cohort including 1128 knees.
Although excellent clinical outcomes have been demonstrated, controversial conclusions still exist when compared MP system with other PS prosthesis. Kim et al. demonstrated worse early and long-term outcomes of MP prosthesis, especially less ROM [13, 14]. In this study, significant improvements of post-operative clinical parameters including KSS clinical component, KSS function component, WOMAC score, and ROM were provided in this averaged five year follow-up, which is similar to previous studies reporting the mid-term outcomes of MP system [12, 16,17,18,19,20]. In a meta-analysis conducted by Fitch et al., which included eight intermediate follow-ups of MP system and contains 1146 MP knees, the weighted mean KSS and KSS function score were reported to be 87.9 (73.2–92.1) and 80.0 (65.0–85.4) [15], while the three year, four year, and five year pooled survivorships were 99.5%, 99.4%, and 99.2%, respectively. In our study, the averaged KSS and KSS function score were 84.71 and 74.56, respectively, which were relatively lower than the weighted scores reported by Fitch et al. In our study, the preoperative KSS, KSS function component, and the ROM are lower than those reported in other independent researches, indicating a worse pre-operative clinical function of the knee. Considering that the post-operative function is largely depended on the pre-operative function, we attribute the lowered KSS and KSS function component to the worse pre-operative conditions. The survival rate with a mean five year follow-up was 99.2%, which is very similar to the pooled survivorships in the meta-analysis. In our study, with the large cohort in this study, the bias is largely eliminated and the survivorship is reasonable. The survival rate was even higher when considering revision due to aseptic reasons, reaching 99.9%, which demonstrated the reliable effect of MP system. The FJS is composed of 12 questions of daily activities to assess the joint awareness after joint replacement. Although the FJS has been used to evaluate the patient-reported joint awareness in several previous studies, it is rarely reported in MP TKAs. Compared with the PS knees, the design of MP systems largely mimics the normal kinematics of a healthy knee and is presumed to have better results of joint awareness. Samy et al. reported a 1-year FJS of 60.56 ± 31.38 of MP systems and compared it with that of PS designs. They found a significantly better FJS in favor of the MP systems [21]. Here, we reported an averaged 5-year FJS of 67.29 ± 21.05, which is better than the one year FJS reported by Samy et al. The FJS is mainly affected by pain within one month after joint arthroplasty, and by strength of quadriceps after six months [22]. As a result, with the gradual recovery of the quadriceps strength, the results of joint awareness should be better in daily activities if no complication occurred.
In our cohort, we identified 30 patellofemoral complications, including seven cases of anterior patella pain and 23 cases of joint clicking, which took the greatest amount among all complications. Although no re-operation is needed at present, the patellofemoral complications reduce the satisfactory rate of the patients. Theoretically, the MP system largely mimics the normal kinematics of a healthy knee; however, an excessive internal rotation of the femur has been observed during climbing and descending stairs, as well as during the stance phase of the gait cycle. This phenomenon has been regarded to increase the tension of the patella [8]. Clinically, MP system alters the kinematics of the patellofemoral joint, as well as the patella tilt and patella shift [23, 24]. However, the complications of patellofemoral joint after MP TKA are seldom studied. Based on our data, we presumed that the post-operative patellofemoral complications might be caused by the increased tension due to the changed kinematics of the patellofemoral joint. Thus, more attentions should be paid when adjusting the patellar tracking during the procedure, or patella resurfacing technique may be a solution to this problem. Unfortunately, until now, no study has investigated the clinical outcomes of patellar resurfacing in MP systems.
In our study, the reasons of implant failure and revision TKAs were recorded. Among ten revision procedures, nine revision TKAs were used to treat joint infection, and the other one was carried out due to severe valgus laxity. To maintain the unique “medial pivot” kinematics of the MP system, the stability of medial compartment, especially the normal function medial collateral ligament, is emphasized. However, in most cases with severe valgus, laxity of medial structures and contracted lateral compartment are two prominent characteristics. Moreover, rheumatoid arthritis is one of the main reasons that cause valgus deformity. The persistent erosion of the ligaments also provides the potential late-onset medial instability after joint replacement. Considering the concept of the MP implants, it is still controversial whether MP implants are suitable for severe valgus deformities. Although Kitagawa et al. demonstrated a partial restoration of normal “medial-pivotal” kinematics in seven patients with severe valgus deformity using MP implants, no independent study investigated the clinical outcomes of MP implants in treating severe valgus knees [25]. In our study, the case was diagnosed with rheumatoid arthritis and severe valgus deformity. The patient received a reconstruction of medial collateral ligament one year after MP TKA and a revision procedure using hinge knee implant four years after the primary TKA due to knee instability. Although lacking generalization, this single case might partly reflect the limitations of MP systems in treating severe valgus deformity. However, intensive clinical trials are still needed to demonstrate the applicability of MP implants in severe valgus knees.
