Abstract
Purpose
To assess how the level of the deformity, the stage of the osteoarthritic process, and the role of additional surgeries impact radiographic and clinical outcomes following an extra-articular medial closing supramalleolar osteotomy for treatment of post-traumatic valgus ankle osteoarthritis.
Methods
About 56 consecutive patients who underwent an extra-articular medial closing wedge osteotomy for post-traumatic valgus ankle osteoarthritis were retrospectively analyzed. Subgroups were formed according to the pre-operative level of deformity and preoperative stage of ankle osteoarthritis. Additional surgical steps required to achieve a properly balanced hindfoot were also noted. Radiographic and clinical outcomes of each subgroup were compared with each other, and the role of additional surgical steps required to achieve a balanced hindfoot was investigated.
Results
Radiographic and clinical outcomes improved significantly between pre-operative assessment and the last follow-up. Patients with a pre-operative supramalleolar deformity showed superior radiographic outcomes compared to patients with an intra-articular deformity. Clinical outcomes did not differ significantly between these two subgroups. The pre-operative stage of ankle osteoarthritis significantly impacted radiographic outcomes but did not influence clinical outcome measures. An additional fibula or calcaneus osteotomy was necessary for 55% and 23% of all patients, respectively.
Conclusion
Extra-articular medial closing supramalleolar osteotomies show satisfactory mid- to long-term radiographic and clinical outcomes in patients with post-traumatic valgus ankle osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Supramalleolar osteotomies for treatment of early- to mid-stage ankle osteoarthritis have become more popular in recent years [1,2,3,4,5,6,7,8]. Because supramalleolar osteotomies can correct osseous deformities without sacrificing the ankle joint, this technique is of particular interest in the treatment of ankle osteoarthritis in young and physically active patients [6]. This is especially important as long-term outcomes after joint sacrificing procedures, like total ankle replacements or fusions, are associated with certain complications (e.g., degenerative changes of the adjacent joints) [9,10,11].
Recent research has mainly focused on the utility of supramalleolar osteotomies in the treatment of varus ankle osteoarthritis [2,3,4,5, 7, 8]. However, only limited evidence is available on mid- to long-term radiographic and clinical outcomes of supramalleolar osteotomies in posttraumatic valgus ankle osteoarthritis. Additionally, the impact of the pre-operative level of deformity, pre-operative stage of ankle osteoarthritis, and the role of additional surgical steps needed to balance the hindfoot are poorly understood.
The aim of this study was to report on mid- to long-term radiographic and clinical outcomes in patients treated with an extra-articular medial closing supramalleolar osteotomy for post-traumatic valgus ankle osteoarthritis. The impact of the pre-operative level of deformity, preoperative stage of ankle osteoarthritis, and the role of additional surgical steps were also investigated.
Materials and methods
Inclusion and exclusion criteria
Institutional Review Board approval (Ethics Committee Northwest/ Central Switzerland, #2017-02286) was obtained, and the study was conducted in accordance with the Declaration of Helsinki and the guidelines for Good Clinical Practice. Informed consent was available from all individual participants included in the study. A retrospective analysis of patients treated with an extra-articular medial closing wedge osteotomy for post-traumatic (patients with history of a fracture of the tibia and/or fibula and/or post-traumatic chronic ligamentous instability) valgus ankle osteoarthritis was performed. Exclusion criteria were patients with primary ankle osteoarthritis, patients who had a correcting osteotomy in multiple planes (e.g., coronal and sagittal), patients with a history of subtalar fusion, and patients with end-stage (e.g., ankle joint obliteration of > 50% on the mortise view) ankle osteoarthritis. About 56 consecutive patients who underwent surgery between April 2007 and December 2016 were ultimately included (Fig. 1). Baseline characteristics of the included patients are available in Supplemental Table I.
