Abstract
Purpose
To investigate the use of anterior hip ultrasound (van Douveren’s method)-assisted Pavlik harness in developmental dysplasia of the hip (DDH).
Methods
Weekly anterior hip ultrasound scanning was performed in children with fixed Pavlik harness to detect whether hip reduction was achieved with the help of harness (the superior ramus of the pubis, the acetabulum, the femoral head, and the femoral neck being depicted in one plane indicated concentric reduction of the hip), and the stability of the reduction was checked by ultrasonography.
Results
A total of 39 child patients and 51 dysplastic hips were successfully detected by anterior ultrasound, and stable reduction was achieved in 37 hips (15 Graf type D and 22 type III) right after the help of Pavlik harness, in seven hips (6 type III and 1 type IV) two weeks after the help of Pavlik harness; the remaining seven hips (2 type III and 5 type IV) failed to reach stable reduction after two weeks.
Conclusion
The anterior hip ultrasound (van Douveren’s method) can be used to detect the reduction and stability of hip after Pavlik harness treatment in children with DDH. The majority of Graf type D and III hips can achieve a stable concentric reduction right after the help of Pavlik harness, while severely dislocated type IV hips have a low success rate for harness treatment, and abandonment of harness therapy should be considered in early stage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH), as the most common type of limb deformity in newborns and young children, is currently a hotspot in orthopaedics and imaging department, including acetabular dysplasia, subluxation of the hip, and hip dislocation with proximal femoral displacement [1]. At present, Graf lateral ultrasound scanning is widely used for initial screening of suspected DDH newborns and for follow-up [2, 3]. Nevertheless, during the Pavlik harness treatment, concentric reduction of harness-fixed femoral head cannot be accurately and real-timely detected by the Graf method because of the fixed hip flexion-abduction position [4]. In 2003, Professor van Douveren proposed that the ultrasound probe could be positioned in the groin to confirm the position of the femoral head after closed or open reduction surgery in children with DDH [5].
This paper aims to investigate the detection and follow-up value of anterior hip ultrasound-assisted Pavlik harness in children with DDH.
Materials and methods
General data
This study was approved by the Ethical Committee of the Shanghai Children’s Medical Center, Shanghai Jiao Tong University School of Medicine. The informed consents were obtained from all parents of child patients. A group of children with DDH treated by Pavlik harness from January 2015 to December 2016 was included in this study. Inclusion criteria include age less than six months at initial diagnosis; hip dislocation of Graf type D, type III, or type IV suggested by initial diagnosis (hip ultrasonography); and no prior intervention treatment. Exclusion criteria include neurogenic, pathological, or syndrome hip dislocation; with complications of other congenital malformations; and follow-up less than 12 months.
Anterior inguinal ultrasonography
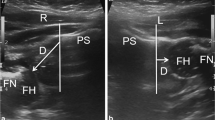
The GE Logiq 9 diasonograph with 8C micro-convex probe and centre frequency of 7 MHz was used. Methods of ultrasonography include (1) no sedatives were used during the examination with unloosing of Pavlik harness and sustaining position-fixation; (2) child patients on the examining table were in the supine position with the exposure of groin; (3) excessive or maximally abduction of the hip should be avoided, maintaining a posture of “safety angle” with the fixation of Pavlik harness [6]; (4) in cross-section scanning, the probe started from the pubic symphysis to both sides of the rami of the ischia in order to observe the right and left hip, respectively; (5) the probe was placed on the superior ramus of the pubis in front of the hip, and the centre point was perpendicular to the femoral head. The scanning direction was from front to back, and the probe was always perpendicular to the vertical axis of the trunk during the scanning to avoid excessive head-to-tail or side-to-side tilt (Fig. 1). The anatomical position of the femoral head and femoral neck was confirmed and they were made to be in one plane with the superior ramus of the pubis and the acetabulum; (6) static observation of the relative position and abnormal echo between the femoral head and acetabulum was performed with photograph records stored in the picture archiving and communication system (PACS); and (7) the position of the femoral head in the acetabulum with hip flexion-abduction and the stability of the femoral head with fixed Pavlik harness were dynamically examined, and the video records were stored in the PACS.
