Abstract
Introduction
In last three decades, total hip replacement in young patients became an habitual procedure. Principles of bone preservation are pushing many surgeons to implant conservative femoral components in patient younger than 65 years. Despite an overall good survivorship and clinical outcomes of conservative implants, failed cases are reported and the need to revise a conservative femoral component became an occasional procedure (with high prevalence of failed resurfacing implants).
Methods
During conservative femoral component revisions, we analyzed proximal bone stock preservation, considering the type of original component removed, aetiology of failure, timing of revision, and femoral explantation technique.
Results
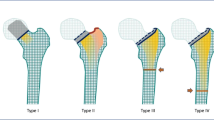
We identified four patterns of proximal femoral changes (types I–IV). We suggest, for each of them, a revision strategy directed toward a “conservative revision procedure” using conservative or primary component. Out of our 21 cases, none underwent further revision due to mechanical failure (follow-up ranging from 6 to 152 months, mean 54 months). We had two cases of re-operation: one for early septic loosening and one for prosthetic modular neck fracture.
Conclusions
If literature offers well-established guidelines to femoral revision of conventional stems, there is, on the other hand, a lack of data about revision strategies in presence of failed conservative implants. Although the mean follow-up of our procedures is still too short (4.5 years) to give final conclusions, we would leave a message: a conservative hip arthroplasty is not a “one time” opportunity for young and active people. A “conservative revision” is a valid option for at least a part of them, when an early failure of primary procedure occurred.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Principles of bone preservation and biomechanical restoring have pushed a non-neglectable number of hip reconstruction surgeons to implant conservative femoral components, such as resurfacing hip, neck retaining implant, or metaphyseal bone preserving stems.
A recent systematic review on the available evidence published before 2002 performed by Wyness [1] has detected a revision rate included between 0 and 14.3% for resurfacing implants: majority of revision surgery was due to fractures (56%), followed by loosening (19%), infection (11%), avascular necrosis (11%), and dislocation (3%).
Neck retaining conservative stems show a high percentage of excellent and good clinic-radiographic results (97%) in a 25-year experience on 943 implants [2]. Bone stock preserving implants show, at mid-term follow-up actually available in literature [3, 4], a survival rate without aseptic loosening ranging from 98.2 to 97.5%. Periprosthetic femoral fractures seem to be the main reason for re-operation after a short-stem hip arthroplasty, as observed in a large multicentric analysis evaluating 1089 hips [5]. This finding shows a different importance of this complication compared to conventional stems [6], where periprosthetic fractures represent the fourth most common cause for hip revision [7].
Despite an overall good survivorship and clinical outcomes, failed case reported (related to an increasing volume of primary conservative arthroplasty) is making the revision of a conservative femoral component a non-occasional procedure.
In our practice using different conservative hip solutions (over 600 implants) since 1999, we have performed several revision procedures for conservative implants, facing variable patterns of changes in proximal femoral structure, bone quality and, consequently, different needs during femoral stem substitution.
If literature offers well-established guidelines to femoral revision of conventional stems, based on metaphyseal and diaphyseal femoral bone defects [8], there is, on the other hand, a lack of data about revision strategies in presence of failed conservative implants in the young and active population.
However, in our opinion, even revision surgery should offer these patients a second conservative chance (where it is possible): in particular in early revisions, when criteria that made a patient suitable for a non-conventional primary stem may still be present at the time of revision (young age, good bone stock) and then we may think to a “conservative revision”.
This paper reports an analysis of femoral changes observed during revision procedures of conservative components, with the aim of proposing a practical classification to select reconstructive options (supported by our own experience).
A peculiarity of conservative femoral component failure is the presence of a variable proximal bone stock preservation (cervical or metaphyseal), able to accept both a conventional or conservative primary stem: it mainly depends on the type of original component removed, aetiology of failure, and timing of revision.
Methods
Twenty-one consecutive revision procedures involving conservative hip arthroplasty have been performed between October 2005 and February 2018.
We removed eight resurfacing hip femoral implants (5 ASR De Puy J&J, Warsaw-IN, 1 BHR Smith Nephew Orthopaedics, Memphis TN, 1 MRS Lima Lto, Villanova S. Daniele UD, Italy, 1 ReCup Biomet Warsaw-IN), one CFP stem (Waldemar Link Hamburg, AG), four Mayo stems (Zimmer, Warsaw, IN), four SMF Stems (Smith &Nephew London, UK), four Metha stems (BBraun, Melsungen AG) in 21 patients, with a mean follow-up of 13.58 months (range 3–48 months, SD13,54) after primary hip replacement.
