Abstract
Purpose
Adjacent segment degeneration (ASDeg) and disease (ASDis) have become major concerns after fusion surgery. However, there is no definitive data or knowledge about the incidence or risk factors. The review discusses the incidence and risk factors and prevention of ASDeg and ASDis in the relevant literature.
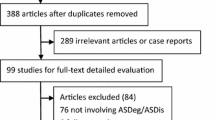
Methods
We performed a systematic review of meta-analyses, randomized control trials, and cohort studies published in English to provide evidence-based information about ASDeg and ASDis.
Results
According to a meta-analysis, the pooled incidence of ASDeg after lumbar and cervical fusion surgery was 26.6% and 32.8%, respectively. Approximately 1/4–1/3 of ASDeg progressed to ASDis. Risk factors after cervical fusion surgery were young age, pre-existing disc degeneration, short fusion segment, high T1 slope, disruption of adjacent soft tissue, and plate placement close to the adjacent disc. The risk factors of ASDeg and ASDis after lumbar fusion surgery were age, genetic factors, high body mass index, pre-existing adjacent segment degeneration, laminectomy at the adjacent level of fusion, excessive distraction of the fusion level, insufficient lumbar lordosis, multilevel fixation, floating fusion, coronal wedging of L5-S disc, pelvic tilt, and osteoporosis. Motion-preserving surgeries seem to have less risk of ASDeg and ASDis than conventional fusion surgery both in the lumbar and cervical spine.
Conclusions
The existent literature points out variables involved in ASDeg and ASDis. High evidence-level studies should provide more relevant data to guide strategies for avoiding ASDeg and ASDis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number and the rate of spinal fusion surgeries have been increasing annually [1, 2]. Recently, adjacent segment degeneration (ASDeg) has become a major concern after fusion surgery. Adjacent segment degeneration is defined as the radiographic change in the intervertebral discs adjacent to the surgically treated spinal level, regardless of the presence of symptoms [3]. Adjacent segment disease (ASDis) represents symptomatic adjacent segment degeneration, causing pain or numbness due to post-operative spinal instability or nerve compression at the same level [4]. The relationship between adjacent segment degeneration and spinal fusion surgery has been discussed in several reports [4, 5]; however, no definitive data or knowledge about the incidence or risk factors exist due to various operative methods or patients’ backgrounds. As a matter of course, the pathology of adjacent segment degeneration differs between the lumbar and the cervical spine due to the difference in their anatomical and mechanical feature. Although various new surgical strategies have been developed to avoid adjacent segment degeneration (especially for motion-preserving surgeries) [4, 6,7,8], the efficacy of those new technologies is still controversial.
This review aims to discuss the incidence and risk factors of and methods to avoid adjacent segment degeneration and disease in the lumbar and cervical spine in reference to recent literature.
Incidence
The incidence of ASDeg and ASDis after spinal fusion surgery has a great variance among previous reports. Xia et al. [9] analyzed ASDeg and ASDis by meta-analysis using 94 literature reports containing 34,716 patients who underwent spinal fusion surgery.
According to their report [9], the occurrence of ASDeg and ASDis after lumbar spinal fusion surgery ranges 5–77% and 0–27% with a pooled prevalence of 26.6% and 8.5%, respectively. On the contrary, the occurrence of ASDeg and ASDis after cervical spinal fusion surgery ranges 7–92% and 0–25% with the pooled prevalence of 32.8% and 6.3%, respectively. Table 1 shows the prevalence of ASDeg and ASDis by spinal level. The prevalence of ASDeg and ASDis was also analyzed by period from the spinal fusion surgery. The post-operative period was divided into three groups for the analysis: 0.5–two, two to five, and five to ten years. Table 2 shows the prevalence of ASDeg and ASDis in each period. Hilibrand et al. [10] reported that the ASDis after cervical anterior arthrodesis occurred at a relatively constant incidence of 2.9% per year, reaching 25.6% after ten years. Considering these data, approximately 1/4–1/3 of ASDeg is assumed to proceed to ASDis; radiographic adjacent segment degeneration is not necessarily related to symptoms after spinal fusion surgery, as shown in the literature [11,12,13].
