Abstract
Purpose
The purpose of this study was to investigate whether adductor canal block (ACB) combined with lateral femoral cutaneous nerve block (LFCNB) could improve the efficacy of post-operative analgesia in a comparison with a standard peri-articular infiltration analgesia (PIA) after a total knee arthroplasty (TKA).
Methods
One hundred and sixty patients of scheduled unilateral primary TKA were randomly allocated into two groups for post-operative analgesia. Eighty cases were treated with ACB combined with LFCNB and the other eighty treated with PIA. The primary outcomes were pain visual analogue scale (VAS) and rescue pain killer consumption, and the secondary outcomes were knee active range of motion (ROM), quadriceps strength, patients’ ambulation ability, Knee Society Score (KSS), length of hospital stay, and adverse events.
Results
We found that ACB combined with LFCNB was better on decreasing the post-operative pain score within 12 hours at rest and 8 h with activity (p < 0.05) and provided longer duration of analgesia (19.91 ± 5.09 VS 12.06 ± 3.67 h, p < 0.01) and less rescue morphine consumption (13.63 ± 9.84 vs 18.00 ± 11.52 mg, p = 0.011) than the PIA. There was no significant difference between the two groups (p > 0.05) in terms of knee ROM, quadriceps strength, daily mobilization distance, KSS, and complication occurrence.
Conclusions
ACB combined with LFCNB provides a significantly better pain control, less opioid consumption, and longer duration of analgesia than peri-articular infiltration while preserving muscle function without affecting knee functional recovery nor the length of stay or side effects occurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has become the most effective method to treat advanced knee osteoarthritis [2]. Despite the tremendous progress that the surgical procedure has achieved, TKA still cannot meet the patients’ standard of satisfaction. In the literature, it shows that nearly 20% of patients are not satisfied with their clinical outcomes after TKA and mainly because of poor post-operative pain control [1, 10]. Post-operative pain is an undesirable experience that influences patients’ early rehabilitation. There are almost approximately 60% of patients who underwent TKA suffered such moderate to severe post-operative pain, but the optimal pain management protocol has not been well defined [1, 12, 24].
As the development of enhanced recovery after surgery (ERAS), the patients increasingly expect to have an early rehabilitation without much suffering of pain [13, 26]. In recent years, many methods have been reported to be effective as post-operative analgesics, including opioids consumption, epidural analgesia, peripheral nerve block, and multimodal peri-articular infiltration analgesia [13, 19, 30]. Periarticular infiltration analgesia (PIA) is the most common used method in TKA for relieving the post-operative pain. Studies have showed that the method of PIA combined with multimodal analgesia could improve pain management and provide good performance on early rehabilitation after TKA [14, 16, 19].. Nerve block as a mode of regional analgesia has shown a good pain control efficacy in knee arthroplasty [6, 8, 13, 14, 19]. However, with either peripheral nerve block or neuraxial block, the preservation of quadriceps function and preventing patient from fall must be the main concerns [5, 8, 18, 19]. Adductor canal block (ACB) is a popular and successful method for reducing pain after TKA by blocking the saphenous nerve without weakening the quadriceps strength, and it is usually recommended for pain management after TKA [5, 18, 31]. Studies have shown that ACB alone is not as good as peri-articular infiltration of analgesia (PIA) in the setting of total knee arthroplasty [9, 19, 21]. Therefore, the use of ACB alone may not be enough.
In fact, the anatomical distributions of saphenous nerve only cover the medial and anterior regions of the knee [21, 29]. Consequently, ACB can only relieve the pain in the anteromedial sides of the knee and not the lateral or posterior regions. According to previous studies [17, 25], the local analgesia within the posterior capsule has no additional analgesic effects after TKA but may increase the damage to the nerve and vessels in the capsule. Therefore, blocking the nerve in the posterior capsule of the knee is not beneficial. In addition, it is still unknown, and no study reported if blocking the sensory nerve that distributes in the anterolateral side of knee could benefit to the post-operative analgesia. Anatomical studies showed that lateral femoral cutaneous nerve (LFCN) distributes in the anterolateral side of the knee, which may make blocking it combined with ACB a good method for pain management after TKA [4, 22].