Diagnostic criteria of anterior inguinal ultrasonography: If the femoral head stably relied on the surface of the acetabular cartilage with a normal position and concentric reduction, the femoral head could be easily found by the above examination method, and the superior ramus of the pubis, the acetabulum, the femoral head, and the femoral neck could be depicted in one plane, which was similar to the modified Shenton’s line in CT examination proposed by van Douveren et al. (Fig. 2) [5]. If the femoral neck and superior ramus of the pubis could not be depicted in one plane, their position was considered to be abnormal, and concentric reduction was not achieved (Fig. 3), suggesting timely Pavlik harness adjustment or new therapeutic regimen.
Comparison of CT cross-section in children and concentric reduction ultrasonography in children at the same age by anterior inguinal ultrasonography. a Ultrasonography of a left hip. b CT cross-section of left hip in children at the same age (black down-pointing triangle indicates superior ramus of the pubis; black star, acetabulum; white arrow, femoral head; black arrow, femoral neck; S, modified Shenton’s line)
Comparison of CT cross-section in children and failed concentric reduction ultrasonography in children at the same age by anterior inguinal ultrasonography. a Ultrasonography of a left hip. b CT cross-section of the left hip in children at the same age. The superior ramus of the pubis, the acetabulum, the femoral head, and the femoral neck could not be depicted in one plane (black down-pointing triangle indicates superior ramus of the pubis; black star, acetabulum; white arrow, femoral head; black arrow, femoral neck; S, modified Shenton’s line). A lot mussy echo of abnormal filling soft tissue showed in the acetabulum
Ultrasound-assisted therapy
An anterior ultrasound was performed right after the fixation of Pavlik harness in children, with weekly reexamination after that. If concentric reduction was achieved right after the help of Pavlik harness, the therapeutic regimen of harness was continued; if not, timely Pavlik harness adjustment and weekly reexamination of anterior ultrasound were performed.
If concentric reduction was failed to achieve in two weeks, the Pavlik harness method was changed to closed or open reduction after traction associated with anesthesia, followed by human position plaster fixation.
Follow-up
In cases confirmed as stable reduction by anterior hip ultrasound, Pavlik harness was not removed for four continuous weeks, and after that, the harness was removed for one hour in each day, and Graf hip ultrasound scanning was reexamined every two to four weeks until the re-examination of pelvic plain films six months after reduction. For cases with residual hip dysplasia, abduction brace was applied; reexamination of pelvic plain films was performed every three months for children younger than two years and every six months for children older than two years.
For cases that failed to achieve reduction in two weeks of Pavlik harness, new therapeutic regimen of closed or open reduction after traction was carried out associated with anesthesia, followed by two to three months of human position plaster fixation and another six to 12 months of abduction brace. During the treatment period, reexamination of pelvic plain films was conducted every three months to assess hip development.
Observation index
The observation indices in this study included age (first visit), gender, side of hip dysplasia, Graf type, success rate of anterior hip ultrasound, success rates of hip reduction right after the help of Pavlik harness and two weeks of harness, the acetabular index at the final follow-up, the Kalamchi and MacEwen classification, the incidences of residual hip dysplasia, and avascular necrosis of the femoral head.
Statistical analysis
Descriptive statistics was adopted to describe the individual characteristics of patients; the continuous variables were expressed as mean ± standard deviation if they were in accordance with normal distribution, while the others were expressed as the median and the interquartile range. The categorical variables were expressed as rate; the significance testing of differences was performed by two-tailed χ2 or Fisher’s exact test; and Bonferroni correction was used for the pairwise comparisons between multiple groups.
Results
General data
There were 39 patients (51 hips: 31 left ones and 20 right ones), including five males (6 hips) and 34 females (45 hips), with a minimum age of ten days and a maximum of 105 days at the first visit, and an average age of 54 ± 17 days. Among the 51 hips, there were 15 of Graf type D, 30 of type III, and six of type IV.
Success rate of ultrasound
In this study, 241 anterior hip ultrasound examinations were performed, with a success rate of 100%.
