Abstract
Purpose
To evaluate and compare the effectiveness of the modified Heuter approach and the Kocher-Langenbeck approach in the treatment of Pipkin type I and II femoral head fractures.
Methods
The study cohort consisted of 39 patients with Pipkin type I or type II femoral head fractures who were treated by open reduction and internal fixation through the modified Heuter approach (the Heuter group) or the Kocher-Langenbeck approach (the K-L group) between June 2013 and January 2016. Standard radiographs and computed tomography (CT) scans were obtained before surgery and during the follow-up. The two approaches were compared in reference to operative time, amount of blood loss, the occurrence of complications, and final functional outcome. The Brooker classification was used to document heterotopic ossification and the Thompson-Epstein scores were used for final evaluation.
Results
The mean operative time and estimated blood loss in the Heuter group were lower than those in the K-L group (P < 0.001 for both measures). The incisions healed primarily in all patients after surgery, no infection or deep venous thromboses were detected in either group, post-operative imaging data showed that dislocation and fractures were reduced, and the fractures finally achieved bony union. There were no significant differences in the incidence of complications or final functional outcomes between the two groups.
Conclusions
Compared with the Kocher-Langenbeck approach, the modified Heuter approach can effectively reduce the blood loss and operative time without increasing the risk of complications; this approach is simple, straightforward, and atraumatic and may be a viable option for open reduction and internal fixation of Pipkin type I and type II femoral head fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoral head fractures are relatively uncommon injuries, mostly caused by high-energy damage, such as traffic accidents, falls from a height, industrial accidents, and sports injury. In 1896, when Birkett [1] first described the fracture of the femoral head, the incidence of this injury was low and always associated with traumatic posterior hip dislocation. However, with the rapid development of society and economies, the incidence of this injury has increased steadily in recent years. Although several classification systems for femoral head fracture have been described in previous reports, the most widely used classification is still the Pipkin classification, which was proposed by Pipkin in 1957 [2]. This classification system is based on the location of the femoral head fracture in relation to the fovea and additional lesions on the femoral neck or acetabulum.
For the management of Pipkin type I and type II femoral head fractures, treatment with nonsurgical techniques often leads to difficulty in achieving a satisfactory effect, and obvious limitations in patient mobility and the high cost of prolonged admission have led to the abandonment of this method of treatment [3,4,5,6]. Therefore, for Pipkin type I and type II femoral head fractures, surgery is an effective option that can not only restore the anatomical structure of the hip joint but also enable patients to perform early functional training, resulting in better recovery of post-operative function. However, because of the limited numbers of patients, insufficient length of follow-up, and the use of nonvalidated outcome instruments, there is still no consensus on the management of Pipkin type I and type II injuries; the controversy mainly concentrates on the selection of optimal surgical approach [5, 7,8,9,10,11,12,13,14]. In this study, we retrospectively reviewed patients with Pipkin type I and type II femoral head fractures managed surgically through the modified Heuter anterior approach and posterior Kocher-Langenbeck approach, with the objective of defining the best approach with the least morbidity.
Patients and methods
Between June 2013 and January 2016, 39 patients were treated by open reduction and internal fixation using the modified Heuter approach in 21 cases (the Heuter group) and by the Kocher-Langenbeck approach in 18 cases (the K-L group); the baseline characteristics of the patients in both groups are summarized in Table 1. The two approaches were compared with reference to operative time, amount of blood loss, occurrence of complications, and final functional outcome.
All patients presented to our emergency department and then were assessed according to the Adult Trauma Life Support (ATLS™) guidelines, including a pelvis radiograph, CT scan, and three-dimensional reconstruction. At the same time, immediate closed reduction of the hip fracture dislocation was attempted under general anaesthesia, after which skeletal traction was essential to maintain the reduction.
To avoid examiner bias, clinical evaluations and post-operative follow-up were performed by two independent surgeons who were not involved in the surgical treatment of the patients. Serial radiographs were obtained before and immediately after surgery, as well as at one, two, three, six, 12, and 24 months after surgery and at final follow-up. During the follow-up, the scale of the Brooker classification [39] (Table 2) was used to classify heterotopic ossification when present, and avascular necrosis of the femoral head was mainly assessed by clinical symptoms (hip pain) and plain radiographs (pelvis and hip joint). At the final follow-up, the Thompson-Epstein [38] (Table 3) scores were used for final functional evaluation.
