Abstract
Purpose
The purpose of this study was to introduce a modified arthroscopic treatment technique for popliteal cyst and hypothesize that this modified technique would provide good clinical efficacy and low recurrence rate.
Methods
From January 2013 to January 2017, 34 patients with symptomatic popliteal cysts were treated with our technique. A figure-of-four position and double posteromedial portals were used to achieve adequate enlargement of the posteromedial valvular opening between the cyst and the joint cavity and complete excision of the cyst wall. MRI was used to detect the recurrence of the popliteal cyst, and the Rauschning and Lindgren score was recorded to evaluate the clinical outcome.
Results
All patients were followed up with a mean period of 14.8 months (range, 12 to 36 months). Associated intra-articular lesions were found and treated in all cases. Degenerative cartilage damage was the most common pathology, which affected 23 (67.6%) of the cases. The Rauschning and Lindgren score improved significantly after surgery, and no evidence of recurrence was found from MRI in any case.
Conclusions
Our modified arthroscopic treatment technique, using a figure-of-four position and double posteromedial portals, is effective and safe for treating popliteal cyst.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Popliteal cyst is a common ailment in the knee joint, which was first systematically described by Baker in 1877, as a distension of bursa caused by synovial fluid trapped in the bursa, mostly the gastrocnemius-semimembranosus bursa [1]. The conventional surgery method of open resection usually associates with high recurrence rate and large wound [2]. The pathological studies have found that the associated intra-articular pathology and the unidirectional valvular mechanism of the capsular fold play the key roles in the genesis of popliteal cyst [3,4,5]. Thus, if the concomitant intra-articular pathology and the unidirectional valvular mechanism were not addressed, the cyst would recur easily.
In the recent two decades, with the advances in arthroscopic techniques, a lot of arthroscopic treatment methods of popliteal cyst were proposed [6,7,8,9,10]. Some of these articles have reported low recurrence rates and satisfactory clinical results. However, these methods still required several specific instruments such as leg holders and were inconvenient to operate.
In this study, we introduced a modified arthroscopic treatment technique for popliteal cyst, using a figure-of-four position and double posteromedial portals. And we hypothesized that this modified technique would provide good clinical efficacy and low recurrence rate.
Materials and methods
Patient demographics
This study obtained the informed consent of the patients and was approved by the local ethics committee. From January 2013 to January 2017, 34 patients with symptomatic popliteal cysts were treated with the modified arthroscopic technique. There were 16 men and 18 women. The average age was 55.38 years (range, 7 to 83 years). Fourteen cases were in the left knee, and 20 cases in the right knee. The mean time of onset was 16.1 months (range, 6 to 36 months).
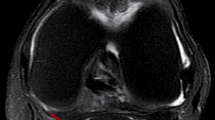
The Chief complaints included posterior knee pain, swelling, and limitation of deep knee flexion. All the patients had undergone conservative treatments for at least six months. Pre-operative magnetic resonance imaging (MRI) was performed to evaluate the cyst and the intra-articular pathology in all cases (Fig. 1). For clinical evaluation, the criteria proposed by Rauschning and Lindgren [2] was adopted. All the surgeries were operated by the same surgeon.
Surgical technique
After spinal or general anaesthesia, the patient was placed in supine position. Routine arthroscopic detection and intra-articular pathology treatment were performed via the high anterolateral (HAL) portal and anteromedial (AM) portal. After that, the knee was gently placed into a figure-of-four position, and the first standard posteromedial (PM) portal was established.
A probe was then inserted to locate the connecting opening to the cyst. Usually, the opening was located at the posteromedial side of the medial head of the gastrocnemius which was behind the capsular fold (Fig. 2). Then, we resected the capsular fold by a shaver via the PM portal and exposed the medial head of the gastrocnemius (Fig. 3). Afterward, we completely enlarged the valvular opening by the shaver and basket forceps to reestablish a normal bidirectional communication. All the operations were performed on the posteromedial side of the medial head of the gastrocnemius to avoid vessel and nerve damage.