Natural course, biomechanics, and risk factors
Adjacent segment degeneration and disease after spinal fusion surgery are considered to be multifactorial. Since the biomechanical feature is different by the levels of the spinal column, the etiology and/or risk factors are likely also different between the lumbar and cervical spine.
Lumbar spine
Natural course and non-fusion surgery
Regarding the natural course of disc degeneration, a study of whole spine magnetic resonance images (MRI) of 653 patients revealed that the grade of disc degeneration is strongly correlated with aging in all levels of the spine [14]. Age-related lumbar intervertebral disc degeneration was also reported in healthy volunteers [11, 13, 15]. According to these reports, more than half of healthy individual ≥ 60 years have degenerated discs, determined radiologically. On the contrary, the cumulative incidence of ASDis after lumbar laminectomy without fusion was reported to be 10% over four years [16], which was lower than that with fusion surgery at the same institute [17].
Biomechanics
In a biomechanical study using finite element models, fusion at the L4/5 level increased stress on L3/4 vertebral endplate and intervertebral discs on flexion/extension moment [18]. Also, a cadaveric experiment revealed the increased intradiscal pressure of the adjacent, proximal intervertebral disc to the fixed level [19, 20]. Cunningham et al. demonstrated increased L2/3 intradiscal pressure on flexion/extension stress by 45% in the cadaveric L3/4 fixation model [19].
Risk factors
Various risk factors have been proposed on the occurrence of ASDeg or ASDis and were discussed in the literature, such as aging, genetic factors, high body mass index (BMI), pre-existing adjacent segment stenosis or degeneration, laminectomy at the adjacent level of fusion, excessive distraction of the fusion level, insufficient lumbar lordosis, multilevel fixation, “floating fusion” with the lower end vertebra of the fusion at L5, coronal wedging of L5-S disc, posterior tilting of the pelvis, and osteoporosis (Table 3). Lawrence et al. [21] stated that patients older than 60 years may have an increased risk of developing ASDis in the lumbar spine. A genetic investigation revealed that single-nucleotide polymorphisms in the IL18RAP gene were associated with lower disc space height at the adjacent level, although this relationship has not been replicated [22]. Retrospective studies investigating a relationship between BMI and ASDeg demonstrated the higher incidence of ASDeg in patients with BMI ≥ 25. Pre-existing adjacent segment narrowing, degeneration of intervertebral disc, and facet joint are also risk factors of ASDis [23,24,25]. According to Yugue et al. [25], spinal canal narrowing at an adjacent segment ≥ 47% was found to be a risk factor of ASDis following lumbar fusion surgery. Additionally, laminectomy at the adjacent level of fusion increases the risk of ASDeg. Miyagi et al. [26] stated that the rate of ASDeg was significantly higher at the decompressed site adjacent to the fused level in patients with posterior lumbar interbody fusion (PLIF) compared to those without decompression. Radcliff et al. [27] also supported the finding of risk of ASDis after laminectomy of adjacent level. Kaito et al. [28] observed the relationship between the extent of disc space distraction of L4/5 disc and occurrence of ASDeg and ASDis at the L3/4 disc in patients with L4/5 PLIF. The L4/5 disc space distraction by cage insertion was 3.1 mm in the group without ASDeg, 4.4 mm in the group with ASDeg, and 