Abstract
Background
Developmental dysplasia of the hip (DDH) diagnosed in older postnatal children can be effectively treated by closed reduction (CR) alone. However, no prospective or comparative trial to explore the differential effectiveness of CR between non-walking and walking postnatal children has yet been reported. This study investigated the clinical and radiologic outcomes of CR in the age range of interest (12–18 months old) via a prospective trial and compared these results with those of a younger age group who also underwent CR.
Patients and methods
Between 1999 and 2009, 56 children diagnosed with DDH were enrolled. Of these, 45 were followed after CR for a period of at least seven years. The anatomical parameters of the hip/pelvis, including arthrograms, were evaluated and compared before and after CR. The final radiologic status, including the occurrence of avascular necrosis (AVN), and clinical outcomes were evaluated and compared.
Results
The mean ages at the start of treatment were 6.11 and 15.29 months old in group 1 and group 2, respectively. None of the children required surgical open reduction during the follow-up period. The final status of hips were classified according to the Bucholz-Ogden system. Two type II hips and one type I hip were found in group 1. In group 2, two type I hips and one type III hip were observed at the final follow-up. The overall clinical outcomes were satisfactory in both groups, according to McKay’s criteria. No significant differences in clinical outcomes between the two groups were found (P = 0.382). Surgery was performed for just one patient in group 2 at seven years old.
Conclusions
CR in DDH for postnatal children 12–18 months old may provide similar results to the non-walking age group if performed with preliminary traction, gentle CR under general anaesthesia, percutaneous adductor tenotomy, and the minimization of forceful abduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) can be detected early via neonatal screening and sonographic techniques [1]. Therefore, late diagnosis is very rare and is mainly ascribed to extensive neonatal screening in developed countries. However, some cases are still diagnosed late as a result of the late presentation of DDH or missed diagnosis in other countries. Although there is no consensus in the literature on the preferred treatment modality in infants who are of walking age (≥12–15 months), most surgeons choose to perform open reduction (OR) with or without femoral or pelvic osteotomy.
The occurrence of pathologic changes such as inverted and hypertrophied labrum, excessive pulvinar degeneration, and contracted iliopsoas tendon and hip capsule, along with increased shallowness of the acetabulum, make closed reduction (CR) difficult [2, 3]. Many surgeons have recommended OR for walking-age children for two main reasons: the more frequent rate of additional surgery after CR, and avascular necrosis (AVN) of the head evoked by forceful traction/abduction during CR [4, 5]. However, other authors have suggested the use of CR, emphasizing the benefits of minimizing the limitations of the post-operative range of motion of the hip joint or iatrogenic AVN related to surgery [2].
It is currently accepted that children who present over 24 months old should not be considered for conservative treatment [6]. However, to the best of our knowledge, there has been no prospective or comparative trial regarding the differential effectiveness of CR between children who are of walking and non-walking age. We investigated the clinical and radiological outcomes of CR in children 12–18 months old through a prospective trial, and compared the results with those of a younger age group who also underwent CR.
Materials and methods
Patient selection
This study was approved by our Institutional Review Board and the parents of all subjects provided written informed consent prior to participation. We prospectively included 56 children diagnosed with DDH at our hospital (a tertiary referral hospital) between January 1999 and December 2009. The children were all initially diagnosed and referred to our institute without previous treatment history. Six patients met the exclusion criteria and were not included. In all, 31 subjects less than 12 months old who were unable to walk without any support were designated as group 1 (the non-walking age group); 19 children between 12 months and 18 months old (i.e., after the start of walking; the walking age group) were classified as group 2. The exclusion criteria were as follows: non-walking children 12 months old or older, walking earlier than 12 months, neuromuscular disease, syndromal hip subluxation or dislocation with chromosomal abnormalities, history or sequelae of septic hip, bilateral DDH, DDH combined with other lesions on any side of the lower extremities such as congenital metatarsus adductus, history of previous hip surgery, and failed previous treatment. In addition, three children in group 1 and two children in group 2 were lost to follow-up. Ultimately, a total of 28 and 17 children in group 1 and group 2, respectively, were evaluated and compared. Demographic data prior to reduction are given in Table 1.