In this RCT, we want to evaluate if additional blocking of the lateral femoral cutaneous nerve (LFCNB) combined with ACB could further relieve the pain, reduce the opioids consumption, and accelerate early rehabilitation when compared with a standard PIA after TKA.
Material and methods
This study was a single-center, prospective, double-blind, randomized controlled trial (RCT). The approval was obtained from the Clinical Trials and Biomedical Ethics Committee of our institution (NO.2012268) and was registered with the Chinese Clinical Trial Registry (ChiCTR1800015832). All participants had signed the informed consent before the surgery.
Patients and inclusion criteria
We included patients who underwent primary unilateral TKA at our hospital from April 2018 to January 2019. Patients from 50 to 80 years of age with a body mass index (BMI) of 19 to 30 kg/m2 and an American Society of Anesthesiologists (ASA) functional status of I–III were included. We excluded patients (1) with knee deformity, flexion deformity ≥ 30°, varus-valgus deformity ≥ 30°; (2) have allergy to the study anaesthesia drugs or had a long past history of opioid consumption; (3) had any contraindications to nerve blocks or local infiltration; and (4) with a medical history of psychiatric illness, cognitive impairment, recognized neuromuscular disorder, narcotic dependency, knee infection, knee surgery, or thrombolytic events including myocardial infarction, cerebrovascular accident, deep vein thrombosis, and pulmonary embolus. In addition, the patients with a language barrier, or refused to sign the informed consent, were not included as well.
Randomization
Eligible patients were randomized using a computer-generated list of random numbers with a 1:1 allocation ratio into two groups (ACB + LFCNB VS PIA) prior to the TKA procedures. Investigator (XX) sealed the random numbers in opaque envelopes, and the patients were required to select an envelope to determine the treatment group. The surgeons, outcome assessors (YY), anesthetists, data collectors and statistical analysts were all blinded to the analgesic techniques and groups allocation.
Pre-operative management
Basic characteristics of the patients, including age, sex, BMI, ASA degree, pain score, ROM, quadriceps strength, and KSS (Knee Society Score) were documented on hospital admissions. Loxoprofen (60 mg, twice a day) was prescribed to control the pain after hospital admission.
All TKAs were performed by a group of surgeons using a standard medial parapatellar approach after general anesthesia, and the prostheses that were used included Depuy P.F.C and striker triathlon. Pneumatic tourniquets were applied during the surgeries, as well as the use of tranexamic acid (1 g, i.v, b.i.d), measures to control blood pressure, and elastic bandages.
Adductor canal block with lateral femoral cutaneous nerve block group (experiment group)
Single-shot injections of 30 ml anaesthetics consisted of 0.2% ropivacaine and 2.0 μg/ml epinephrine were administrated pre-operatively under ultrasound guidance by experienced anesthesiologists into the adductor canal and lateral femoral cutaneous nerve region. The anesthetics were prepared by investigator (XX) who did not take part in the surgery, anaesthesia, outcomes collection, and statistical analysis.
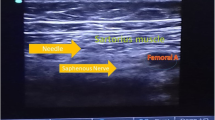
Adductor canal block: Adductor canal was identified at the middle of the thigh using a high-frequency linear array ultrasonic transducer. A 22-gauge, 100-mm needle was directed into the fascia of the sartorius and 3 mL of isotonic saline was injected to ensure the correct placement of the needle, and then, a 20 mL of anaesthetic was injected into the canal.
Lateral femoral cutaneous nerve block: As introduced above, the same ultrasonic transducer helped identifying the lateral femoral cutaneous nerve between the origin of the sartorius and the tensor fasciae latae muscle, and another 10 mL of anaesthetic was injected subcutaneously to cover the lateral side of the knee joint [22, 27].
Sham peri-articular injections of isotonic saline solution (100 mL) were administered intra-operatively, and both the surgeon and anaesthetist were blinded.