Radiographic and clinical assessment
Radiographic and clinical assessment was performed pre-operatively, two and four months post-operatively, and thereafter annually. Weight-bearing radiographs of the foot and ankle (mortise and lateral view) were performed at each visit. The medial distal tibial surface angle (TAS) and the tibiotalar angle (TTS) were assessed on the mortise view [12]. The tilt of the talus in the ankle mortise was calculated by subtracting the TTS from the TAS [12]. The tibial lateral surface angle (TLS) was assessed on lateral radiographs [12]. Measurements on conventional radiographs were performed in a randomized order by a fellowship trained orthopaedic surgeon (NK). Previous studies have shown good reliability for the angular measurements used in this study [13,14,15]. Valgus ankle osteoarthritis was defined as follows: clinical (pain and swelling around the ankle joint which impair physical activities) and radiographic (joint space narrowing, and/or subchondral sclerosis, and/or subchondral cysts formation, and/or periarticular osteophytes) evidence of ankle osteoarthritis as well as either a TAS of ≥ 92 degrees or a valgus talar tilt in the ankle mortise of ≥ 4 degrees [1, 8, 16]. To ensure a homogenous cohort, patients with a talo-first metatarsal (Meary’s) angle of > 5 degrees were excluded from this study [17]. Thus, patients with radiographic evidence of flat foot deformity – due to osteoarthritic changes at the level of the mid-tarsal joints or tibialis posterior tendon dysfunction with a concomitant break through the talo-navicular or naviculo-cuneiform joint and subluxation at the level of the subtalar joint (inframalleolar deformity) – were not considered for this study.
The TAS and talar tilt were used to distinguish between patients with a supramalleolar and patients with an intraarticular deformity. A supramalleolar deformity was defined as having a TAS of ≥ 92 degrees and the center of rotation of angulation (CORA) located supramalleolarly (mortise view, Fig. 2-A). An intra-articular deformity was defined as a talar tilt of ≥ 4 degrees (incongruent ankle joint, Fig. 2-B) [1]. All included patients either showed a supramalleolar (N = 20) or an intra-articular deformity (N = 36). Patients with either a combined deformity or a TAS of ≥ 92 degrees with the deformity located at the level of the distal tibial articular surface and a talar tilt of < 4 degrees (corresponds to an intra-articular deformity) were not available. In addition, three subgroups were formed according to the pre-operative tilt of the talus in the ankles mortise: ankles with a tilt of < 4 degrees (N = 20), 4–10 degrees (N = 27), and > 10 degrees (N = 9) [1, 6, 8]. The stage of ankle osteoarthritis was divided into two subgroups: one subgroup consisted of patients with lateral joint space narrowing but no obliteration (N = 33), while the second subgroup contained patients where lateral obliteration of the joint space was evident on the mortise view (N = 23). Clinical assessment included ankle range of motion (ROM; determined with a goniometer) and pain rated on a visual analogue scale (VAS) ranging from 0 (no pain) to 10 points (maximum pain) [18]. The American Orthopedic Foot & Ankle Society (AOFAS) Hindfoot score was also assessed at each visit. The clinical examination was done by research associates who were otherwise not involved in the treatment.
Assessment of the level of deformity and stage of ankle osteoarthritis. (2-A) Supramalleolar deformity with a congruent ankle joint (tibiotalar tilt < 4 degrees). A circle fitting into the distal part of the tibia was drawn, touching the medial and lateral cortex as well as the distal articular surface. The center of the distal articular surface was defined as the intersection of the circle and the distal articular surface. A line from the center of the distal articular surface crossing the middle of the circle was defined as the axis of the distal tibia (*). In addition, the tibial shaft axis was drawn, defined as a line crossing two circles eight and 13 cm above the ankle joint (**). In the case of the supramalleolar deformity, both axes are crossing above the ankle joint at the centre of rotation and angulation (CORA). The tibial articular surface angle (TAS) and tibiotalar tilt (TTS) are defined as the angles between the tibial shaft axis and the distal articular surface of the tibia (TAS) or the articular surface of the talus (TTS), respectively. (2-B) In this example, the level of deformity is intra-articular, which is incongruent (tibiotalar tilt ≥ 4 degrees). In addition, there is lateral tibiotalar joint obliteration (arrow). The axis of the distal part of the tibia and the axis of the tibial shaft are in the same line
Surgical technique
A medial approach to the distal tibia was performed, and two 1.6-mm Kirschner (K)-wires were used to mark an oblique osteotomy [19, 20]. An overcorrection of 2 to 5 degrees was anticipated [19, 20]. If the ankle joint was incongruent (tibiotalar tilt of ≥ 4 degrees) after fixation of the osteotomy, an oblique fibula osteotomy was done [21]. In the case of a persisting hindfoot valgus, a calcaneal osteotomy was performed [21]. Ligament reconstruction was performed when ankle instability was evident after hindfoot realignment [21]. Lateral ligament reconstruction included the anterior talofibular ligament as well as the calcaneofibular ligament. Medial ligament reconstruction included the superficial part of the deltoid ligament. An anchor (3.0 mm SutureTak®, Arthrex, Naples, FL, USA) was used for reconstruction. Posterior tibial tendon reconstruction included a debridement and reconstruction of the insertion at the navicular bone using an anchor (3.0 mm SutureTak®, Arthrex, Naples, FL, USA). An additional reconstruction of the insertion of the spring ligament at the navicular bone was performed at the same time. Additional procedures are summarized in Supplemental Table II. Post-operative rehabilitation included a short leg cast and touch ground weight-bearing for eight weeks, followed by a gradual return to full activity [20].