By using a switching stick, the arthroscope was switched to the PM portal and then advanced into the popliteal cyst wall along the posteromedial side of the medial head of the gastrocnemius (Fig. 4). And then, an additional PM portal was made. This second PM portal was usually 2 cm inferior or posterior to the first PM portal, depending on the location of the cyst. Through this portal, we used the shaver and vapour to remove the inner wall of the cyst (Figs. 5 and 6). Because of the figure-of-four position, the popliteal cyst did not prolapse due to the gravity, and we could obtain a clear operation field. Moreover, we could easily change the angle of knee flexion and push the cyst from outside to assist a complete arthroscopic cystectomy (Fig. 7).
Finally, a drainage tube was inserted, and a compressive dressing was applied. Operation time ranged from 20 to 60 minutes depending on the concomitant intra-articular lesions.
Follow-up
Every patient got a follow-up for at least one year after surgery. The average period was 14.8 (range, 12 to 36) months. All cases underwent MRI at three months post-operatively and at final follow-up, to detect the recurrence of popliteal cyst. And for clinical outcome, the Rauschning and Lindgren score [2] was evaluated at three months after surgery and at the last follow-up respectively.
Results
Associated intra-articular lesions were found and treated in all cases. Degenerative cartilage damage was the most common pathology, which affected 23 (67.6%) of the cases, including 15 (44.1%) femoral chondral lesions and eight (23.5%) patellar chondral lesions. Then, medial meniscal tears were identified in 11 (32.4%) cases and followed by lateral meniscal tears in seven (20.6%) cases, synovitis in five (14.7%) cases, gout in three (8.8%) cases, and intercondylar notch stenosis in three (8.8%) cases (Table 1).
The Rauschning and Lindgren score before surgery was grade 1 in seven cases (20.6%), grade 2 in 21 cases (61.8%), and grade 3 in six cases (17.6%). At three months after surgery, the score improved significantly to grade 0 in 30 cases (88.2%) and grade 1 in four cases (11.8%) (P < 0.05). And the improvements were sustained till the last follow-up (Table 2).
In all cases, MRI was performed 3 months postoperatively and at last follow-up evaluation. No evidence of recurrence was found from MRI in any case, and none of the cysts could be palpated again after surgery till the last follow-up (Figs. 8 and 9). And we have experienced no major complications such as neurovascular injury, deep vein thrombosis, and infection during the follow-up.
Discussion
Most researchers would agree that the intra-articular pathology is essential in the formation of popliteal cyst. Sansone and De Ponti [8] indicated that the recurrence of popliteal cyst is related to intra-articular pathology, which must be corrected during the surgery. Johnson and colleagues [11] described the frequency of different kinds of intra-articular pathology. They found osteoarthritis in 81% of the popliteal cyst cases, followed by medial meniscal tears in 68%, loose bodies in 38%, oedema in 35%, and patellofemoral joint cartilage damage in 30% of the cases. Stone and associates [12] investigated 238 popliteal cysts and found meniscal tear was the most common pathology associated with a popliteal cyst. The conclusion was supported by several other scholars too [13, 14]. While Rupp and his colleagues [4] reported that articular cartilage damage was the most common intra-articular pathology associated with a popliteal cyst, in our study, we also found that the degenerative cartilage damage (including femoral and patellar chondral lesions) was the most frequently involved pathology.
Our technique of the arthroscopic surgery can provide an effective management of not only the cyst but also the intra-articular pathology, which will diminish the risk of recurrence.
Besides the concomitant intra-articular pathology, the continuous unidirectional flow of effusion from the knee joint cavity to the cyst is another essential cause of recurrence. Rauschning [15] described it thoroughly in his paper, including the capsular connection between the gastrocnemius-semimembranosus bursa and the joint cavity. This slit-shaped capsular orifice behaved like a valve. During flexion, it opened due to the pulling force of the semimembranosus tendon. While during extension, the connection closed due to compression by the overlying tendons.