Ultrasound-assisted treatment
Pavlik harness was effective in 44 hips confirmed by anterior ultrasound. Pelvic X-ray plain films were performed after the removal of Pavlik harness to confirm a successful reduction of the femoral head (Fig. 4).
Anterior inguinal ultrasonogram of a left hip during treatment (male, 1 month). a Preliminary screening as Graf type IIIa. b Stable concentric reduction right after the help of Pavlik harness in a left hip confirmed by anterior inguinal ultrasonography. c Pelvic X-ray plain film of a left hip after finishing the therapy of Pavlik harness, which confirmed successful reduction of the femoral head
A total of 37 hips of reduction was achieved right after the fixation of harness, including 15 hips of Graf type D, with a success rate of 100.0%, 22 hips of type III, with a success rate of 73.3%, and none successful reduction of type IV; the difference of successful reduction rates between the three groups was statistically significant (p < 0.001, Table 1). Pairwise comparisons between the three groups showed that there was no significant difference of reduction rates between type D and type III hips, but the reduction rates of the above two groups were significantly higher than those of the type IV hips (p < 0.0001 and p < 0.002, respectively).
Among the 14 hips (8 hips of Graf type III, 6 of type IV) that did not initially achieve concentric reduction, seven hips (6 of type III and 1 of type IV) achieved stable reduction after two weeks of harness therapy, while the other seven hips (2 of type III and 5 of type IV) could not achieve concentric reduction in two weeks of harness therapy confirmed by anterior ultrasound, so the old regimen was replaced by closed reduction after traction (3 hips) and open reduction (4 hips); post-operative magnetic resonance imaging confirmed successful concentric reduction of the femoral head.
The success rate of hip reduction by harness was 86.3% (44/51); the success rates of Graf types D, III, and IV were 100.0%, 93.3%, and 16.7%, respectively; and the difference of successful reduction rates after two weeks was statistically significant (p < 0.001). Further pairwise analysis showed that there was no significant difference in the reduction rate between type D and type III hips after two weeks of harness treatment (p = 0.545), while the successful reduction rate of type IV was significantly lower than that of the above two types (both p < 0.001).
Prognosis
Follow-up with a median of 17 months was conducted. In 44 hips of successful reduction by harness and seven hips by surgery, there were eight (18.2%) and two (28.6%) cases that respectively showed residual hip dysplasia with no significant difference. Avascular necrosis of the femoral head showed in one hip of type III and the only successful reduction (by harness) hip of type IV, with a necrosis rate of 3.9% (2/51). According to the Kalamchi and MacEwen classification system, the former was type 1 and the latter was type 4. Among the 44 hips of successful reduction by harness, the avascular necrosis rate of the femoral head in Graf type IV hip was 100%, which was significantly higher than that of types D and III (2.3%, 1/43, p = 0.044).
Discussion
DDH refers to the poor coverage of the acetabulum to femoral head because of acetabular developmental defects, leading to long-term biomechanical abnormity, gradual emergence of subluxated femoral head, cartilage degeneration in the weight-bearing area, focal necrosis of the femoral head, and severe osteoarthritis; it includes acetabular dysplasia, subluxation of the hip, and hip dislocation [7]. At present, hip sonography is widely used for initial screening of suspected DDH newborns, and examiner-dependent factors have been discussed to influence sonographic measurements [8, 9]. Late diagnosis and intervention can exacerbate different types of DDH: from acetabular dysplasia to subluxation or dislocation. The therapeutic regimen of DDH is related to the age of the child patients. For children younger than 6 months, Pavlik harness method is, currently, commonly accepted; however, the worse the initial dislocation, the higher the failure rate of Pavlik harness and the incidence of ischaemic necrotic femoral head [10]. This study showed similar results. The successful reduction rates of Graf type D, III, and IV hips by harness were 100.0%, 93.3%, and 16.7%, respectively, showing a decreasing trend. Avascular necrosis of the femoral head appeared in the only successful harness-reduction hip of type IV, suggesting that Graf type IV hips (the worst dislocation) were almost impossible to achieve reduction by Pavlik harness. Even if the reduction was successful, there was a huge risk of femoral head necrosis. The results are consistent with the findings of Upasani, Novais, and Omeroglu [10,11,12]. The reason of severe necrosis of the femoral head in this case may be due to a high degree of dislocation, resulting in great pressure on the femoral head after reduction.