Statistical methods
Statistical significance level was set as P < .05. As repeated measurements were made per patient over time, mixed-effects models with patient ID as random effects (R package lme4) were used for the assessment of potential effects from covariates on variables of interest [22]. Collinearity was determined using variance inflation factors, and model compliance with underlying assumptions was assessed using residual plots. Nested models were compared using likelihood ratio tests for covariate selection. The Tukey method was used for post hoc multiple comparisons between individual groups. To assess the differences between cohorts at a single time point, either an independent Student’s t-test (given variance homoscedasticity), a Welch’s t-test (given variance heteroscedasticity), or a Kruskal-Wallis test (given violation of normality assumption) was carried out for continuous data. Assumption of normality in our data and variance homogeneity were tested using the Shapiro-Wilk test and the Levene’s test, respectively. Differences between proportions were assessed using Fisher’s exact test. If data was not available (e.g., missing last clinical follow-up), the patient was excluded for statistical analysis requiring this date. The analysis was performed in R (v3.4.3) using RStudio (v1.1.42) [23].
Results
The mean follow-up was performed at 36 (standard deviation [SD] 30, range 5–105) months post-operatively. Radiographic assessment at two months post-operative was missing for four patients (7%). A missing radiographic or clinical final follow-up was reported for 11 patients (20%). Patients either moved abroad or were deceased for reasons not related to the surgical procedure. Two patients (4%) had the last clinical and radiographic follow-up earlier than 12 months after surgery (after 5 and 8 months, respectively). They also moved abroad and were not anymore available for any clinical or radiographic follow-up.
Radiographic and clinical outcomes improved significantly between preoperative assessment and at the last follow-up, except for the TLS (Table 1). The TAS significantly decreased in both patients with a supramalleolar and patients with an intraarticular deformity (Fig. 3-A). Pre-operative TTS did not differ significantly between patients with a supramalleolar and patients with an intra-articular deformity (Fig. 3-B). TTS decreased significantly at the two month post-operative follow-up and remained stable over time. The tilt of the talus in the ankle mortise was significantly higher in patients with an intra-articular deformity (pre-operative, 2-month post-operative, last follow-up) compared to patients with a supramalleolar deformity (Fig. 3-C). Patients with an obliteration of the joint space as well as patients with a higher pre-operative tilt of the talus in the ankle mortise showed a significantly lower TAS and significantly higher TTS at the last follow-up (Table 2). The aetiology of ankle osteoarthritis, the pre-operative stage of ankle osteoarthritis, and the pre-operative tilt of the talus in the ankle mortise did not significantly impact clinical outcome measures (Table 3). The stage of ankle osteoarthritis remained the same for each patient over the study period. A tibiotalar tilt < 4 degrees (congruent ankle joint) at the last follow-up could be achieved in 17 out of 36 patients (47%) with an intra-articular deformity (Figs. 4 and 5).