In order to correct the unidirectional flow mechanism, some authors tried to close the valvular opening by valve suturing [12, 16, 17]. However, Lindgren [18] measured the pressure in the knee joint and gastrocnemius-semimembranosus bursa during normal knee flexion and extension. And he indicated that such repairs may be inefficient to sustain the normal pressure changes, which may explain relatively high failure rates of these communication-closure surgeries.
While another strategy for solving the unidirectional valvular pathology was communication enlargement, Takahashi and Nagano [6] enlarged the opening under arthroscopy by removing a slit-like structure in the posterior wall of the capsule through the posteromedial portal. Ahn and associates [19] introduced a modified arthroscopic technique with an additional posteromedial cystic portal. They corrected the valvular mechanism by resecting the capsular fold through the posteromedial working portal. Cho [10] and Ohishi [7] also disrupted the valvular mechanism via enlargement of the unidirectional valve slit. All the authors reported a high success rate, over 95%. Moreover, Sansone and De Ponti [8] also indicated that enlargement of the capsular orifice did not weaken the articular structure. Thus, communication-enlargement surgery may be an effective method for the popliteal cyst.
In our study, we also resected the capsular fold and enlarged the posteromedial valvular connecting area by at least 5 mm. And that was adequate to convert the unidirectional flow into the normal bidirectional flow between the joint cavity and the gastrocnemius-semimembranosus bursa [20]. The final follow-up result was also promising; no case of recurrence was encountered.
Furthermore, the influence of a complete cyst wall resection on the recurrence rate of the popliteal cyst is still controversial. Rauschning [16] indicated that radical excision of the cyst was not essential for the therapeutic result. Sansone and De Ponti [8] only corrected the valvular mechanism and intra-articular lesions, without removing the cyst wall. And they reported a 95% success rate. Ko [20] retained some parts of the cystic capsule but did not find any recurrence in total 14 cases. However, other authors preferred to complete cyst wall resection. Cho [10] used a 70-degree arthroscopy to get a better operative field for a complete excision of the cyst wall. All patients obtained excellent clinical results and experienced no recurrence. Ahn [19] performed a direct excisional cystectomy via the posteromedial cystic portal in 24 patients with fibrous structures within the cysts. And after a mean follow-up of 36.1 months, the cysts disappeared or reduced in size in all 24 cases.
We performed a complete excision of the cyst wall with double posteromedial portals and obtained a good therapeutic outcome. There was no case of recurrence. And we think a complete excision of the cyst wall, combined with treating intra-articular pathologies and correcting the valvular mechanism, is beneficial to diminish the possible recurrence of popliteal cyst.
Our surgical technique is a little bit different from those of other authors. We use a figure-of-four position combined with double posteromedial portals. There are some advantages of this modified method. First, it is much more simple and convenient for the surgeon to operate because the leg holders are not needed with a figure-of-four position, and the surgeon can operate upon the operating table, instead of operating from medial side but standing on the lateral side. Second, the cyst prolapses downwards and backwards due to the gravity with a common supine position, which will cause a limited operation field. With the figure-of-four position, the cyst does not prolapse but gets close to the front, which facilitates complete cystectomy. Besides, the surgeon can easily change the angle of knee flexion and push the cyst from outside to assist a complete resection of the cyst wall. Finally, the popliteal fossa usually swells after surgery due to the perfusion pressure of fluid pump. While with the figure-of-four position, the saline does not easily flow into the popliteal interstitial space because the factor of gravity is eliminated, which reduces the occurrence of swelling.
The major weakness of this study is that there is no control group with an open approach. Besides, the number of cases and the follow up are also insufficient. We will conduct further control studies with large number of cases and long term follow-up.
Conclusions
The modified arthroscopic treatment technique, using a figure-of-four position and double posteromedial portals, is effective and safe for treating popliteal cyst.