Peri-articular infiltration analgesia (control group)
To ensure blinding, patients allocated to the control group underwent a pre-operative injection of isotonic saline solution (60 mL) in the adductor canal and lateral femoral cutaneous nerve region. The same amount of the anaesthetic solution (0.2% ropivacaine, 2.0 μg/mL of epinephrine, total 100 ml) was prepared during the operation. The infiltration analgesia in the posterior region of the capsule was performed using 20 ml of the solution prior to placement of the prosthesis. Another 20 mL of the solution was injected in the medial and lateral collateral ligaments prior to the component implantation. After implantation of the prosthesis, the quadricep and retinacular tissues were infiltrated with 20 mL of solution, while the fat and subcutaneous tissues were infiltrated with 40 mL of PIA solution [9, 24]. Regular drainage tubes were not used in all the patients in this study.
Post-operative management
Patients were sent to the ward with an ice compress applied around the incision after being revived from anaesthesia. Loxoprofen (60 mg, 1 tab, twice a day) was administered to control post-operative pain, and alprazolam (0.4 mg, 1 tab, quaque nocte) was prescribed to help sleep at night. Morphine hydrochloride (10 mg) was intramuscularly administrated if patients were unable to tolerate the pain or pain score was higher than six points at rest. For venous thromboembolism (VTE) prevention, enoxaparin (0.2 mL) was subcutaneously administered at 12 hours after surgery, then 0.4 mL every 24 hours afterward until hospital discharge, and after that, rivaroxaban (10 mg) was prescribed once a day orally for two weeks. The elastic bandages were removed two hours after the patients have been sent to the ward and passive and active physiotherapy began, including lower limbs movements and lower extremity’s strength training. X-rays of the knee were reviewed a day post-operatively, and patients were required to walk with partial weight-bearing.
Outcome measurement
The primary outcomes that were assessed included the post-operative pain at rest and with activity (knee flexion of 45°) at two, four, eight, 12, 24, and 48 hours and at discharge using visual analogue scale (VAS) score (in the scale of 0–10, where 0 indicates no pain and 10 indicates worst pain) [19, 20, 27]. The consumption of morphine hydrochloride that was required to control intolerable pain was also documented [19, 20]. The time from the end of surgery to the first remedial morphine usage was regarded as the duration of analgesia [27]. The secondary outcomes that evaluated the knee functional recovery included the ROM, quadriceps strength (in the scale of 0–5, where 0 indicates worst strength, and 5 indicates best strength), patients’ daily ambulation distance, and functional KSS (Knee Society Score, evaluating the ability of walking and climbing) [27]. Other outcomes that were investigated are the occurrence of any adverse events, such as nausea, vomiting, wound secretions, wound swelling, delayed wound healing, venous thrombosis, and any neurovascular, cerebrovascular, and cardiovascular events. The duration of hospital stay was also recorded. All patients were suggested to remove the stitches three weeks after operation and return to the hospital three months later to evaluate the function and rehabilitation.
Statistical analysis
Based on previously published reports and our preliminary pilot study, we found that pain score was 4.3 ± 1.8 at 24 hours after operation with activity and considered a mean difference of 1.0 VAS point between both groups to be clinically significant difference post-operatively. This helps to calculate that at least 72 patients, with an anticipated 20% dropout rate, are needed in each group with a two-sided alpha level of 0.05 and power of 90%. The data of patients’ demographic characteristics including age, weight, height, and body mass index were normally distributed and analyzed using Student’s t test, while gender and surgery side were categorical data and analyzed using the chi-squared test. Clinical outcomes of continuous data, including pain score, morphine consumption, analgesic duration time, ROM, daily mobilization, KSS, and hospital stays, were also analyzed using Student’s t test with Levene examination for the normally distributed data and the Mann-Whitney U test for those not normally distributed data (skewed data). The categorical data, e.g., adverse events occurrence, were analyzed using chi-square and Fisher exact test. All statistical analyses were performed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA). Differences with a p value of < 0.05 indicate statistically significant.