6.2 mm in the group with ASDis. They concluded that the excessive distraction of the fusion level by cages was a significant risk factor of ASDeg and ASDis. Sagittal malalignment or loss of lumbar lordosis after lumbar fusion surgery was discussed by Djurasovic et al. [29] in their case-control study. Patients who required re-operation for ASDis had significantly less lordosis through the fused levels and total lumbar lordosis. The number of fusion levels can also influence the occurrence of ASDeg. The longer lever arm produced by multiple-level fusion causes more stress at the free segments [30]. The influence of floating fusion, i.e., fusion with the lower end vertebra at L5, on ASDis was investigated in a retrospective study with a large case series from a single institute by Bydon et al. [17]. In 511 cases of posterolateral instrumented lumbar arthrodesis, floating fusion cases were more likely to develop ASDeg. Moreover, coronal wedging of the L5/S disc is also a risk factor of foraminal stenosis at L5/S level after floating fusion [31]. High pelvic tilt is also a potential risk factor of ASDeg. In a retrospective study of 263 patients with transforaminal lumbar interbody fusion, logistic regression and receiver operating characteristic analyses revealed that the risk of ASD incidence was 5.1 times greater in subjects with pre-operative PT of more than 22.5% [32]. Another retrospective study demonstrated that patients with a sacral slope (SS) < 39° or PT ˃ 21° were at higher risk for ASDis, with a relative risk of 1.73 and 3.66, respectively [33]. Osteoporosis is another potential risk of ASD. In an experiment with spinal fusion in ovariectomized, osteoporotic rat model, osteoporosis evoked greater ASDeg than wild-type rats, which was prevented with the administration of alendronate [34]. A similar effect was observed by administration of parathyroid hormone (PTH) 1-34 in another experiment using rat models [35].
Cervical spine
Natural course and non-fusion surgery
Regarding the natural course of the cervical intervertebral disc, Boden et al. [36] investigated MRI of the cervical spine in 63 asymptomatic volunteers without previous history of cervical disorders. Major abnormalities in the cervical intervertebral discs were found in 14% and 28% of the subjects younger than 40 and elder than 40 years, respectively. Kretzer at al. [37] reported a cadaveric study measuring range of motion and intradiscal pressure in adjacent discs in various patterns of posterior surgeries for the cervical spine. In a study comparing C3–C6 laminectomy with/without posterior instrumented fusion, posterior instrumentation doubled both the range of motion and the intradiscal pressure of the adjacent discs.
Biomechanical studies
In a biomechanical study using a finite element model [38], C5/6 fixation caused higher stress force on C4/5 disc more than C4/5 fixation on the C5/6 disc, indicating the upper adjacent segment to the fixation site received more stress force than the lower adjacent segment. A cadaveric study also demonstrated that anterior cervical fusion caused increased intradiscal pressure in the proximal adjacent disc on flexion/extension [39]. Matsumoto et al. [40] compared disc degeneration on MRI between patients with anterior cervical fusion surgery and normal volunteers. The study demonstrated the decreased signal intensity of C4/5, increased posterior protrusion of C5/6 disc, decreased disc height, and progressed foraminal stenosis at C3/4 and C6/7 disc in fusion group; however, these changes were not necessarily symptomatic.