The principle and goal of early DDH treatment is to simulate the physiological environment of normal hip development as much as possible in order to prevent possible early degenerative changes in children with DDH. Therefore, suitable abduction position for each patient is extremely important in the process of Pavlik harness treatment, for improper use of Pavlik harness will not promote hip development but cause iatrogenic injury and Pavlik disease [13]. In previous treatment, the position of putting on Pavlik harness mainly depended on the clinical experience of paediatric orthopaedics surgeons, and in this study, anterior ultrasound was used to observe if the position is conducive to benign development of the hip in real time and to fine adjustment of the position of harness, so that accurate and individualized treatment of each child can be achieved, and the incidence of Pavlik disease is decreased.
The previous experience for detection during Pavlik harness treatment was to re-examine the lateral hip by Graf static ultrasound to observe the reduction and stability of the femoral head as well as the developmental maturity of the acetabulum. But for dislocated hip, it has obvious limitations. Firstly, the Graf static ultrasound must be carried out with the removal of harness and the abduction of the hip, which easily leads to loss of reduction and again dislocation; it is inconducive to a stable reduction of the femoral head. Secondly, it cannot accurately and real-timely detect the concentric reduction of the femoral head with harness-fixation, so it cannot provide guidance for the proper position of harness. In 1991, Suzuki recommended the use of a special giant probe to scan the bilateral hips simultaneously through the anterior pubic symphysis in order to simulate pelvic X-ray plain films and to avoid unnecessary radiation examination in primary DDH screening [14, 15]. In Fukiage’s report, this method was used to detect the reduction of femoral head during traction and abduction [16]. In a case report of Keller and Weiss in 1988, real-time anterior ultrasound was used, for the first time, in the process of closed reduction of DDH to detect the position of the femoral head [17]. Professor van Douveren and Beek et al. utilized similar methods to confirm the position of the femoral head after closed or open surgery in children with DDH, and they compared the results with CT examinations to verify that the ultrasound examination was 100% consistent with CT findings [5, 18, 19]. In 2014, Carlile suggested that anterior ultrasound could be used to confirm the reduction of hip during the treatment of Pavlik harness [20]. This study shows that anterior ultrasound can effectively assess the reduction of hips in children with fixed Pavlik harness, the stability of reduction, and the development between the femoral head and acetabulum, which provides a clinical therapeutic evaluation of Pavlik harness. The area of femoral head in the acetabulum was found to be decreased in unstable hips, and there was a tendency for subluxation and dislocation. In this study, reexamination of anterior ultrasound showed that seven dislocated hips could not achieve stable reduction by two weeks of harness. Therefore, the treatment method was changed in time, and concentric reduction was achieved after the completion of new treatment method (confirmed by magnetic resonance imaging). The prognosis of the children was maximally improved, and the incidence of complications such as Pavlik disease and aseptic necrosis of the femoral head was minimized.
Previous literature suggested that the reduction of the femoral head often occurred in sleep (the weight of lower extremities resulting in hip abduction) during the reduction process of dislocated hips with Pavlik harness [21]. However, this study found that 100% (15/15) of children with Graf type D and 73.3% (22/30) with type III could achieve stable concentric reduction right after the help of Pavlik harness, and another seven hips gradually reached a stable concentric reduction within two weeks of Pavlik harness. Our results confirm that in dislocated hip of Graf types D and III, correct wearing of the Pavlik harness has a strong reduction effect immediately, and there is just a very small proportion of gradual spontaneous reduction after wearing harness. However, for severely dislocated hip of Graf type IV, the reduction effect of harness is extremely limited, with a success rate of 16.7% (1/6), and there is a risk of ischemic necrosis of the femoral head.