Results
Patient characteristics
A total of 200 patients were assessed for eligibility; as shown in the flowchart (Fig. 1), 20 patients did not meet the inclusion criteria, and another 12 refused to participate in the study. The remaining 168 eligible patients were randomized into two groups, 84 in the LFCNB + ACB group and 84 in the PIA group; however, eight patients (four from each group) were excluded as a result of rejecting the postoperative assessments. Baseline characteristics, including age, gender, BMI, preoperative pain scores, knee ROM, quadriceps strength, KSS function score, ASA status, and operation time, were similar across both groups (Table 1).
Primary outcomes concerning pain control
Patients in LFCNB + ACB group had significantly lower VAS score for pain while resting at two, four, eight and 12 hours post-operatively when compared with the patients in the PIA group (p < 0.05) (Table. 2, Fig. 2). The VAS pain scores with activity at two, four, eight hours post-operatively were also significantly lower for the patients in LFCNB + ACB group compared with those in PIA group (p < 0.05) (Table 2, Fig. 3). In addition, there were 65 patients (81.25%) in LFCNB + ACB group who required morphine injections for severe pain compared with 69 patients (86.25%) in PIA group (p > 0.05). The morphine consumption at the first 24 hours post-operatively in patients treated with ACB combined with LFCNB was less compared with those treated with PIA (10.88 ± 6.79 vs 13.75 ± 7.18 mg; p = 0.010) (Table 2, Fig. 4). In addition, the total post-operative morphine consumption in the LFCNB + ACB group showed a better outcome (13.63 ± 9.84 vs 18.00 ± 11.52 mg, p = 0.011). However, post-operative VAS pain scores at rest and with activity (at 24, 48, and 72 h) and morphine consumption (at days 2 and 3) were not significantly different among the two groups (p > 0.05). Time to first rescue analgesia which used to evaluate the analgesia duration was significantly longer for the patients in group ACB combined with LFCNB (19.91 ± 5.09 h) compared with those in PIA group (12.06 ± 3.67 h)(p < 0.001) (Fig. 5).
Secondary outcomes concerning function recovery
There was no difference between the two groups in terms of the secondary outcome measures, including knee ROM, quadriceps strength, time to first mobilization, and daily mobilization distance post-operatively (p > 0.05). The patients in ACB + LFCNB group stayed in hospital for 74.31 ± 10.96 hours after operation, while those in PIA group stayed for 74.71 ± 11.15 h, and this difference was not statistically significant (p = 0.65). There were no significant differences between the two groups (p > 0.05) (Table 3) in the KSS function scores which were evaluated at hospital discharge and two months follow-up.
Other outcomes
Nausea has occurred in 27 (33.8%) patients in ACB + LFCNB group and 31 (38.8%) patients in PIA group (p = 0.511), and vomiting occurred in 13 (16.3%) vs 17 (21.3%) patients (p = 0.418). The symptoms improved after treated with metoclopramide dihydrochloride injections. Additionally, other adverse events, including wound oozes, wound swelling, delayed wound healing, and venous thrombotic events, were not significantly different between the two groups (p > 0.05). There were no occurrence of pulmonary embolisms, patients fall incidents, or neurovascular, cerebrovascular, and cardiovascular events. Furthermore, the three month mortality and three month readmission in both groups did not occur as well (Table 4).
Discussion
This study was conducted to investigate whether ACB combined with LFCNB could improve the efficacy of post-operative analgesia compared with standard PIA after TKA. We found that ACB combined with LFCNB was better on decreasing the pain score at rest within 12 hours post-operatively and at eight hours with activity, providing longer duration of analgesia and less morphine consumption compared with the PIA. However, the other outcome measures including knee ROM, quadriceps strength, early functional rehabilitation, and complication occurrence were comparable between the two groups.