Risk factors
The features of risk factors of ASDeg and ASDis in cervical spine differ from those in the lumbar spine, due to the difference in anatomical structure and/or mechanical function. In the cervical spine, young age, preexisting disc degeneration, short fusion segment, high T1 slope, disruption of adjacent soft tissue, and plate placement close to the adjacent disc are proposed to be potential risk factors causing ASDeg and ASDis (Table 3). Lawrence et al. [41] reported that in people aged less than 60 years, pre-existing disc degeneration and fusion adjacent to C5–6 and/or C6–7 levels contribute to the development of ASDis. Interesting findings have been shown in the literature for the incidence of ASDeg after single-level and multiple-level cervical fusion. Ikenaga et al. [42] reported that a ten year follow-up of 31 cases after > four level cervical anterior fusion showed only one case of ASDeg, indicating that the cervical anterior multilevel fusion is not necessarily a risk factor. Hilibrand et al. [10] also demonstrated that the risk of ASDis following multilevel cervical fusion was significantly lower than that following single-level fusion. In this study, 31 out of 256 multilevel fusions and 27 out of 153 single-level fusions caused ASDis (odds ratio, 0.64; P < 0.001). Yang et al. [43] assessed the impact of T1 slope on the development of ASDis. While analyzing 90 cases with cervical disc arthroplasty (CDR), the incidence of symptomatic adjacent segment degeneration and neck pain was significantly more severe in patients with high T1 slope. Nassr et al. [44] analyzed the influence of soft tissue disruption in anterior cervical fusion surgery, finding that 15 of 87 patients with anterior cervical discectomy and fusion had incorrect needle localization, i.e., a needle was placed at the level not included in the fusion at surgery. Patients with incorrect needle localization developed more disc degeneration at the two year follow-up with an odds ratio of 3.2. They concluded that needle penetration of nucleus pulposus could facilitate disc degeneration. Plate placement close to the adjacent disc is also reported as a risk factor of ASDis. Park et al. [45] reviewed lateral radiographs of 118 patients with cervical anterior fusion with a plate and found that the adjacent disc ossification occurred more frequently in patients whose plate placement was within 5 mm of the adjacent disc. The risk factors of ASDeg and ASDis in occipitocervical fusion surgery were also discussed. In the retrospective study of 41 non-rheumatoid arthritis patients with atlantoaxial instability, Wu et al. [46] found that patients with ASDeg had less correction of O-C2 angle and C2-7 lordosis compared to those without ASDeg, and concluded that the poor correction of cervical sagittal alignment could be a risk factor in developing ASDeg and ASDis.
Strategies to avoid adjacent segment degeneration and disease
Spinal fusion surgery develops adjacent segment degeneration by concentrating a stress force in the adjacent segment, regardless of the presence of concomitant symptoms [3]. In this regards, strategies to avoid adjacent segment degeneration are discussed in this section, especially highlighting tips in conventional fusion surgery and effect of recent motion-preserving surgery in the lumbar and cervical spine.
Lumbar spine
Several tips have been proposed for conventional lumbar fusion surgery to prevent adjacent segment degeneration. Liu et al. [47] conducted a clinical research study to elucidate the effect of posterior element resection in lumbar fusion. In total, 120 patients were randomly allocated for facetectomy, hemilaminectomy, and total laminectomy on L4-5 fusion. After asix year follow-up, patients with total laminectomy developed a significantly larger number of ASDeg and ASDis cases. Imagama et al. [48] also investigated the effect of laminectomy on fusion level. A five year follow-up of 52 patients after L4-5 fusion with L4 laminectomy or L4-5 fenestration revealed that patients with fenestration developed less ASDeg. Results indicate that preservation of posterior element of the fusion site is a key factor to avoid ASDeg or ASDis after lumbar fusion surgery. Makino at al. [49] reported that minimum disc distraction using low-profile interbody cages could prevent ASDeg. In that study, the incidence of ASDeg in 41 patients with L4-5 PLIF with minimum disc distraction (12.2%) was significantly lower than that of previous study about PLIF with distracted disc space (31.8%). Treatment of osteoporosis is another tip to prevent ASDeg and ASDis. An experiment with a lumbar fusion model of ovariectomized rats demonstrated significantly more ASDeg than a control group, and the administration of alendronate significantly improved bone mass and vertebrae microstructures, increased disc height, and decreased endplate calcification area. Additionally, alendronate significantly decreased COL1, MMP13, and ADAMTS4 expression and increased COL2 and aggrecan expression in the disc matrix [34]. The same group showed that parathyroid hormone (PTH) 1-34 in the same model also prevents ASDeg by preserving disc height, microvessel density, relative area of vascular buds, endplate thickness, and relative area of endplate calcification [50]. These results suggest the use of bisphosphonates or PTH in patients with lumbar spinal fusion surgery.