Compared with conventional radiographic imaging techniques such as X-ray or CT, ultrasonography does not have the overlapping effect caused by Pavlik harness, with better imaging results [22]. In addition, there is no radiation during ultrasonic examination, which makes it suitable for repeated examinations. Through our practice, micro-convex probes are recommended, for example, the 8C probe of GE diasonograph used in this study. The micro-convex probe is designed for paediatric abdominal or cranial ultrasound, with frequency range of 6–10 MHz and depth up to 2–14 cm. Although, its contact surface on hips is small, it has a wide field of vision and a depth sufficient to cover the entire hip with high image resolution. Compared with the linear-array probe used by Timothy, the micro-convex probe can reveal a clearer anatomical structure, also with wider application [6]. But if there is geometric distortion of using micro-convex probe for the linear arrangement of the superior ramus of the pubis, the acetabulum, the femoral head, and the femoral neck still need to be checked by further multi-case clinical practices. Additionally, scanning physicians need to be familiar with anatomical structure; in practice, the anatomical position of the superior ramus of the pubis, acetabulum, femoral head, and femoral neck needs to be depicted in one plane. Our experience is to find the superior ramus of the pubis at the very first during scanning, then move the probe laterally to find the acetabulum, and finally find the femoral head and femoral neck after a slight rotation of the probe.
There are still some shortcomings in this study. Firstly, this is a continuous retrospective case study. We only reported the treatment results of patients undergoing anterior hip ultrasound, but without any comparison between them and patients undergoing Graf ultrasound. Secondly, all the evaluation of hip anterior ultrasound examination in this study was performed by one doctor independently, which results in certain inevitably subjective deviation. The reliability and repeatability of the anterior ultrasound method argument are kind of insufficient. Finally, we had a learning curve for mastering the anterior hip ultrasound, so quality of the early- and later-obtained ultrasonic image had certain difference which would not affect the judgment of the reduction state of the femoral head but might affect the judgment of reduction quality of the femoral head.
Despite the above shortcomings, we, for the first time, adopted anterior hip ultrasound in continuous Pavlik harness treatment process, which provided an optional monitoring method for early treatment of DDH. It is easy to operate, with straightforward results. The efficacy of Pavlik harness can be evaluated without any treatment interruption, which provides timely basis for clinical decision-making. Besides, this study also found that concentric reduction can be achieved right after the help of Pavlik harness in the vast majority of Graf type D and III hips, but for severely dislocated hip of Graf type IV, abandonment of harness therapy should be considered in the early stage, for the success rate of it is very low with a risk of femoral head necrosis.
References
Gulati V, Eseonu K, Sayani J, Ismail N, Uzoigwe C, Choudhury MZ, Gulati P, Aqil A, Tibrewal S (2013) Developmental dysplasia of the hip in the newborn: a systematic review. World J Orthopedics 4(2):32–41
Graf R (1984) Fundamentals of sonographic diagnosis of infant hip dysplasia. J Pediatr Orthop 4(6):735–740
Graf R (2017) Hip sonography: background; technique and common mistakes; results; debate and politics; challenges. Hip Int: J Clinical Experimental Res Hip Pathology Therapy 27(3):215–219
Wientroub S, Grill F (2000) Ultrasonography in developmental dysplasia of the hip. The Journal of bone and joint surgery American volume 82-a (7):1004-1018
van Douveren FQ, Pruijs HE, Sakkers RJ, Nievelstein RA, Beek FJ (2003) Ultrasound in the management of the position of the femoral head during treatment in a spica cast after reduction of hip dislocation in developmental dysplasia of the hip. J Bone Joint Surgery British Volume 85(1):117–120