Radiographic parameters describing the ankle alignment in the coronal plane pre-operatively (PreOP), two months post-operatively (2-M FU), and at the last follow-up (Last FU). (3-A) The mean distal tibial articular surface angle (TAS) in the case of a supramalleolar deformity was 96.6 (standard deviation [SD] 2.5) degrees before surgery, declined by 8.5 degrees by the two month follow-up (P < .0001), and then remained stable (P = .974) until the last follow-up. The pre-operative TAS in patients with an intra-articular deformity was 89.8 (SD 1.9) degrees, declined by 5.5 degrees after surgery (P < .0001), and then remained stable until the last follow-up (P = .329). The mean TAS of patients with an intra-articular deformity was 6.8 degrees (pre-operative), 3.9 degrees (2-month post-operative follow-up), and 4.9 degrees (last follow-up) smaller (each P < .0001) than in patients with a supramalleolar deformity. (3-B) The mean tibiotalar angle (TTS) did not vary between patients with a supramalleolar and patients with an intra-articular deformity. Surgery reduced TTS from 97.1 (SD 4.1) to 87.9 (SD 3.4) degrees, evaluated at the two month follow-up (P < .001). The TTS remained stable until the last follow-up (P = .736). (3-C) At any time point, the mean tilt in patients with a supramalleolar deformity was significantly (each P < .006) smaller than in patients with an intra-articular deformity. In patients with an intra-articular deformity, the mean tilt declined after surgery by 3.7 degrees (P < .0001) and remained constant until the last follow-up (P = .568). In contrast, no significant change over time was evident in patients with a supramalleolar deformity
Example of a 39-year-old patient suffering from post-traumatic valgus ankle osteoarthritis. The osseous deformity is located supramalleolarly. (4-A) Mortise view pre-operative. A valgus deformity of the distal tibia is evident. The ankle joint is congruent with a slight narrowing lateral and subchondral sclerosis. (4-B) Lateral view. (4-C) Mortise view at 12 months post-operative following a supramalleolar medial closing osteotomy of the tibia. The distal tibial articular surface angle (TAS) is slightly overcorrected. The ankle mortise appears symmetrical. Of note, the osseous correction has been performed distally to the centre of rotation of angulation (CORA). Translation of the distal in relation to the proximal part of the osteotomized bone is possible. (4-D) Lateral view. (4-E) Mortise view 7 years post-operatively. The achieved correction is stable, and the osteoarthritic process has not progressed. (4-F) Lateral view
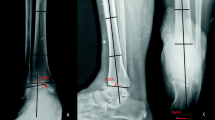
Example of a 71-year-old patient suffering from post-traumatic valgus ankle osteoarthritis. The osseous deformity is intra-articular. (5-A) Mortise view pre-operative. The distal articular surface angle (TAS) is within normal anatomic range. The ankle joint is incongruent and obliterated laterally. (5-B) Lateral view. (5-C) Mortise view at 2 months post-operative following a supramalleolar medial closing osteotomy of the tibia and a medial sliding osteotomy of the calcaneus. The distal tibial articular surface angle (TAS) is slightly overcorrected. Persistent tilt of the talus in the ankle mortise. (5-D) Lateral view. (5-E) Mortise view 12 months post-operative. Due to ongoing pain and swelling at the level of the ankle joint, the patient underwent a total ankle replacement. (5-F) Lateral view
An additional fibula osteotomy was necessary in around half of the patients and was more frequently performed in patients with an intra-articular deformity (Supplemental Table III). A calcaneus osteotomy was necessary in around a quarter of all patients and was also more frequently performed in patients with an intra-articular deformity. Medial ligament reconstruction was more frequently performed than lateral ligament reconstruction and was only necessary in patients with an intra-articular deformity. Pre- and post-operative radiographic and clinical outcome measures did not differ significantly between patients with and without an additional fibula osteotomy (Supplemental Table III). The pre- and post-operative tilt of the talus in the ankle mortise differed significantly between patients with and without an additional calcaneus osteotomy. In the case of a combined fibula and calcaneal osteotomy, no significant difference in the post-operative tilt of the talus in the ankle mortise compared to patients without additional osteotomies was evident.