References
Baker WM (1994) On the formation of synovial cysts in the leg in connection with disease of the knee-joint. 1877. Clin Orthop Relat Res :2–10
Rauschning W, Lindgren PG (1979) Popliteal cysts (Baker’s cysts) in adults. I. Clinical and roentgenological results of operative excision. Acta Orthop Scand 50:583–591
Childress HM (1970) Popliteal cysts associated with undiagnosed posterior lesions of the medial meniscus. The significance of age in diagnosis and treatment. J Bone Joint Surg Am 52:1487–1492
Rupp S, Seil R, Jochum P, Kohn D (2002) Popliteal cysts in adults. Prevalence, associated intraarticular lesions, and results after arthroscopic treatment. Am J Sports Med 30:112–115
Lindgren PG, Willén R (1977) Gastrocnemio-semimembranosus bursa and its relation to the knee joint. I Anatomy and histology. Acta Radiol Diagn (Stockh) 18:497–512
Takahashi M, Nagano A (2005) Arthroscopic treatment of popliteal cyst and visualization of its cavity through the posterior portal of the knee. Arthroscopy 21:638
Ohishi T, Takahashi M, Suzuki D, Fujita T, Yamamoto K, Ushirozako H, Banno T, Matsuyama Y (2015) Treatment of popliteal cysts via arthroscopic enlargement of unidirectional valvular slits. Mod Rheumatol 25:772–778
Sansone V, De Ponti A (1999) Arthroscopic treatment of popliteal cyst and associated intra-articular knee disorders in adults. Arthroscopy 15:368–372
Ahn JH, Yoo JC, Lee SH, Lee YS (2007) Arthroscopic cystectomy for popliteal cysts through the posteromedial cystic portal. Arthroscopy 23:559.e1–559.e4
Cho JH (2012) Clinical results of direct arthroscopic excision of popliteal cyst using a posteromedial portal. Knee Surg Relat Res 24:235–240
Johnson LL, van Dyk GE, Johnson CA, Bays BM, Gully SM (1997) The popliteal bursa (Baker’s cyst): an arthroscopic perspective and the epidemiology. Arthroscopy 13:66–72
Stone KR, Stoller D, De Carli A, Day R, Richnak J (1996) The frequency of Baker’s cysts associated with meniscal tears. Am J Sports Med 24:670–671
Pankaj A, Chahar D, Pathrot D (2016) Arthroscopic management of popliteal cysts. Indian J Orthop 50:154–158
Artul S, Jabaly-Habib H, Artoul F, Habib G (2015) The association between Baker’s cyst and medial meniscal tear in patients with symptomatic knee using ultrasonography. Clin Imaging 39:659–661
Rauschning W (1980) Anatomy and function of the communication between knee joint and popliteal bursae. Ann Rheum Dis 39:354–358
Rauschning W (1980) Popliteal cysts (Baker’s cysts) in adults. II. Capsuloplasty with and without a pedicle graft. Acta Orthop Scand 51:547–555
Hughston JC, Baker CL, Mello W (1991) Popliteal cyst: a surgical approach. Orthopedics 14:147–150
Lindgren PG (1978) Gastrocnemio-semimembranosus bursa and its relation to the knee joint. III. Pressure measurements in joint and bursa. Acta Radiol Diagn (Stockh) 19:377–388
Ahn JH, Lee SH, Yoo JC, Chang MJ, Park YS (2010) Arthroscopic treatment of popliteal cysts: clinical and magnetic resonance imaging results. Arthroscopy 26:1340–1347
Ko S, Ahn J (2004) Popliteal cystoscopic excisional debridement and removal of capsular fold of valvular mechanism of large recurrent popliteal cyst. Arthroscopy 20:37–44
Funding
This study was supported by the Natural Science Foundation of Zhejiang Province, China (Grant No. LQ18H060004) and Medical Science and Technology Planning Project of Zhejiang Province, China (Grant No. 2017KY016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Gu, H., Bi, Q. & Chen, J. Arthroscopic treatment of popliteal cyst using a figure-of-four position and double posteromedial portals. International Orthopaedics (SICOT) 43, 1503–1508 (2019). https://doi.org/10.1007/s00264-018-4087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4087-4