Several limitations of this study should be acknowledged. One of the limitations is due to the retrospective design, which lowered the evidence level of the current study. In addition, the follow-up period in this study was relatively short and should be maintained for the long-term. Recently, several studies have reported excellent long-term outcomes and survivorship of the MP system, but the cohort should be enlarged to decrease the bias [26, 27]. Moreover, although the five senior residents followed the same criteria when recording the final outcomes, bias could inevitably exist across the residents. Another limitation is that the radiological outcomes were not included in this study, resulting in the absence of an evaluation of the positioning of the prosthesis. The final limitation is that the high loss to follow-up rate. In this study, the loss to follow-up rate reached nearly 15%. We attribute this to the incomplete follow-up system, as well as rapid human transportation and change of contact information. However, in the literature, a lower rate of failure and higher satisfaction rate has been demonstrated in the population “lost to follow-up” [28]. Nevertheless, we depicted a Kaplan-Meier survivorship curve regarding all cases lost to follow-up as failures (Fig. 2c). When taking all cases lost to follow-up as failures, the survivorship was 83.8% at five years and 50.6% at seven years. We will continue trying to contact with those lost to follow-up and enlarging our database.
Taken together, we presented the mid-term follow-up of the MP system based on a large sample cohort, and provided satisfactory intermediate clinical outcomes and survivorship. We also investigated the post-operative complications and proposed the possible reasons that lead to the complications based on the experience of our institution. However, more studies are still needed to reveal the advantages and disadvantages of the MP implants.
References
Dixon MC, Brown RR, Parsch D, Scott RD (2005) Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am 87(3):598–603. https://doi.org/10.2106/JBJS.C.00591
Papasoulis E, Karachalios T (2019) A 13- to 16-year clinical and radiological outcome study of the genesis II cruciate retaining total knee arthroplasty with an oxidised zirconium femoral component. Knee 26(2):492–499. https://doi.org/10.1016/j.knee.2019.01.013
Kremers HM, Sierra RJ, Schleck CD, Berry DJ, Cabanela ME, Hanssen AD, Pagnano MW, Trousdale RT, Lewallen DG (2014) Comparative survivorship of different tibial designs in primary total knee arthroplasty. J Bone Joint Surg Am 96(14):e121. https://doi.org/10.2106/JBJS.M.00820
Feng B, Weng X, Lin J, Jin J, Wang W, Qiu G (2013) Long-term follow-up of cemented fixed-bearing total knee arthroplasty in a Chinese population: a survival analysis of more than 10 years. J Arthroplast 28(10):1701–1706. https://doi.org/10.1016/j.arth.2013.03.009
Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ (2003) Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res 410:139–147. https://doi.org/10.1097/01.blo.0000063565.90853.a4
Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T (2011) Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplast 26(7):1038–1044. https://doi.org/10.1016/j.arth.2010.08.015
Ansari F, Ries MD, Pruitt L (2016) Effect of processing, sterilization and crosslinking on UHMWPE fatigue fracture and fatigue wear mechanisms in joint arthroplasty. J Mech Behav Biomed Mater 53:329–340. https://doi.org/10.1016/j.jmbbm.2015.08.026
Shu L, Yamamoto K, Kai S, Inagaki J, Sugita N (2019) Symmetrical cruciate-retaining versus medial pivot prostheses: the effect of intercondylar sagittal conformity on knee kinematics and contact mechanics. Comput Biol Med 108:101–110. https://doi.org/10.1016/j.compbiomed.2019.03.005
Minoda Y, Kobayashi A, Iwaki H, Miyaguchi M, Kadoya Y, Ohashi H, Yamano Y, Takaoka K (2003) Polyethylene wear particles in synovial fluid after total knee arthroplasty. Clin Orthop Relat Res 410:165–172. https://doi.org/10.1097/01.blo.0000063122.39522.c2
Karachalios T, Varitimidis S, Bargiotas K, Hantes M, Roidis N, Malizos KN (2016) An 11- to 15-year clinical outcome study of the Advance Medial Pivot total knee arthroplasty: pivot knee arthroplasty. Bone Joint J 98-B(8):1050–1055. https://doi.org/10.1302/0301-620X.98B8.36208
Castellarin G, Pianigiani S, Innocenti B (2019) Asymmetric polyethylene inserts promote favorable kinematics and better clinical outcome compared to symmetric inserts in a mobile bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27(4):1096–1105. https://doi.org/10.1007/s00167-018-5207-9
Fan CY, Hsieh JT, Hsieh MS, Shih YC, Lee CH (2010) Primitive results after medial-pivot knee arthroplasties: a minimum 5-year follow-up study. J Arthroplast 25(3):492–496. https://doi.org/10.1016/j.arth.2009.05.008