One patient, initially revised for resurfacing failure with a Mayo Stem, has undergone a second revision procedure for septic loosening with a primary conventional stem (Platform, Smith & Nephew).
One patient, initially revised for resurfacing failure with a Metha stem, has undergone a second revision procedure for prosthetic neck fracture with SMF stem.
Proximal femoral deficiency (PFD) was classified following a closed scheme, where it is mandatory to sequentially answer the questions:
-
QUESTION 1: Medial neck preservation > 1.5 cm?
-
QUESTION 2: Lateral neck and trochanteric fossa preserved?
-
QUESTION 3: Metaphyseal cancellous bone fully supportive?
-
QUESTION 4: Extent of diaphyseal bone violation less than 2 cm?
We can summarize PFD as follows (see Table 1):
PFD type I:
-
QUESTION 1: YES
-
QUESTION 2: YES
-
QUESTION 3: YES
-
QUESTION 4: YES
A femur with a type I defect shows an almost intact cortical femoral neck, corresponding or just below the neck-head junction, with a very limited amount of cancellous bone lost (Fig. 1). This type of deficiency can be observed in early aseptic loosening of resurfacing arthroplasty and in a peculiar pattern of failure of the same prosthetic design: a fracture at the head-neck junction, often hidden by the resurfacing component and evolved in fibrous non-union (Fig. 2).
We have observed and published in 2007 [9] a case report about an unnoticed sub-capital fracture under a resurfacing arthroplasty, evolved in non-union and revised after 11 months to a neck retaining implant [10].
PFD type II:
-
QUESTION 1: NO
-
QUESTION 2: YES
-
QUESTION 3: YES
-
QUESTION 4: YES
A femur with a type II defect presents a neck preservation variable but at least the 1.5 cm of medial neck and trochanteric fossa are intact (with proximal cancellous bone, underneath the fossa itself, still supportive in Gruen [11] zone 1).
A such, defect is usually observed in some trans-cervical fracture below a resurfacing arthroplasty (Fig. 3), caused by blunt trauma of the hip or favoured by a wrong positioning of the component (varus orientation, notching) [12, 13], or in resurfacing implants failed with neck reabsorption.
Again, it may be detected in early failure of neck preserving implants, like was CFP and Metha (in the latter example, a specific indication to revision was prosthetic modular neck fracture in well-fixed implant, see Fig. 4). A late failure of same components may present an involution of bone in Gruen zone 1 after a stress-shielding effect, and then, cancellous bone in the same area may be not supportive.
PFD type III:
-
QUESTION 1: NO
-
QUESTION 2: NO
-
QUESTION 3: NO
-
QUESTION 4: YES
A femur with a type III defect is defined by a cortical neck preservation < 1.5 and, most important, trochanteric fossa with surrounding bone appears to be violated (by primary implant technique, after loosening has occurred or during femoral extraction of a well-fixed component).
This type of defect is principally observed in late aseptic loosening of cementless neck retaining conservative implants (CFP or similar) or aseptic loosening of metaphyseal bone stock retaining stem, such as the SMF stem (Fig. 5).
This defect is partially comparable to Paproski type I femoral defect for conventional stems, but with a very limited femoral canal violation (being the stems involved shorter than a conventional stem).
PFD type IV:
-
QUESTION 1: NO
-
QUESTION 2: NO
-
QUESTION 3: NO
-
QUESTION 4: NO
A femur with a type IV defect shows a deficiency comparable to Paproski type I defect, with involvement of significant tract of diaphyseal spongy bone, where cortical diaphyseal bone is usually intact: this defect is usually met in late or septic loosening of metaphyseal bone stock retaining stem, such as Mayo stem (Fig. 6), with considerable subsidence of the stem.
On the basis of the classification described above, we suggest the following revision strategies:
PFD type I defects
Virtually, every conservative hip stem can be implanted, except resurfacing or mid-head resection implant. This wide range of revision options is allowed by a supportive femoral neck, both in cortical and cancellous bone. We performed a new primary hips with a neck retaining implant (CFP stem and metha stem) (Fig. 7).