Four patients (7%) underwent a secondary total ankle replacement or an ankle fusion. Total ankle replacements and ankle fusions were performed at 12 and 58 months and 11 and 28 months after the supramalleolar correction, respectively. The pre-operative level of deformity was intra-articular in three patients. In the same three patients, obliteration of the lateral part of the ankle joint was evident, and a talar tilt of > 10 degrees was noted. Other complications included delayed union (two patients, 4%) and delayed wound healing (two patients, 4%). No further surgery was required in those patients. Hardware removal was performed in 31 patients (55%). Hardware removal was proposed 12 months post-operatively for every patient in order to minimize possible complications associated with late hardware removal.
Discussion
A retrospective case study was performed investigating the impact of pre-operative osseous deformities on clinical and radiographic outcomes following an extra-articular supramalleolar osteotomy in patients suffering from post-traumatic valgus ankle osteoarthritis. The three most relevant findings were as follows: (I) supramalleolar osteotomies showed satisfactory radiographic and clinical outcomes for treatment of early- to mid-stage valgus ankle osteoarthritis; (II) patients with a supramalleolar deformity showed better radiographic outcomes compared to patients with an intra-articular deformity, while clinical outcome measures did not significantly differ between the two subgroups; and (III) additional surgical steps were necessary for a substantial part of the patients to achieve a balanced and stable hindfoot.
Only a few articles are available investigating mid- to long-term results in patients treated with a supramalleolar osteotomy for post-traumatic valgus ankle osteoarthritis [1, 6, 24]. Comparable radiographic and clinical outcomes were described for a cohort with a mean follow-up of 7.1 years that underwent either a medial closing or lateral opening wedge osteotomy in addition to an oblique osteotomy and lengthening of the fibula [24]. Another study investigated the effect of a supramalleolar osteotomy in 61 consecutive patients suffering from valgus ankle osteoarthritis (mixed etiology and various operative techniques used) at a mean of 43 months [1]. Patients were subdivided according to the tilt of the talus, the remaining ankle joint space, and malalignment in the sagittal plane [1]. Similar to the present study, both the AOFAS and VAS score significantly improved, but radiographic outcome measures did not significantly differ between the subgroups [1]. More recently, a consecutive cohort of 294 patients suffering from either varus or valgus ankle osteoarthritis was retrospectively analyzed at a mean of 5.0 years (mixed aetiology and various operative techniques used). Age at the time of surgery and the pre-operative stage of ankle osteoarthritis were identified as risk factors for failure [6]. The available studies failed to report whether the location of the deformity impact clinical and radiographic outcomes. Also, different operative techniques were used in each study, potentially limiting the generalization of the findings.
The radiographic outcome following supramalleolar osteotomy is highly dependent on the pre-operative level of the deformity. In the case of a pre-operative supramalleolar deformity, the pre- and post-operative talar tilt in the ankle mortise was < 4 degrees (congruent joint) in all patients; no obliteration of the ankle joint was evident in most cases. In contrast, patients with an intra-articular deformity evidenced a pre-operative tibiotalar tilt of ≥ 4 degrees (incongruent joint), as well as an obliteration of the joint space laterally. Realignment surgery of the hindfoot may enable correction of an incongruent ankle joint with a low tibiotalar tilt (e.g., ≤ 10 degrees), while ankles with a high pre-operative tibiotalar tilt (e.g., > 10 degrees) remain incongruent post-operatively. Interestingly, a consistent talar tilt post-operatively did not impact clinical outcome measures. It could be argued that the correcting pull of the Achilles tendon after realignment surgery unloads the lateral part of the ankle joint. This may result in decreased peak pressure and decreased pain when ambulating, regardless of whether the ankle joint is congruent or not. In addition, patients with a low tibiotalar tilt/early stage of ankle osteoarthritis may have a correctable deformity, while patients with a higher tibiotalar tilt/ advanced stage of ankle osteoarthritis possibly have a more fixed deformity. This may be the reason why a supramalleolar osteotomy impacts the tibiotalar tilt in patients with a low tibiotalar tilt, while no change could not be observed in patients with a high tibiotalar tilt.