TKA is a procedure that leads to bone and soft tissue damage and is associated with the exposure of sensory nerve fibers that distributed around the patella without enough soft tissue protection, which make the patients have to suffer severe post-operative pain [20, 32]. Additionally, surgical stress-induced immune reactions and inflammatory reactions increase the sensitivity of the nerve fibers around the knee and result in more pain [20]. Therefore, multimodal analgesia with peripheral nerve blocks or peri-articular local infiltration has become popular and effective methods to relieve the pain [13, 14, 16, 19, 30]. Peri-articular infiltration analgesia is a commonly used procedure on post-operative pain control; however, the nerve selective is poor and requires large quantity of anaesthetic with unsatisfactory duration [19, 27]. Therefore, blocking specified peripheral nerves around the knee to control the pain with taking into consideration the muscle strength was our intention. Femoral nerve block (FNB) and sciatic nerve block (SNB) are not recommended for analgesia in TKA [5, 13, 19]. As reported in the literature, ACB controls only the pain in the anteromedial region of the knee, which might be a disadvantage compared with PIA [19, 27]. To improve the analgesic effects of ACB, blocking the nerve that control the lateral side of the knee might be a good option. LFCNB is a technique that could decrease the sensations in later thigh and knee [4, 22, 23] and has been used in total hip arthroplasty (THA). In fact, previous studies have reported the use of LFCNB in knee surgery [7, 15], but the analgesic effect in TKA was not clear. This study was conducted to investigate whether LFCNB can be a good supplement to ACB and whether ACB combined with LFCNB can provide better pain management when compared with standard PIA.
LFCN originates from L2 and L3 with variation of its upper distribution before going through the inguinal ligament but usually went down between the origin of the sartorius and the tensor fasciae latae muscle [3, 27]. Tang J [28] reported that more than 95% of people had LFCN with the trunk’s body surface from anterior superior spine to middle point of the patella outer margin. The terminal branches are evenly distributed over the components in the upper and lateral side of the knee joint. At the same time, almost 100% of the LFCN diverged an anterior branch that distributed to the patella [22, 28]. Consequently, blocking LFCN could decrease sensation in in anterolateral side of the knee and play as a supplementary method to ACB in post-operative analgesia of TKA. Sogbein OA et al. [27] reported that blocking the nerves around the knee could help to decrease the post-operative pain, but the techniques were complicated. This study investigated the analgesic effects of blocking the medial, anterior, and lateral region of the knee.
According to the results, the pain scores while resting at two, four, eight and 12 hours and with activity at two, four and eight hours post-operatively were significantly lower in patients treated with LFCNB combined with ACB. Furthermore, the mean difference of pain scores at four and eight hours was higher than 1.1. This indicates that specified nerve block provides better pain control than blind PIA in the early time after TKA. The additional method of LFCNB combined with ACB decreased the pain scores especially in the lateral aspect of knee. In addition, the rescue morphine consumption at the first 24 hours was reduced in the group of LFCNB combined with ACB, which indicates that the pain was better controlled in this group. More importantly the patients in PIA group required the first morphine injection at mean 12.06 ± 3.67 hours after operation compared with 19.91 ± 5.09 h in nerve block group, which suggests that LFCNB combined with ACB could decrease the pain and prolong the analgesia duration in TKA. However, the pain scores at other time points have no significant differences between the two groups. These outcomes demonstrated that the pain at early stages after TKA was hard to bear, and effected badly patients’ comfort and effective measures are indicated [20, 25, 27], but the pain scores were not significant after recue pain killers were used. The quadriceps strength, functional recovery outcomes, and the adverse events were comparable between the two groups, which indicated that the nerve block protocol in this study was a motor-sparing technique and had no significant influence on muscle strength and knee functional rehabilitation. Nevertheless, other outcomes were without significant difference; the better pain control and less opioid consumption made the patients experience a better comfort during the early rehabilitation.
One of the limitations of this study was the variation of LFCN; as studies showed, 12% of LFCN gave off the anterior branches in the pelvic cavity [11, 28], so the LFCNB cannot cover all cases, which might be the reason that some of the patients in study group still suffered severe pain. The second limitation was that we combined the use of ACB and LFCNB; however, it is still unknown if the single method of LFCNB could provide good performance in TKA. The third limitation was that despite what has been reported, studies have shown that the pain in the posterior of the knee is mild [17, 25]; we did not investigate that in this study.
In conclusion, a LFCNB combined with ACB provides a significantly better pain control, less opioid consumption, and longer duration of analgesia than peri-articular infiltration while preserving muscle function and without affecting length of stay, satisfaction, side effects, or functional rehabilitation. Additional LFCNB may be a good supplement for ACB on increasing the nerve blocking area for analgesia following TKA and can be recommended for clinical practice.