PFD type II defects
The choice of implant may vary on the basis of fracture level, but short metaphyseal stem seems to be more reliable for a conservative revision: an intact trocantheric fossa means that most of the metaphyseal cancellous bone can still be supportive; components that require only a partial–medial–neck retention (while lateral neck cortex is generally opened with a box osteotome) appear to be particularly suitable in this type of defect. We usually selected a short stem with a generous proximal fill and fit, and a scratch fit enhanced by porous coating (i.e., SMF) that in proximal femur seems to be more reliable than HA-coating.
However, in the presence of significant stress-shielding (frequently observed in some short or neck-retaining design such as Mayo Stem and Metha Stem) in zone 1 of Gruen, we consider metaphyseal bone in proximal lateral femur not supportive and then defect should be defined as type III.
Type III defects
The rate of neck preservation is comparable to a conventional osteotomy, metaphyseal cancellous bone is only partially lost, and a very limited femoral canal violation by the primary short stem is usually detected: a conventional primary stem is affordable as revision option, with few restriction in terms of design (proximal fit with distal taper or proximal plus distal fit) and no preference in terms of surface finishing or coating (textured or HA coated).
In early failure of a metaphyseal short stem, where implant removal did not require extensive proximal bone loss, or loosening of a severely undersized standard stem, a revision with a second short stem (usually a little over-sized compared to primary hip) may still be an option.
The use of a straight stems, in any case, may have some advantages compared to anatomic components, being primary stability less influenced by proximal fill: impaction grafting is then not usually needed.
Type IV defects
This situation reaches the limit possible for a conservative revision: the extensive cancellous proximal bone loss suggests that surgeons use a conventional straight stem (able to fit proximal and distal cortex) in conjunction with endomedullary impaction grafting (Fig. 8) or decline the conservative strategies, in favour of a proximally coated, noncemented implant with diaphyseal fixation (or distal fixation with an extensively porous coated implant), as usually suggested by conventional strategies. Regarding this point, clinical outcomes of intramedullary cancellous impaction grafting alone or in combination with cortical allografts showed no significant differences [14]. Fully hydroxyapatite conventional stems provided reliable results as revision component up to 27 years of follow-up, improving results of cemented or proximally coated stems [15].
This new proposal of classification has been validated for intra-observer and inter-observer reproducibility.
A group of 25 X-rays (our 21 primary failed hips, our two failed conservative revision, 2 cases from other institutions) have been electronically sent to five orthopaedic surgeons experienced in total hip replacement and five orthopaedic surgeons that only occasionally perform primary or revision hip (together with a brief explanation of type I to IV defects and classification scheme).
Same group of radiograms, set in a different order, was sent to the same assessors two weeks later.
Results were subjected to weighted kappa statistical analysis.
Results
Kappa values for inter-observer agreement were 0.69 after first evaluation and 0.71 after second evaluation for experienced reconstructive surgeons. Kappa values were 0.59 after first evaluation and 0.61 after second evaluation for occasional reconstructive surgeons.
Intra-observer agreement was 0.79 for experienced reconstructive surgeons and 0.63 for occasional reconstructive surgeons.
Clinical outcomes of our conservative revisions showed a survivorship of 90.47% (mean follow-up 54 months, range 6–152 months). Harris hip score raised from a pre-operative mean value of 51.76 to 92.86.
We had two cases undergone a second procedure (one for septic loosening, one for prosthetic neck fracture).
Actually, no further patient is scheduled for further re-operation and no clinical or radiographic signs of femoral loosening have been detected.
Discussion
Revision with primary stem is not a recent acquisition, as efficiently described by Cavagnaro et al. in 2018 [16] in their systematic review where specifically focused studies were detected from 2000 to 2016. Then, escalation of invasivity is not the unique strategy for femoral revision.
As described above, in revision settings after a conservative implant failure, we may have a limited bone defect, still suitable for a conservative bone preserving stem, pushing the concept of revision with primary stem further, to conservative revision.
Actually, there is a lack of references about pre-operative bone defect estimation after a conservative femoral component failure. This new classification tries to give the first step to understand and plan effectively a “conservative revision”.
Even if it is in an embryonal phase, this classification shows a “Good” inter and intra-observer reproducibility [17], comparable to conventional classifications [18, 19], in particular for experienced reconstructive surgeons.