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS 20.0, IBM, New York City, USA). Categorical data were tabulated with frequencies or percentages, and continuous data were expressed as the mean ± standard deviation (SD). Normality was tested using the Kolmogorov-Smirnov test. Fisher’s exact probability test (n < 40) for categorical variables was used to compare patients’ characteristics at baseline. The independent sample t test was used to analyze intergroup comparisons for normally distributed continuous data. A P value of less than 0.05 was considered to be statistically significant.
Surgical technique
In the modified Heuter anterior approach (the Heuter group), the patient was placed supine on a radiolucent table. A bump was placed under the affected hip. The affected leg was draped free to enable traction, flexion, extension, and rotation of the hip without any interference. After several landmarks were identified, the modified Heuter anterior approach incision began approximately 2 cm lateral and 2 cm distal to the anterior superior iliac spine. This incision was over the muscle belly of the tensor fascia lata. The incision was performed distally and slightly posterior for approximately 10 cm. After skin incision, the dissection was carried down to the fascia overlying the muscle belly of the tensor fascia lata. The fascia was divided over the muscle belly; the lateral femoral cutaneous nerve was medial and thus spared. Blunt dissection was then used to develop the interval between the tensor fascia lata and the sartorius, working within the fascial sheath. The tensor muscle belly was retracted laterally while the sartorius was retracted medially; subsequently, the femoral neck could be palpated. The Hohmann retractors were placed medially and laterally around the femoral neck aiming to retract sartorius and rectus femoris medially, and the tensor and gluteus medius/minimus were retracted laterally. The femoral head and neck were centered between the retractors. At this point, the lateral femoral circumflex vessel leash was identified and subsequently ligated. An H-shaped capsulotomy was made, and the retractors were placed deep to the capsule and the femoral neck, then the femoral head and the fracture were exposed completely. Flexion, abduction, and external rotation of the hip brought the fracture site into view. Small or comminuted fragments of the femoral head remaining in the acetabulum were removed; the large fragments were reduced anatomically and temporarily fixed with Kirschner wires, which were sequentially replaced with bioabsorbable screws or cannulated screws. The heads of the screws were countersunk below the cartilage level. Any soft tissue attachments to the bone fragment were preserved to prevent further damage to the blood supply of the femoral head. For closure, the arthrotomy was repaired, as was the superficial fascia. The dermis and skin were then closed (Fig. 1).
a Identified landmarks and planned incision. b The Blunt dissection between the tensor fascia lata and the sartorius; the femoral neck can be touched through the gap. c The lateral femoral circumflex vessel was identified and subsequently ligated. d H-shaped capsulotomy. e Exposed fracture of femoral head. f The fracture was reduced and then fixed with cannulated screws
In the group of patients who were treated through the posterior Kocher-Langenbeck approach (the K-L group), surgery was performed with the patients in the lateral decubitus position on the contralateral side using a standard OR table. A Kocher-Langenbeck incision was made and the fascia lata was incised in line with the skin incision. The posterior border of the gluteus medius and minimus was identified and retracted to expose the posterosuperior aspect of the hip capsule. This retraction was facilitated by abduction and internal rotation of the limb. The piriformis tendon was tagged and released, but the short external rotators (quadratus femoris and obturator internus) were preserved, and the sciatic nerve was revealed and protected. After blunt dissection by periosteal elevator, a Hohmann retractor was used to retract the gluteus maximus, short external rotators, and sciatic nerve medially. We could see the femoral head was dislocated posteriorly, and if the posteroinferior capsule was torn seriously, in this step, we repaired the capsule with a heavy suture to prevent further inferior extension at the time of surgical dislocation. A Z-shaped capsulotomy was extended toward the acetabulum along the anterosuperior aspect of the femoral neck and then continued posteriorly along the acetabular rim, stopping at the superior edge of the piriformis tendon. Care was taken to avoid damaging the sciatic nerve and the acetabular labrum during this approach. Next, the hip was slowly and gently dislocated by flexion, adduction, and internal rotation, and the fractured fragment was handled, reduced, and stabilized in the same way as in the modified Heuter approach.
Post-operative management and aftercare
Intravenous antibiotics were given to prevent infection for 24 hours after operation and low molecular weight heparin was given to avoid deep venous thrombosis. Generally, the patients were encouraged to perform functional exercises of the quadratus femoris muscles on the second day after surgery. All patients were instructed to continue non-weight bearing for six to eight weeks post-operatively, then the patients were gradually increased from partial to full weight bearing. Radiographs were taken immediately after surgery, at one, two, three, six, 12, and 24 months after surgery, and at final follow-up. Once the radiographs showed fracture healing, progressive weight bearing and active exercises for the strengthening of the abductor muscles were started.