Recently, motion-preserving techniques such as total disc arthroplasty have been developed and widely used under the belief that preserved segmental motion could disburse the stress on the adjacent segments. On the contrary, the adjacent segment degeneration-prevention effect of total disc arthroplasty has been controversial. Among recently published meta-analyses comparing the incidence or risk of ASDeg or ASDis between conventional lumbar fusion surgery and motion-preservation procedures, Pan et al. [51] analyzed 15 studies, including nine cohort studies and 6 randomized controlled trials (RCTs), comprising 1474 patients. Among these patients, 687 underwent fusion and 787 underwent motion-preservation procedures. The prevalence of ASDeg after long-term follow-up in lumbar fusion group (37.5%) was significantly higher than that in the non-fusion group (18.6%) with an odds ratio of 3.03. Also, the prevalence of ASDis in the fusion group (14.4%) was significantly higher than that in the motion-preserving group (5.1%) with an odds ratio of 2.81. The re-operation rate in the fusion group (7.7%) was also significantly higher than that in the motion-preserving group (1.1%) with an odds ratio of 4.82. From the viewpoint of ASDeg and ASDis risk, motion-preserving surgery appears to be superior to fusion surgery, although each procedure should consider the pros and cons in other parameters.
Cervical spine
Considering that multiple cervical anterior fusions do not increase the risk of ASDeg and ASDis compared to single-level fusion [10, 52], Basques et al. [52] concluded that well-preserved cervical alignment contributes to lower incidence of adjacent segment problems. Therefore, ACDF with well-preserved cervical lordosis could help to avoid ASDeg and ASDis. Nassr et al. [44] reported that incorrect needle placement into the disc increases the risk of ASDeg as shown in the risk factor section, indicating that preservation of adjacent soft tissue could help ACDF to avoid ASDeg and ASDis.
As total disc replacement or cervical disc arthroplasty (CDR) has been used worldwide recently, cohort studies and RCTs have reported this new technique. Among meta-analyses investigating the incidence of ASDeg and ASDis between these procedures, the largest and most recent study was conducted by Dong et al. [53]. In this analysis, 41 articles including 27 RCTs, eight retrospective cohort studies, and six prospective cohort studies were enrolled containing a total of 3959 patients with CDR and 3573 patients with ACDF. The rate of ASDeg was 60% lower in CDA compared with ACDF, with an odds ratio of 0.40. In subgroup analysis, the rate of ASDeg in single-level and 2-level CDA was 54% and 74% lower than that of ACDF, respectively. Also, the rate of ASDis was 50% lower in CDA than ACDF. The rate of reoperation for ASDis was reduced by 47% in the CDA group compared to ACDF, with an odds ratio of 0.53. Especially in patients with 24-month or longer follow-up, the re-operation rate was reduced by 69% in the CDA group (odds ratio, 0.31). Moreover, the range of motion of upper and lower adjacent disc was significantly reduced compared to ACDF. Accordingly, motion-preserving cervical surgery seems to have potential preventing ASDeg and ASDis by reducing mechanical stress to the adjacent disc. These results are consistent with Hilibrand’s study [10] stating a close correlation between the incidence of ASDis and the magnitude of motion at the adjacent disc level.
Conclusion
The aetiology, incidence, and risk factors of adjacent segment degeneration and disease in various fusion surgeries are gradually being elucidated. In particular, meta-analyses of RCT and retrospective/prospective cohort studies have formed strong evidence. However, owing to the multifactorial feature of adjacent segment degeneration and disease, a variety of surgical options is challenging to give consensus on pathology or risk factors. The risk factors of adjacent segment degeneration and disease were different between the lumbar and cervical spine because of the difference in their mechanical and functional feature. Strategies to avoid adjacent segment problems in the lumbar spine include minimal disc space distraction for cage placement and preservation of adjacent posterior elements. Additionally, motion-preserving technologies such as total disc arthroplasty have been widely used in both lumbar and cervical spine. Studies have determined a potential to decrease adjacent segment problems by diverging stress forces on the adjacent segments. Further studies generating high evidence-level need to provide more precise and concrete data to inform strategies avoiding ASDeg and ASDis in spinal surgeries.