The stepwise procedure of question answering has been introduced after a preliminary evaluation of inter-observer reproducibility (not included in the present study), because of the confusion in which aspect would be considered more important between neck and metaphyseal bone preservation. Confusion was, as expected, more evident in preliminary answers by occasional reconstructive hip surgeons.
Under a clinical point of view, limited defect is usually related to early loosening both of resurfacing or short femoral components (defects I and II), while in defects type III and IV, a standard primary stem may give a more reliable stability (with or without impaction grafting).
Limited to neck preserving implants and short metaphyseal stems, an endofemoral extraction of failed stem is mandatory for further steps in conservative revision strategy, whereas a proximal femoral osteotomy would be an exclusion criteria.
Obviously, any deviation from a properly defined supportive proximal femur bone stock, pre-operative or intra-operative after stem extraction, should suggest the choice of a conventional revision option, on the basis of the guidelines widely accepted.
On our routine, an early or mid-term failure in young patients suggests a revision strategy as much conservative as possible, if the indications—related to their young age—are not significantly modified.
A large experience with conservative hip solutions as primary procedures is vital, to face a revision with a solid background on conservative hip arthroplasty techniques and a clear understanding of needs in terms of femoral support for each stem.
In our experience, a proper pre-operative planning may lead to successful “conservative revision procedures”.
Out of our 21 cases, none underwent further revision due to aseptic loosening (follow-up ranging from 6 to 152 months). We had only one case of re-operation due to early septic loosening: a Mayo stem implanted after resurfacing mechanical failure for fracture, then revised with a two-step procedure (antibiotic spacer followed by conventional primary stem—Platform, Smith &Nephew London, UK—and proximal bone graft).
We had a further case revised for modular neck failure (fracture): a Metha (BBraun, Melsungen AG) modular stem was revised to a Monolithic SMF stem (Smith &Nephew London, UK) four years after implantation.
Follow-up of some of our procedures exceed ten years of follow-up giving a time-tested reliability: a conservative hip arthroplasty then is not a “one shot” opportunity for young and active people. A “conservative revision” is a valid option for at least a part of them, who has experienced an early failure of primary procedure.
Aseptic loosening and periprosthetic fracture (the latter limited to resurfacing) are typical situation suitable for revision of conservative femoral components, while carefully selected cases of early septic loosening of a short stem (that we usually manage with a two-staged procedure) may be revised again with a short stem: we had one case in our experience, with re-implantation of the same design (SMF, Smith&Nephew, London, UK) one size larger, after antibiotic spacer removal in a 58-year-old male. It was an early septic loosening; infection was initially treated— four weeks after primary procedure—with soft tissue debridment and six weeks later with endofemoral explantation and spacer. Antibiotic remains in situ for three months before final re-implantation.
Type IV defects represent a group of cases in which a conservative revision may represent a time/resources expensive procedure, and a careful selection should be performed to avoid an early second revision.
Anyway, in revision, surgery pre-operative bone loss may be underestimated and intra-operative findings may be worse than expected (in particular if stem extraction is challenging). Vital is to prepare revision surgery with dedicated instrumentation to simplify revision procedure and avoid undesired extension of operative time and intra-operative bone loss, as well as established for conventional straight stems [20].
Unfortunately, conservative stems allow only a little margin in over-sizing and sub-optimal positioning: then, is mandatory to be prepared with a conventional or revision stem, in case of quitting conservative revision previously planned.
Usually, we applied a logic of stepwise progression: resurfacing-neck retaining stem-metaphyseal short stem-standard stem.
However, in some selected cases, a revision with same category of conservative stem (in our experience, Neck Retaining CFP revised with Neck Retaining Nanos) would be possible, and in very selected ones, even a de-escalation is not impossible, if for any reason a standard femoral component was significantly under-sized, and a short stem with metaphyseal anchorage can achieve a reliable stability in proximal femur despite the level of canal violation. Following this principle, we revised a severely undersized Corail Stem (De Puy, Warsaw, IN) using a SMF stem and a McKee Farrar Stem (with a very thin layer of cement around the implant, easily removed) with a slightly over-sized Nanos Stem.
Being this study based on a retrospective evaluation of our conservative revisions, a further step will be to prospectively compare x-ray classification with intra-operative findings, to validate its ability to predict revision complexity.