Results
The clinical outcomes between the two groups are listed in Table 4. The mean operative time for the Heuter group was 96.9 ± 14.8 minutes and for the K-L group was 131.8 ± 21.2 minutes (P < 0.001). The estimated blood loss was 103.3 ± 28.5 ml for the Heuter group and 334.5 ± 58.9 ml for the K-L group (P < 0.001). The incisions healed primarily in all patients after surgery; no infection or deep venous thrombosis was detected in either group, post-operative imaging data showed that dislocations and fractures were reduced, and the fractures ultimately achieved bony union.
During the follow-up, three patients in each group developed post-traumatic osteoarthritis. Heterotopic ossification (HO) was found in four patients in the Heuter group (the Brooker type II in three, type III in one) and two patients in the K-L group (the Brooker type I in one, type III in one). None of the patients with HO elected to undergo surgical excision of the ectopic bone, despite the limited hip flexion noted in the patients with type III. Avascular necrosis of the femoral head occurred in one patient (4.8%) of the Heuter group and one patient (5.6%) of the K-L group; the two patients were treated by total hip arthroplasty to improve limb function. There were no statistically significant differences between the two groups in the incidence of post-traumatic osteoarthritis (P = 1.000), HO (P = 0.667), or avascular necrosis of the femoral head (P = 1.000).
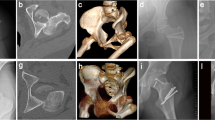
At the final follow-up, functional outcomes were assessed by the Thompson-Epstein scoring scale [38] (Table 3) in the two groups: scores were excellent in 12 cases, good in six cases, fair in two cases, and poor in one case for the Heuter group and excellent in nine cases, good in six cases, fair in two cases, and poor in one case for the K-L group (Fig. 2).
A 30-year-old male patient with right Pipkin II type femoral head fracture was treated by open reduction and internal fixation through the modified Heuter approach. Plain radiograph and CT 3-D reconstruction after injury (a–c). Plain radiograph and CT scan after closed reduction (d, e). Post-operative (f) and final follow-up (g–i) radiographs demonstrating an anatomic reduction
Discussion
Fracture of the femoral head is a relatively uncommon injury; typically, it occurs following traumatic posterior dislocation of the hip joint. About 5 to 15% of posterior hip dislocations have been reported to be associated with femoral head fracture [13, 15, 16].
The classic mechanism of injury for femoral head fracture is traumatic posterior hip dislocation [38]; when a powerful violence caused by trauma applied to the hip joint, the femoral head is believed to exit from the acetabulum posteriorly as the head forcibly shears against the acetabular rim, which leads to femoral head fracture [17]. Traumatic posterior hip dislocation is generally considered to be the result of an axially applied force to the femoral shaft with the hip positioned in flexion, adduction, and internal rotation; the most common cause is the so-called dashboard injury, which means the knee of a passenger striking the dashboard during a motor vehicle collision [18, 17]. The position of the leg at the time of the accident determines whether the hip dislocates with or without additional osseous lesions on the femoral head or the posterior wall of the acetabulum: if the hip flexion is greater than 60°, while the femoral head and acetabular posterior wall contact area is small, the fracture is most likely Pipkin type I or II type femoral head fracture; if the hip flexion is less than 60°, while the femoral head and acetabulum posterior wall contact surface is large, the axial compression is more transmitted to the hip. In this case, in addition to the occurrence of hip dislocation and fracture of the femoral head, the injury may also lead to acetabular and femoral neck fracture [12].
For the treatment of Pipkin type I and type II femoral head fractures, nonsurgical treatment often does not achieve a satisfactory outcome, and the obvious limitations in patient mobility and the high cost of prolonged admission have led to the abandonment of this method of treatment [3,4,5,6]. Therefore, for Pipkin type I and type II femoral head fractures, surgery is an effective option, which not only restores the anatomical structure of the hip joint but also enables patients to perform early functional training, which benefits the recovery of post-operative function. However, the question of which surgical approach is the best for femoral head fractures remains controversial, and the advantages and disadvantages of the different approaches have been the subject of previous studies [3].