References
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303(13):1259–1265
Kotwal S, Pumberger M, Hughes A, Girardi F (2011) Degenerative scoliosis: a review. HSS J 7(3):257–264
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6 Suppl):190S–194S
Harrop JS, Youssef JA, Maltenfort M, Vorwald P, Jabbour P, Bono CM, Goldfarb N, Vaccaro AR, Hilibrand AS (2008) Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 33(15):1701–1707
Saavedra-Pozo FM, Deusdara RA, Benzel EC (2014) Adjacent segment disease perspective and review of the literature. Ochsner J 14(1):78–83
Anakwenze OA, Auerbach JD, Milby AH, Lonner BS, Balderston RA (2009) Sagittal cervical alignment after cervical disc arthroplasty and anterior cervical discectomy and fusion: results of a prospective, randomized, controlled trial. Spine (Phila Pa 1976) 34(19):2001–2007
Cho SK, Riew KD (2013) Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg 21(1):3–11
Kelly MP, Mok JM, Frisch RF, Tay BK (2011) Adjacent segment motion after anterior cervical discectomy and fusion versus Prodisc-c cervical total disk arthroplasty: analysis from a randomized, controlled trial. Spine (Phila Pa 1976) 36(15):1171–1179
Xia XP, Chen HL, Cheng HB (2013) Prevalence of adjacent segment degeneration after spine surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 38(7):597–608
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M (1995) 1995 Volvo award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine (Phila Pa 1976) 20(24):2613–2625
Borenstein DG, O’Mara JW Jr, Boden SD, Lauerman WC, Jacobson A, Platenberg C, Schellinger D, Wiesel SW (2001) The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects : a seven-year follow-up study. J Bone Joint Surg Am 83-A(9):1306–1311
Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331(2):69–73
Oh CH, Yoon SH (2017) Whole spine disc degeneration survey according to the ages and sex using Pfirrmann disc degeneration grades. Korean J Spine 14(4):148–154
Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 72(3):403–408
Bydon M, Macki M, De la Garza-Ramos R, McGovern K, Sciubba DM, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A (2016) Incidence of adjacent segment disease requiring reoperation after lumbar laminectomy without fusion: a study of 398 patients. Neurosurgery 78(2):192–199
Bydon M, Xu R, Santiago-Dieppa D, Macki M, Sciubba DM, Wolinsky JP, Bydon A, Gokaslan ZL, Witham TF (2014) Adjacent-segment disease in 511 cases of posterolateral instrumented lumbar arthrodesis: floating fusion versus distal construct including the sacrum. J Neurosurg Spine 20(4):380–386
Chosa E, Goto K, Totoribe K, Tajima N (2004) Analysis of the effect of lumbar spine fusion on the superior adjacent intervertebral disk in the presence of disk degeneration, using the three-dimensional finite element method. J Spinal Disord Tech 17(2):134–139
Cunningham BW, Kotani Y, McNulty PS, Cappuccino A, McAfee PC (1997) The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure: an in vitro biomechanical analysis. Spine (Phila Pa 1976) 22(22):2655–2663
Weinhoffer SL, Guyer RD, Herbert M, Griffith SL (1995) Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976) 20(5):526–531
Lawrence BD, Wang J, Arnold PM, Hermsmeyer J, Norvell DC, Brodke DS (2012) Predicting the risk of adjacent segment pathology after lumbar fusion: a systematic review. Spine (Phila Pa 1976) 37(22 Suppl):S123–S132