Kim YH, Yoon SH, Kim JS (2009) Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res 467(2):493–503. https://doi.org/10.1007/s11999-008-0221-8
Kim YH, Park JW, Kim JS (2017) Clinical outcome of medial pivot compared with press-fit condylar sigma cruciate-retaining mobile-bearing total knee arthroplasty. J Arthroplast 32(10):3016–3023. https://doi.org/10.1016/j.arth.2017.05.022
Fitch DA, Sedacki K, Yang Y (2014) Mid- to long-term outcomes of a medial-pivot system for primary total knee replacement: a systematic review and meta-analysis. Bone Joint Res 3(10):297–304. https://doi.org/10.1302/2046-3758.310.2000290
Chinzei N, Ishida K, Tsumura N, Matsumoto T, Kitagawa A, Iguchi T, Nishida K, Akisue T, Kuroda R, Kurosaka M (2014) Satisfactory results at 8 years mean follow-up after ADVANCE(R) medial-pivot total knee arthroplasty. Knee 21(2):387–390. https://doi.org/10.1016/j.knee.2013.10.005
Karachalios T, Roidis N, Giotikas D, Bargiotas K, Varitimidis S, Malizos KN (2009) A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. Knee 16(6):484–488. https://doi.org/10.1016/j.knee.2009.03.002
Youm YS, Cho SD, Lee SH, Cho HY (2014) Total knee arthroplasty using a posterior cruciate ligament sacrificing medial pivot knee: minimum 5-year follow-up results. Knee Surg Relat Res 26(3):135–140. https://doi.org/10.5792/ksrr.2014.26.3.135
Ishida K, Matsumoto T, Tsumura N, Iwakura T, Kubo S, Iguchi T, Akisue T, Nishida K, Kurosaka M, Kuroda R (2014) No difference between double-high insert and medial-pivot insert in TKA. Knee Surg Sports Traumatol Arthrosc 22(3):576–580. https://doi.org/10.1007/s00167-012-2314-x
Vecchini E, Christodoulidis A, Magnan B, Ricci M, Regis D, Bartolozzi P (2012) Clinical and radiologic outcomes of total knee arthroplasty using the Advance Medial Pivot prosthesis. A mean 7 years follow-up. Knee 19(6):851–855. https://doi.org/10.1016/j.knee.2012.04.002
Samy DA, Wolfstadt JI, Vaidee I, Backstein DJ (2018) A retrospective comparison of a medial pivot and posterior-stabilized total knee arthroplasty with respect to patient-reported and radiographic outcomes. J Arthroplast 33(5):1379–1383. https://doi.org/10.1016/j.arth.2017.11.049
Hiyama Y, Wada O, Nakakita S, Mizuno K (2016) Joint awareness after total knee arthroplasty is affected by pain and quadriceps strength. Orthop Traumatol Surg Res 102(4):435–439. https://doi.org/10.1016/j.otsr.2016.02.007
Chinzei N, Ishida K, Matsumoto T, Kuroda Y, Kitagawa A, Kuroda R, Akisue T, Nishida K, Kurosaka M, Tsumura N (2014) Evaluation of patellofemoral joint in ADVANCE Medial-pivot total knee arthroplasty. Int Orthop 38(3):509–515. https://doi.org/10.1007/s00264-013-2043-x
Ishida K, Matsumoto T, Tsumura N, Chinzei N, Kitagawa A, Kubo S, Chin T, Iguchi T, Akisue T, Nishida K, Kurosaka M, Kuroda R (2012) In vivo comparisons of patellofemoral kinematics before and after ADVANCE medial-pivot total knee arthroplasty. Int Orthop 36(10):2073–2077. https://doi.org/10.1007/s00264-012-1634-2
Kitagawa A, Ishida K, Chin T, Tsumura N, Iguchi T (2014) Partial restoration of knee kinematics in severe valgus deformity using the medial-pivot total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(7):1599–1606. https://doi.org/10.1007/s00167-012-2315-9
Bordini B, Ancarani C, Fitch DA (2016) Long-term survivorship of a medial-pivot total knee system compared with other cemented designs in an arthroplasty registry. J Orthop Surg Res 11:44. https://doi.org/10.1186/s13018-016-0388-8
Macheras GA, Galanakos SP, Lepetsos P, Anastasopoulos PP, Papadakis SA (2017) A long term clinical outcome of the Medial Pivot Knee Arthroplasty System. Knee 24(2):447–453. https://doi.org/10.1016/j.knee.2017.01.008
Joshi AB, Gill GS, Smith PL (2003) Outcome in patients lost to follow-up. J Arthroplast 18(2):149–153. https://doi.org/10.1054/arth.2003.50061
Funding
This research is supported by the National Natural Science Foundation of China (No. 81672197) and the Youth Program of the National Natural Science Foundation of China (No. 82002349).
Author information
Authors and Affiliations
Contributions
SX performed all the analysis and write the paper. YZW, CYL, and CYW collected the data and participated in writing and revising the paper. HNZ designed the whole study.
Corresponding author
Ethics declarations
Ethics approval
The review board of the Affiliated Hospital of Qingdao University approved this study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The participant has consented to the submission of the case report to the journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Xiang, S., Wang, Y., Lv, C. et al. Mid-term clinical outcomes and survivorship of medial-pivot total knee arthroplasty—a mean five year follow-up based on one thousand, one hundred and twenty eight cases. International Orthopaedics (SICOT) 45, 2877–2883 (2021). https://doi.org/10.1007/s00264-021-05017-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05017-1