The common surgical approaches that have been recommended include the Smith-Petersen approach, Kocher-Langenbeck approach, and Ganz approach [20, 19, 21, 22]. The Heuter approach was first described by German surgeon Heuter in the nineteenth century and mainly used for the treatment of hip tuberculosis, developmental hip dysplasia, and femoro-acetabular impingement [23]; subsequently, this approach has been modified and become popular for total hip arthroplasty [24, 23, 25,26,27,28,29,30,31]. In recent years, some surgeons began to apply the modified Heuter direct anterior approach for open reduction and internal fixation of femoral head fractures [32]. To the knowledge of the authors, no case-matched study comparing the modified Heuter direct anterior approach versus the Kocher-Langenbeck approach has been published. Compared with the Kocher-Langenbeck approach, the modified Heuter approach is simple, straightforward, and atraumatic, and the exposure provided is adequate to obtain reduction and fixation without the detachment of such muscles as tensor and abductors, which can effectively reduce blood loss during surgery. Another benefit of the approach is that it allows access to the hip joint in a very timely fashion; within a few minutes, the surgeon can directly access the femoral head, and fracture reduction can be accomplished under direct visualization, which can considerably save operative time as well as avoid re-injury of hip blood supply.
In addition, we found that the patients treated with the modified Heuter approach can also obtain satisfactory outcomes without increased incidence of complications. The main complications include post-traumatic osteoarthritis, avascular necrosis of the femoral head, and the formation of HO. Avascular necrosis of the femoral head and HO has been identified as common post-traumatic complications of femoral head fractures and may lead to a restriction in hip function and permanent disability, and the question of surgical approach and its relationship with HO and avascular necrosis of the femoral head remains controversial. Guo et al. [33] concluded that the anterior approach is one of the risk factors of HO, and the posterior approach increases the incidence of avascular necrosis of the femoral head. Droll et al. [3] also thought the anterior approach would increase the incidence of HO, and this potential risk may be related to aggressive muscular stripping from the ilium during the approach. Epstein et al. [15] showed that the anterior approach can further damage the remaining anterior blood supply to the femoral head after a posterior hip dislocation, but anatomical and clinical studies do not support this theory [35, 34, 36]. Henle et al. [12] showed that even after a posterior dislocation, a posterior approach to the hip joint causes more additional damage to the blood supply of the femoral head than an anterior approach and increased the incidence of avascular necrosis of the femoral head; this conclusion is consistent with the findings of Stannard and his colleagues [37].
In our study, there were no statistically significant differences between the two groups in the incidence of post-traumatic osteoarthritis, HO, or avascular necrosis of the femoral head. Four (19.0%) of 21 patients treated with the modified Heuter anterior approach developed HO; the incidence of HO is less than that in patients treated with the anterior approach (42.1%) in the previous literature [33]. We think this may be related to the fact that no muscle releases were performed during the exposure. At the same time, the lack of muscle detachment can avoid further damage to the remaining blood supply to the femoral head and reduce the incidence of avascular necrosis of the femoral head.
Conclusions
Although limited by the small sample size and nonrandomized controlled trial, we can conclude that compared with the posterior Kocher-Langenbeck approach, the modified Heuter approach can effectively reduce blood loss and operative time, and fracture reduction can be accomplished under direct visualization without the detachment of muscles. The modified Heuter approach is simple, straightforward, and atraumatic with less incidence of complications and is a viable option for open reduction and internal fixation of Pipkin type I and type II femoral head fractures.