References
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Demey G, Magnussen RA, Lustig S, Servien E, Neyret P (2012) Total knee arthroplasty for advanced osteoarthritis in the anterior cruciate ligament deficient knee. Int Orthop 36:559–564
de Ridder VA, de Lange S, Popta JV (1999) Anatomical variations of the lateral femoral cutaneous nerve and the consequences for surgery. J Orthop Trauma 13:207–211
Egeler C, Jayakumar A, Ford S (2013) Motor-sparing knee block - description of a new technique. Anaesthesia 68:542–543
Elkassabany NM, Antosh S, Ahmed M, Nelson C, Israelite C, Badiola I, Cai LF, Williams R, Hughes C, Mariano ER, Liu J (2016) The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: a double-blinded randomized controlled study. Anesth Analg 122:1696–1703
Elkassabany NM, Cai LF, Badiola I, Kase B, Liu J, Hughes C, Israelite CL, Nelson CL (2019) A prospective randomized open-label study of single injection versus continuous adductor canal block for postoperative analgesia after total knee arthroplasty. Bone Joint J 101-B:340–347
Elsey NM, Tobias JD, Klingele KE, Beltran RJ, Bhalla T, Martin D, Veneziano G, Rice J, Tumin D (2017) A prospective, double-blinded, randomized comparison of ultrasound-guided femoral nerve block with lateral femoral cutaneous nerve block versus standard anesthetic management for pain control during and after traumatic femur fracture repair in the pediatric population. J Pain Res 10:2177–2182
Fenten MGE, Bakker SMK, Scheffer GJ, Wymenga AB, Stienstra R, Heesterbeek PJC (2018) Femoral nerve catheter vs local infiltration for analgesia in fast track total knee arthroplasty: short-term and long-term outcomes. Br J Anaesth 121:850–858
Gudmundsdottir S, Franklin JL (2017) Continuous adductor canal block added to local infiltration analgesia (LIA) after total knee arthroplasty has no additional benefits on pain and ambulation on postoperative day 1 and 2 compared with LIA alone. Acta Orthop 88:537–542
Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW (2017) Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplast 32:3854–3860
Hospodar PP, Ashman ES, Traub JA (1999) Anatomic study of the lateral femoral cutaneous nerve with respect to the ilioinguinal surgical dissection. J Orthop Trauma 13:17–19
Husted H, Lunn TH, Troelsen A, Gaarn-Larsen L, Kristensen BB, Kehlet H (2011) Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop 82:679–684
Kampitak W, Tanavalee A, Ngarmukos S, Amarase C (2019) Opioid-sparing analgesia and enhanced recovery after total knee arthroplasty using combined triple nerve blocks with local infiltration analgesia. J Arthroplast 34:295–302
Kastelik J, Fuchs M, Krämer M, Trauzeddel RF, Ertmer M, von Roth P, Perka C, Kirschbaum SM, Tafelski S, Treskatsch S (2019) Local infiltration anaesthesia versus sciatic nerve and adductor canal block for fast-track knee arthroplasty: a randomised controlled clinical trial. Eur J Anaesthesiol 36:255–263
Kim JH, Cho MR, Kim SO, Kim JE, Lee DK, Roh WS (2012) A comparison of femoral/sciatic nerve block with lateral femoral cutaneous nerve block and combined spinal epidural anesthesia for total knee replacement arthroplasty. Korean J Anesthesiol 62:448–453
Kulkarni M, Mallesh M, Wakankar H, Prajapati R, Pandit H (2019) Effect of methylprednisolone in periarticular infiltration for primary Total knee arthroplasty on pain and rehabilitation. J Arthroplast 34:1646–1649
Laoruengthana A, Rattanaprichavej P, Rasamimongkol S, Galassi M (2017) Anterior vs posterior periarticular multimodal drug injections: a randomized, controlled trial in simultaneous bilateral total knee arthroplasty. J Arthroplast 32:2100–2104
Li D, Ma GG (2016) Analgesic efficacy and quadriceps strength of adductor canal block versus femoral nerve block following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2614–2619