Woodacre T, Carlile GS, Cox PJ (2015) The “ischial limb”: a landmark on anterior ultrasound scanning used to assess reduction in developmental dysplasia of the hip. J Pediatr Orthop 35(1):62–68
Guille JT, Pizzutillo PD, MacEwen GD (2000) Development dysplasia of the hip from birth to six months. J Am Academy Orthopaedic Surgeons 8(4):232–242
Kolb A, Benca E, Willegger M, Puchner SE, Windhager R, Chiari C (2017) Measurement considerations on examiner-dependent factors in the ultrasound assessment of developmental dysplasia of the hip. Int Orthop 41(6):1245–1250
Kolb A, Schweiger N, Mailath-Pokorny M, Kaider A, Hobusch G, Chiari C, Windhager R (2016) Low incidence of early developmental dysplasia of the hip in universal ultrasonographic screening of newborns: analysis and evaluation of risk factors. Int Orthop 40(1):1–5
Upasani VV, Bomar JD, Matheney TH, Sankar WN, Mulpuri K, Price CT, Moseley CF, Kelley SP, Narayanan U, Clarke NM, Wedge JH, Castaneda P, Kasser JR, Foster BK, Herrera-Soto JA, Cundy PJ, Williams N, Mubarak SJ (2016) Evaluation of brace treatment for infant hip dislocation in a prospective cohort: defining the success rate and variables associated with failure. J Bone Joint Surg Am 98(14):1215–1221
Novais EN, Kestel LA, Carry PM, Meyers ML (2016) Higher Pavlik harness treatment failure is seen in Graf type IV Ortolani-positive hips in males. Clin Orthop Relat Res 474(8):1847–1854
Omeroglu H, Kose N, Akceylan A (2016) Success of Pavlik harness treatment decreases in patients >/= 4 months and in ultrasonographically dislocated hips in developmental dysplasia of the hip. Clin Orthop Relat Res 474(5):1146–1152
Gornitzky AL, Schaeffer EK, Price CT, Sankar WN (2016) Pavlik harness disease revisited: does prolonged treatment of a dislocated hip in a harness adversely affect the alpha angle? Journal of pediatric orthopedics
Suzuki K, Futami (1992) Ultrasonography in congenital dislocation of the hip. J Pediatr Orthop 12(3):416
Suzuki S, Kasahara Y, Futami T, Ushikubo S, Tsuchiya T (1991) Ultrasonography in congenital dislocation of the hip. Simultaneous imaging of both hips from in front. J Bone Joint Surgery British Volume 73(6):879–883
Fukiage K, Futami T, Ogi Y, Harada Y, Shimozono F, Kashiwagi N, Takase T, Suzuki S (2015) Ultrasound-guided gradual reduction using flexion and abduction continuous traction for developmental dysplasia of the hip: a new method of treatment. The bone & joint journal 97-b (3):405-411
Keller MS, Weiss AA (1988) Sonographic guidance for infant hip reduction under anesthesia. Pediatr Radiol 18(2):174–175
Smith BG, Kasser JR, Hey LA, Jaramillo D, Millis MB (1997) Postreduction computed tomography in developmental dislocation of the hip: part I: analysis of measurement reliability. J Pediatr Orthop 17(5):626–630
Beek FJ, Nievelstein RJ, Pruijs HE, de Jong PA, Sakkers RJ (2010) Transinguinal sonographic determination of the position of the femoral head after reposition and follow-up in a spica cast. Pediatr Radiol 40(11):1794–1799
Carlile GS, Woodacre T, Cox PJ (2014) Verification of hip reduction using anterior ultrasound scanning during Pavlik harness treatment of developmental dysplasia of the hip. J Orthop 11(4):174–179
Suzuki S (1994) Reduction of CDH by the Pavlik harness. Spontaneous reduction observed by ultrasound. J Bone Joint Surgery British Volume 76(3):460–462
Eberhardt O, Zieger M, Langendoerfer M, Wirth T, Fernandez FF (2009) Determination of hip reduction in spica cast treatment for DDH: a comparison of radiography and ultrasound. J Child Orthop 3(4):313–318
Funding
This work was supported by the Shanghai Science and Technology Commission (no. 16411971600).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethical Committee of the Shanghai Children’s Medical Center, Shanghai Jiao Tong University School of Medicine.
Informed consent
Informed consent was obtained from all parents of children included in the study.
Rights and permissions
About this article
Cite this article
Ge, Y., Wang, Z. & Xu, Y. Clinical study of anterior hip ultrasound (van Douveren’s method)-assisted Pavlik harness. International Orthopaedics (SICOT) 43, 1135–1141 (2019). https://doi.org/10.1007/s00264-018-4103-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4103-8