Omair A, Mannion AF, Holden M, Leivseth G, Fairbank J, Hagg O, Fritzell P, Brox JI (2016) Age and pro-inflammatory gene polymorphisms influence adjacent segment disc degeneration more than fusion does in patients treated for chronic low back pain. Eur Spine J 25(1):2–13
Kim JY, Ryu DS, Paik HK, Ahn SS, Kang MS, Kim KH, Park JY, Chin DK, Kim KS, Cho YE, Kuh SU (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16(7):867–875
Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, Lee MY (2009) Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J 18(11):1637–1643
Yugue I, Okada S, Masuda M, Ueta T, Maeda T, Shiba K (2016) Risk factors for adjacent segment pathology requiring additional surgery after single-level spinal fusion: impact of pre-existing spinal stenosis demonstrated by preoperative myelography. Eur Spine J 25(5):1542–1549
Miyagi M, Ikeda O, Ohtori S, Tsuneizumi Y, Someya Y, Shibayama M, Ogawa Y, Inoue G, Orita S, Eguchi Y, Kamoda H, Arai G, Ishikawa T, Aoki Y, Toyone T, Ooi T, Takahashi K (2013) Additional decompression at adjacent segments leads to adjacent segment degeneration after PLIF. Eur Spine J 22(8):1877–1883
Radcliff KE, Kepler CK, Jakoi A, Sidhu GS, Rihn J, Vaccaro AR, Albert TJ, Hilibrand AS (2013) Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J 13(10):1339–1349
Kaito T, Hosono N, Mukai Y, Makino T, Fuji T, Yonenobu K (2010) Induction of early degeneration of the adjacent segment after posterior lumbar interbody fusion by excessive distraction of lumbar disc space. J Neurosurg Spine 12(6):671–679
Djurasovic MO, Carreon LY, Glassman SD, Dimar JR 2nd, Puno RM, Johnson JR (2008) Sagittal alignment as a risk factor for adjacent level degeneration: a case-control study. Orthopedics 31(6):546
Nagata H, Schendel MJ, Transfeldt EE, Lewis JL (1993) The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976) 18(16):2471–2479
Orita S, Yamagata M, Ikeda Y, Nakajima F, Aoki Y, Nakamura J, Takahashi K, Suzuki T, Ohtori S (2015) Retrospective exploration of risk factors for L5 radiculopathy following lumbar floating fusion surgery. J Orthop Surg Res 10:164
Yamasaki K, Hoshino M, Omori K, Igarashi H, Nemoto Y, Tsuruta T, Matsumoto K, Iriuchishima T, Ajiro Y, Matsuzaki H (2017) Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 42(2):E86–E92
Di Martino A, Quattrocchi CC, Scarciolla L, Papapietro N, Beomonte Zobel B, Denaro V (2014) Estimating the risk for symptomatic adjacent segment degeneration after lumbar fusion: analysis from a cohort of patients undergoing revision surgery. Eur Spine J 23(Suppl 6):693–698
Zhou Z, Tian FM, Wang P, Gou Y, Zhang H, Song HP, Wang WY, Zhang L (2015) Alendronate prevents intervertebral disc degeneration adjacent to a lumbar fusion in ovariectomized rats. Spine (Phila Pa 1976) 40(20):E1073–E1083
Luo Y, Li SY, Tian FM, Song HP, Zhang YZ, Zhang L (2018) Effects of human parathyroid hormone 1-34 on bone loss and lumbar intervertebral disc degeneration in ovariectomized rats. Int Orthop 42(5):1183–1190
Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S (1990) Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 72(8):1178–1184
Kretzer RM, Hsu W, Hu N, Umekoji H, Jallo GI, McAfee PC, Tortolani PJ, Cunningham BW (2012) Adjacent-level range of motion and intradiscal pressure after posterior cervical decompression and fixation: an in vitro human cadaveric model. Spine (Phila Pa 1976) 37(13):E778–E785
Maiman DJ, Kumaresan S, Yoganandan N, Pintar FA (1999) Biomechanical effect of anterior cervical spine fusion on adjacent segments. Biomed Mater Eng 9(1):27–38
Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J (2007) Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine 7(1):33–39
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami A, Ikegami T, Takahata T, Hashimoto T (2010) Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 35(1):36–43
Lawrence BD, Hilibrand AS, Brodt ED, Dettori JR, Brodke DS (2012) Predicting the risk of adjacent segment pathology in the cervical spine: a systematic review. Spine (Phila Pa 1976) 37(22 Suppl):S52–S64
Ikenaga M, Shikata J, Tanaka C (2006) Long-term results over 10 years of anterior corpectomy and fusion for multilevel cervical myelopathy. Spine (Phila Pa 1976) 31(14):1568–1574 discussion 1575
Yang P, Li Y, Li J, Shen Y (2017) Impact of T1 slope on surgical and adjacent segment degeneration after Bryan cervical disc arthroplasty. Ther Clin Risk Manag 13:1119–1125
Nassr A, Lee JY, Bashir RS, Rihn JA, Eck JC, Kang JD, Lim MR (2009) Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration? Spine (Phila Pa 1976) 34(2):189–192
Park JB, Cho YS, Riew KD (2005) Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 87(3):558–563
Wu X, Qi Y, Tan M, Yi P, Yang F, Tang X, Hao Q (2018) Incidence and risk factors for adjacent segment degeneration following occipitoaxial fusion for atlantoaxial instability in non-rheumatoid arthritis. Arch Orthop Trauma Surg 138(7):921–927
Liu H, Wu W, Li Y, Liu J, Yang K, Chen Y (2013) Protective effects of preserving the posterior complex on the development of adjacent-segment degeneration after lumbar fusion: clinical article. J Neurosurg Spine 19(2):201–206
Imagama S, Kawakami N, Matsubara Y, Tsuji T, Ohara T, Katayama Y, Ishiguro N, Kanemura T (2016) Radiographic adjacent segment degeneration at 5 years after L4/5 posterior lumbar interbody fusion with pedicle screw instrumentation: evaluation by computed tomography and annual screening with magnetic resonance imaging. Clin Spine Surg 29(9):E442–E451
Makino T, Honda H, Fujiwara H, Yoshikawa H, Yonenobu K, Kaito T (2018) Low incidence of adjacent segment disease after posterior lumbar interbody fusion with minimum disc distraction: a preliminary report. Medicine (Baltimore) 97(2):e9631
Zhou Z, Tian FM, Gou Y, Wang P, Zhang H, Song HP, Shen Y, Zhang YZ, Zhang L (2016) Enhancement of lumbar fusion and alleviation of adjacent segment disc degeneration by intermittent PTH(1-34) in ovariectomized rats. J Bone Miner Res 31(4):828–838
Pan A, Hai Y, Yang J, Zhou L, Chen X, Guo H (2016) Adjacent segment degeneration after lumbar spinal fusion compared with motion-preservation procedures: a meta-analysis. Eur Spine J 25(5):1522–1532
Basques BA, Louie PK, Mormol J, Khan JM, Movassaghi K, Paul JC, Varthi A, Goldberg EJ, An HS (2018) Multi- versus single-level anterior cervical discectomy and fusion: comparing sagittal alignment, early adjacent segment degeneration, and clinical outcomes. Eur Spine J 27(11):2745–2753
Dong L, Wang D, Chen X, Liu T, Xu Z, Tan M, Hao D (2018) A comprehensive meta-analysis of the adjacent segment parameters in cervical disk arthroplasty versus anterior cervical discectomy and fusion. Clin Spine Surg 31(4):162–173
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hashimoto, K., Aizawa, T., Kanno, H. et al. Adjacent segment degeneration after fusion spinal surgery—a systematic review. International Orthopaedics (SICOT) 43, 987–993 (2019). https://doi.org/10.1007/s00264-018-4241-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4241-z