References
Wyness L, Vale L, McCormack K, Grant A, Brazzelli M (2004) The effectiveness of metal on metal hip resurfacing: a systematic review of the available evidence published before 2002. BMC Health Serv Res 4:39
Pipino F, Keller A (2006) Tissue-sparing surgery: 25 years’ experience with femoral neck preserving hip arthroplasty. J Orthop Traumatol 7(1):36–41
Morrey BF, Adams RA, Kessler M (2000) A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br 82-B(7):952–958
Falez F, Casella F, Panegrossi G, Favetti F, Barresi C (2008) Perspectives of metaphyseal conservative stems. J Orthopaed Traumatol 9(1):49–54
Kim SM, HAN SB, Rhyu KH, Yoo JJ, Oh KJ, Yoo JH, Lee KJ, Lim SJ (2018) Periprosthetic femoral fracture as cause of early revision after short stem hip arthroplasty- a multicentric analysis. Int Orthop 42(9):2069–2076
Abdel MP, Cottino U, Mabry TM (2015) Management of periprosthetic femoral fractures following total hip arthroplasty: a review. Int Orthop 39(10):2005–2010
Amenabar T, Rahman WA, Avhad VV, Vera R, Gross AE, Kuzyk PR (2015) Vancouver type B2 and B3 periprosthetic fractures treated with revision total hip arthroplasty. Int Orthop 39(10):1927–1932
Paprosky WG, Burnett RS (2002) Assessment and classification of bone stock deficiency in revision total hip arthroplasty. Am J Orthop 31(8):459–464
Falez F, Casella F, La Cava F, Favetti F (2007) Nonunion in an unnoticed neck fracture in resurfacing total hip arthroplasty – case report. Hip International 17(13):179–182
Morlock MM, Bishop N, Ruther W, Delling G, Hahn M (2006) Biomechanical, morphological, and histological analysis of early failures in hip resurfacing arthroplasty. Proc Inst Mech Eng H 220(2):333–344
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
Amstuz HC, Campbell PA, Le Duff MJ (2004) Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg 86A(9):1874–1877
Indelli PF, Vail TP, Dominguez D, Pickering T (2005) Resurfacing hip replacement: surgical technique and clinical results with minimum 1-year follow-up. Paper presented at 90th nation congress of Italian Orthopaedic and Traumatologic Society 9-13th of October 2005
Li D, Hu Q, Kang P, Yang J, Zhou Z, Shen B, Pei F (2018) Reconstructed the bone stock after femoral bone loss in Vancouver B3 periprosthetic femoral fractures using cortical strut allograft and impacted cancellous allograft. Int Orthop. https://doi.org/10.1007/s00264-018-3997-5
Reikeras O (2017) Femoral revision surgery using a fully hydroxyapatite-coated stem: a cohort study of twenty-two to twenty-seven years. Int Orthop 41(2):271–275
Cavagnaro L, Formica M, Basso M, Zanirato A, Divano S, Felli L (2018) Femoral revision with primary Cementless stem: a systemtic review of the literature. Muscoloskelet Surg 102(1):1–9
Canovas F, Putman S, Girard J, Roche O, Bonnomet F, Le Beguec P (2018) Global radiological score for cementless revision stem. Int Orthop 42(5):1007–1013
Rayan F, Dodd M, Haddad FS (2008) European validation of the Vancouver classification of periprosthetic proximal femoral fractures. J Bone Joint Surg Br 90B(12):1576–1579
Yu R, Hofstaetter JC, Sullivan T, Costi K, Howie DW, Solomon LB (2013) Validity and reliability of the Paprosky acetabular defect classification. Clin Orthop Relat Res 471(7):2844–2847
Affatato S, Comitini S, Fosco M, Toni A, Tigani D (2016) Radiological identification of Zweimuller-type femoral stem prosthesis in revision cases. Int Ortop 40(11):2261–2269
Author information
Authors and Affiliations
Corresponding author
Additional information
LEVEL OF EVIDENCE: III
Rights and permissions
About this article
Cite this article
Casella, F., Favetti, F., Panegrossi, G. et al. A new classification for proximal femur bone defects in conservative hip arthroplasty revisions. International Orthopaedics (SICOT) 43, 63–70 (2019). https://doi.org/10.1007/s00264-018-4233-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4233-z