Whether or not additional osteotomies will be necessary to ensure proper balancing of the hindfoot is difficult to predict pre-operatively. No significant difference for any of the pre- and post-operatively assessed radiographic parameters was evident between patients with or without an additional fibula osteotomy. However, patients who underwent a combined fibula and calcaneus osteotomy did have a significantly higher pre-operative tibiotalar tilt compared to patients without additional osteotomies. No significant difference between the same subgroups was evident post-operatively, indicating that an additional fibula and calcaneus osteotomy sufficiently addressed the remaining deformity after the supramalleolar correction was performed. Nevertheless, a thorough intraoperative assessment after the supramalleolar correction is necessary to ensure no additional surgical steps are necessary. Widening at the medial gutter, shortening of the fibula, and a residual valgus hindfoot alignment should especially be noted [20, 21, 25].
This study has several limitations. First, multiple additional procedures (e.g., calcaneal osteotomies, fibula osteotomy) were necessary for proper correction of the deformity. Although the supramalleolar correction is the most important step to realign the hindfoot, the impact of these procedures on clinical and radiographic outcomes is difficult to predict. Second, no whole leg radiographs were available for pre-operative planning. Possible deformities at the level of the knee or hip joint would not have been detected pre-operatively. Such deformities may have impacted decision-making. Third, the total number of patients included in this study was relatively small. Consequently, statistical comparisons – especially between subgroups – have to be interpreted with care.
To conclude, an extra-articular medial closing supramalleolar osteotomy shows satisfactory mid- to long-term radiographic and clinical outcomes in patients with early- to mid-stage post-traumatic valgus ankle osteoarthritis. A thorough pre-operative assessment is necessary to identify those patients who would benefit from this treatment option.
References
Knupp M, Stufkens SA, Bolliger L, Barg A, Hintermann B (2011) Classification and treatment of supramalleolar deformities. Foot Ankle Int 32(11):1023–1031
Lee WC, Moon JS, Lee K, Byun WJ, Lee SH (2011) Indications for supramalleolar osteotomy in patients with ankle osteoarthritis and varus deformity. J Bone Joint Surg Am 93(13):1243–1248. https://doi.org/10.2106/JBJS.J.00249
Ahn TK, Yi Y, Cho JH, Lee WC (2015) A cohort study of patients undergoing distal tibial osteotomy without fibular osteotomy for medial ankle arthritis with mortise widening. J Bone Joint Surg Am 97(5):381–388. https://doi.org/10.2106/JBJS.M.01360
Hongmou Z, Xiaojun L, Yi L, Hongliang L, Junhu W, Cheng L (2016) Supramalleolar osteotomy with or without fibular osteotomy for varus ankle arthritis. Foot Ankle Int 37(9):1001–1007. https://doi.org/10.1177/1071100716649926
Hintermann B, Ruiz R, Barg A (2017) Novel double osteotomy technique of distal tibia for correction of asymmetric varus osteoarthritic ankle. Foot Ankle Int 38(9):970–981. https://doi.org/10.1177/1071100717712543
Krahenbuhl N, Zwicky L, Bolliger L, Schadelin S, Hintermann B, Knupp M (2017) Mid- to long-term results of Supramalleolar osteotomy. Foot Ankle Int 38(2):124–132. https://doi.org/10.1177/1071100716673416
Haraguchi N, Ota K, Tsunoda N, Seike K, Kanetake Y, Tsutaya A (2015) Weight-bearing-line analysis in supramalleolar osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Am 97(4):333–339. https://doi.org/10.2106/JBJS.M.01327
Krahenbuhl N, Akkaya M, Deforth M, Zwicky L, Barg A, Hintermann B (2019) Extraarticular supramalleolar osteotomy in asymmetric varus ankle osteoarthritis. Foot Ankle Int. https://doi.org/10.1177/1071100719845928
Sokolowski M, Krahenbuhl N, Wang C, Zwicky L, Schweizer C, Horn Lang T, Hintermann B (2019) Secondary Subtalar joint osteoarthritis following total ankle replacement. Foot Ankle Int. https://doi.org/10.1177/1071100719859216