Li D, Tan Z, Kang P, Shen B, Pei F (2017) Effects of multi-site infiltration analgesia on pain management and early rehabilitation compared with femoral nerve or adductor canal block for patients undergoing total knee arthroplasty: a prospective randomized controlled trial. Int Orthop 41:75–83
Li D, Zhao J, Yang Z, Kang P, Shen B, Pei F (2019) Multiple low doses of intravenous corticosteroids to improve early rehabilitation in Total knee arthroplasty: a randomized clinical trial. J Knee Surg 32:171–179
Nader A, Kendall MC, Manning DW, Beal M, Rahangdale R, Dekker R, De Oliveira GS Jr, Kamenetsky E, McCarthy RJ (2016) Single-dose adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia after total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 41:678–684
Nersesjan M, Hägi-Pedersen D, Andersen JH, Mathiesen O, Dahl JB, Broeng L, Thybo KH (2018) Sensory distribution of the lateral femoral cutaneous nerve block - a randomised, blinded trial. Acta Anaesthesiol Scand 62:863–873
Nielsen TD, Moriggl B, Barckman J, Kølsen-Petersen JA, Søballe K, Børglum J, Bendtsen TF (2018) The lateral femoral cutaneous nerve: description of the sensory territory and a novel ultrasound-guided nerve block technique. Reg Anesth Pain Med 43:357–366
Parvizi J, Miller AG, Gandhi K (2011) Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am 93:1075–1084
Pinsornsak P, Nangnual S, Boontanapibul K (2017) Multimodal infiltration of local anaesthetic in total knee arthroplasty; is posterior capsular infiltration worth the risk? A prospective, double-blind, randomised controlled trial. Bone Joint 99-B:483–488
Soffin EM, YaDeau JT (2016) Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth 117:iii62–iii72
Sogbein OA, Sondekoppam RV, Bryant D, Johnston DF, Vasarhelyi EM, MacDonald S, Lanting B, Ganapathy S, Howard JL (2017) Ultrasound-guided motor-sparing knee blocks for postoperative analgesia following total knee arthroplasty: a randomized blinded study. J Bone Joint Surg Am 99:1274–1281
Tang J, Li K, Ren J, Liu J, Xie S, Song D (2012) Anatomic characteristics and clinic significance of the lateral femoral cutaneous nerve. Zhong Nan Da Xue Xue Bao Yi Xue Ban 37:1255–1259
Tifford CD, Spero L, Luke T, Plancher KD (2000) The relationship of the infrapatellar branches of the saphenous nerve to arthroscopy portals and incisions for anterior cruciate ligament surgery. An anatomic study. Am J Sports Med 28:562–567
Tsukada S, Wakui M, Hoshino A (2015) Pain control after simultaneous bilateral total knee arthroplasty: a randomized controlled trial comparing periarticular injection and epidural analgesia. J Bone Joint Surg Am 97:367–373
Wang Q, Yue Y, Li D, Yang Z, Yeersheng R, Kang P (2019) Efficacy of single-shot adductor canal block combined with posterior capsular infiltration on postoperative pain and functional outcome after total knee arthroplasty: a prospective, double-blind, randomized controlled study. J Arthroplast 34:1650–1655
Xie X, Pei F, Huang Z, Tan Z, Yang Z, Kang P (2015) Does patellar denervation reduce post-operative anterior knee pain after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 23:1808–1815
Acknowledgments
We want to express our sincere appreciation for all the patients that joined this study.
Funding
Science and technology program of Sichuan Province (Grant ID: 2019YFS0123).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Clinical Trials and Biomedical Ethics Committee of West China Hospital, and written informed consents were obtained from all participants. This study was approved by the institutional review board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, D., Alqwbani, M., Wang, Q. et al. Ultrasound-guided adductor canal block combined with lateral femoral cutaneous nerve block for post-operative analgesia following total knee arthroplasty: a prospective, double-blind, randomized controlled study. International Orthopaedics (SICOT) 45, 1421–1429 (2021). https://doi.org/10.1007/s00264-020-04549-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04549-2