References
Birkett J (1869) Description of a dislocation of the head of the femur, complicated with its fracture: with remarks. Med Chir Trans 52:133–138
Pipkin G (1957) Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am 39-A:1027–1042
Droll KP, Broekhuyse H, O'Brien P (2007) Fracture of the femoral head. J Am Acad Orthop Surg 15:716–727
Epstein HC (1974) Posterior fracture-dislocations of the hip: long-term follow-up. J Bone Joint Surg Am 56:1103–1127
Dreinhofer KE, Schwarzkopf SR, Haas NP, Tscherne H (1996) Femur head dislocation fractures. Long-term outcome of conservative and surgical therapy. UNFALLCHIRURG 99:400–409
Tripathy SK, Sen RK, Goyal T (2011) Conservative versus surgical management of Pipkin type I fractures associated with posterior dislocation of the hip: a randomised controlled trial. Int Orthop 35:1907
Schonweiss T, Wagner S, Mayr E, Ruter A (1999) Late results after fracture of the femoral head. UNFALLCHIRURG 102:776–783
Brumback RJ, Kenzora JE, Levitt LE, Burgess AR, Poka A (1987) Fractures of the femoral head. Hip:181–206
Lang-Stevenson A, Getty CJ (1987) The Pipkin fracture-dislocation of the hip. Injury 18:264–269
Marchetti ME, Steinberg GG, Coumas JM (1996) Intermediate-term experience of Pipkin fracture-dislocations of the hip. J Orthop Trauma 10:455–461
Roeder LJ, DeLee JC (1980) Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res:121–130
Henle P, Kloen P, Siebenrock KA (2007) Femoral head injuries: which treatment strategy can be recommended? Injury 38:478–488
Mostafa MF, El-Adl W, El-Sayed MA (2014) Operative treatment of displaced Pipkin type I and II femoral head fractures. Arch Orthop Trauma Surg 134:637–644
Nast-Kolb D, Ruchholtz S, Schweiberer L (1997) Treatment of Pipkin fractures. Orthopade 26:360–367
Epstein HC, Wiss DA, Cozen L (1985) Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res:9–17
Hougaard K, Thomsen PB (1988) Traumatic posterior fracture-dislocation of the hip with fracture of the femoral head or neck, or both. J Bone Joint Surg Am 70:233–239
Davis JB (1950) Simultaneous femoral head fracture and traumatic hip dislocation. Am J Surg 80:893–895
Funsten RV, Kinser P, Frankel CJ (1938) Dashboard dislocation of the hip: a report of twenty cases of traumatic dislocation. Jbjs 20:124–132
Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST (1992) Operative management of displaced femoral head fractures: case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma 6:437–442
Kloen P, Siebenrock KA, Raaymakers ELFB, Marti RK, Ganz R (2002) Femoral head fractures revisited. Eur J Trauma 28:221–233
Leslie MP, Wolinsky JP (2010) Treatment of femoral head fractures. Tech Orthop 25:155–159
Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U (2001) Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br Vol 83:1119–1124
Paillard P (2007) Hip replacement by a minimal anterior approach. Int Orthop 31(Suppl 1):S13–S15
JUDET J, JUDET R (1950) The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br 32-B:166–173
JUDET R, JUDET J (1952) Technique and results with the acrylic femoral head prosthesis. J Bone Joint Surg Br 34-B:173–180
Light TR, Keggi KJ (1980) Anterior approach to hip arthroplasty. Clin Orthop Relat Res:255–260
Kennon R, Keggi J, Zatorski LE, Keggi KJ (2004) Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. J Bone Joint Surg Am 86-A(Suppl 2):91–97
Matta JM, Shahrdar C, Ferguson T (2005) Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res 441:115–124
Rudert M, Horas K, Hoberg M, Steinert A, Holzapfel DE, Hübner S, Holzapfel BM (2016) The Wuerzburg procedure: the tensor fasciae latae perforator is a reliable anatomical landmark to clearly identify the Hueter interval when using the minimally-invasive direct anterior approach to the hip joint. BMC Musculoskel DIS 17:57
Fahey JJ (1949) Surgical approaches to bones and joints. Surg Clin North Am 29:65–76
O’Brien RM (1955) The technic for insertion of femoral head prosthesis by the straight anterior or Hueter approach. Clin Orthop 6:22
Kurtz WJ, Vrabec GA (2009) Fixation of femoral head fractures using the modified Heuter direct anterior approach. J Orthop Trauma 23:675–680
Guo JJ, Tang N, Yang HL, Qin L, Leung KS (2010) Impact of surgical approach on postoperative heterotopic ossification and avascular necrosis in femoral head fractures: a systematic review. Int Orthop 34:319–322
Trueta J, Harrison MH (1953) The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br 35-B:442–461
Gautier E, Ganz K, Krugel N, Gill T, Ganz R (2000) Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 82:679–683
Stockenhuber N, Schweighofer F, Seibert FJ (1994) Diagnosis, therapy and prognosis of Pipkin fractures (femur head dislocation fractures). Chirurg 65:976
Stannard JP, Harris HW, Volgas DA, Alonso JE (2000) Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res (377):44–56
Thompson VP, Epstein HC (1951) Traumatic dislocation of the hip: a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am 33-A:746–778
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification[J]. J Bone Joint Surg Am 55(8):1629–1632
Acknowledgments
We wish to thank all of those who generously agreed to be interviewed for this research.
Funding
This work was supported by the Natural Science Foundation of China (81472061).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Wang, S., Li, B., Li, J. et al. Comparison of the modified Heuter approach and the Kocher-Langenbeck approach in the treatment of Pipkin type I and type II femoral head fractures. International Orthopaedics (SICOT) 43, 2613–2620 (2019). https://doi.org/10.1007/s00264-019-04301-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04301-5