Daniels TR, Younger AS, Penner M, Wing K, Dryden PJ, Wong H, Glazebrook M (2014) Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am 96(2):135–142. https://doi.org/10.2106/JBJS.L.01597
Sheridan BD, Robinson DE, Hubble MJ, Winson IG (2006) Ankle arthrodesis and its relationship to ipsilateral arthritis of the hind- and mid-foot. J Bone Joint Surg (Br) 88(2):206–207. https://doi.org/10.1302/0301-620X.88B2.17065
Krahenbuhl N, Siegler L, Deforth M, Zwicky L, Hintermann B, Knupp M (2019) Subtalar joint alignment in ankle osteoarthritis. Foot Ankle Surg 25(2):143–149. https://doi.org/10.1016/j.fas.2017.10.004
Magerkurth O, Knupp M, Ledermann H, Hintermann B (2006) Evaluation of hindfoot dimensions: a radiological study. Foot Ankle Int 27(8):612–616
Nosewicz TL, Knupp M, Bolliger L, Hintermann B (2012) The reliability and validity of radiographic measurements for determining the three-dimensional position of the talus in varus and valgus osteoarthritic ankles. Skelet Radiol 41(12):1567–1573. https://doi.org/10.1007/s00256-012-1421-6
Stufkens SA, Barg A, Bolliger L, Stucinskas J, Knupp M, Hintermann B (2011) Measurement of the medial distal tibial angle. Foot Ankle Int 32(3):288–293. https://doi.org/10.3113/FAI.2011.0288
Yi Y, Cho JH, Kim JB, Kim JY, Park SY, Lee WC (2017) Change in talar translation in the coronal plane after mobile-bearing total ankle replacement and its association with lower-limb and Hindfoot alignment. J Bone Joint Surg Am 99(4):e13. https://doi.org/10.2106/JBJS.15.01340
Akoh CC, Phisitkul P (2019) Clinical examination and radiographic assessment of the cavus foot. Foot Ankle Clin 24(2):183–193. https://doi.org/10.1016/j.fcl.2019.02.002
Huskisson EC (1974) Measurement of pain. Lancet 2(7889):1127–1131
Hintermann B, Knupp M, Barg A (2016) Supramalleolar osteotomies for the treatment of ankle arthritis. J Am Acad Orthop Surg 24(7):424–432. https://doi.org/10.5435/JAAOS-D-12-00124
Hintermann B, Zwicky L, Schweizer C, Ruiz R, Barg A (2017) The use of supramalleolar osteotomies in posttraumatic deformity and arthritis of the ankle. JBJS Essent Surg Tech 7(4):e29. https://doi.org/10.2106/JBJS.ST.16.00081
Knupp M (2017) The use of osteotomies in the treatment of asymmetric ankle joint arthritis. Foot Ankle Int 38(2):220–229. https://doi.org/10.1177/1071100716679190
Douglas Bates MM, Bolker B, Walker S (2015) Fitting Linear Mixed-Effects Models Using lme4. J Stat Softw 67(1):1–48. https://doi.org/10.18637/jss.v067.i01
R Core Team (2015) R: A language and environment for statistical computing. R Foundation for Statistical Computing 2015; Vienna, Austria. (http://www.R-project.org/)
Hintermann B, Barg A, Knupp M (2011) Corrective supramalleolar osteotomy for malunited pronation-external rotation fractures of the ankle. J Bone Joint Surg (Br) 93(10):1367–1372. https://doi.org/10.1302/0301-620X.93B10.2694
Weber BG, Simpson LA (1985) Corrective lengthening osteotomy of the fibula. Clin Orthop Relat Res 199:61–67
Acknowledgments
The authors thank Maxwell Weinberg, a study coordinator at the University of Utah Orthopedic Center, who provided editorial support.
Funding
This work was supported by a grant from the University of Basel (Excellent Junior Research Grant).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Alexej Barg has received personal fees from Medartis (not related to the article) during the conduct of the study. Nicola Krähenbühl, Roman Susdorf, and Beat Hintermann declare that they have no conflict of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level IV, retrospective case series
Rights and permissions
About this article
Cite this article
Krähenbühl, N., Susdorf, R., Barg, A. et al. Supramalleolar osteotomy in post-traumatic valgus ankle osteoarthritis. International Orthopaedics (SICOT) 44, 535–543 (2020). https://doi.org/10.1007/s00264-019-04476-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04476-x