Initial radiological evaluation before closed reduction
Radiographs taken prior to CR were evaluated for the degree of dislocation, using the Tönnis system [7]. This system has four categories focused on the location of the centre of the ossific nucleus related to Perkins’ line and to a horizontal line at the level of the lateral margin of the acetabulum. In addition, the acetabular index (AI), the centre-edge angle (CEA), c/b ratio, Sharp’s angle, and the teardrop figure [6, 8,9,10,11,12] were evaluated. The AI is the angle formed by the acetabular roof line and the horizontal line connecting both triradiate cartilages (the Hilgenreiner line). The CEA is the angle formed by a line perpendicular to the tilt of the pelvis and through the centre of the spherical femoral head and a line from the centre of the femoral head to the lateral aspect of the congruent sourcil. We calculated the c/b ratio, which is the ratio between the distance from the most medial femoral metaphysis to the midline and the distance from Perkins’ line to the midline. Sharp’s angle was measured between the teardrop line and a line through the lateral acetabular edge. The teardrop figure was evaluated as open, closed, crossed, or reverse [6, 11, 12].
Traction before reduction
Children with stage 3 (capital femoral epiphysis at the level of the superior acetabular rim) or 4 (capital femoral epiphysis above the level of the superior acetabular rim) according to the Tönnis system were placed in Bryant traction for a period of at least one week. If the traction was tolerable, this period was increased by an additional week. The angles were evaluated twice: at initial presentation and after preliminary traction, just prior to CR.
Closed reduction and arthrogram with or without adductor tenotomy
CR and an intraoperative arthrogram were performed under general anaesthesia. Hips were immobilized by a spica cast for a total of 12 weeks. At the initial primary CR (an initial period of six weeks), the hip abduction angle was allowed to exceed the safe zone for stable reduction, even above 70°. During the second reduction under general anaesthesia following the first CR, the stability of the reduction was checked by an arthrogram. If the stability of the reduction was not maintained appropriately, conversion to OR was considered. If stable, the hip spica cast was changed to a less abducted position within the safe zone, and the second cast was maintained for a further six weeks. All patients were treated with an abduction brace after removal of the spica cast for a period of more than three months (from 3 months to 12 months) until concentric reduction was seen on a standing anteroposterior radiograph of the pelvis taken while the patient was not wearing the brace. Arthrography was performed immediately after each attempted reduction under general anaesthesia. Miyake’s classification was used to assess the quality of the reduction. This defines the type of limbus as follows: normal, everted (a blunted and enfolded shape causing minimal block to reduction); intermediate, inverted (enfolded and interposed between the femoral head and the acetabulum); blockaded (prevents the entrance of the dye into the true acetabulum and has an ill-defined shape); and impossible, which obviously prevents reduction [6, 11].
Radiological and clinical evaluation at final follow-up
The AI, CEA, c/b ratio, Sharp’s angle, and teardrop figure were checked at the final follow-up. In addition, a radiological assessment of the anatomical results was performed, as described by the Severin criteria [8, 11]. The presence of AVN was also determined using the Bucholz–Ogden classification system [13]. Clinical outcomes at the final status were determined using McKay’s criteria, as modified by Berkeley et al. [8] (Fig. 1 and Table 2).
(a) A radiograph demonstrating the developmental dislocation of the left hip in a 17-month-old girl (group 2). (b) Thirteen weeks after closed reduction (closed reduction two times), the brace was maintained with 15° flexion and 50° abduction for a period of three months. (c) Two years and months months after the closed reduction (at four years old), a well-concentrated head with mild flattening was observed, and the acetabular index was less than 7 compared to the contralateral normal side. (d) The final follow-up at ten years old showed a well remodeled acetabulum and concentrated, spherical head without definitive deformities or any findings of avascular necrosis, and the clinical status according to Mckay’s criteria was I (excellent)
Statistical analysis
Continuous variables, such as age and the various angles, were analyzed and compared between the groups using an independent t-test or the Welch-Aspin test. Within each group, comparisons of pre/post-reductive continuous variables were performed by a paired sample t-test and comparisons of categorical variables were made using the chi-square test. Data were analyzed using SPSS for Windows (SPSS Inc., Chicago, IL, USA). A P value <0.05 was considered to indicate statistical significance.
Results
The mean age at the start of treatment was 6.11 ± 0.96 and 15.29 ± 1.36 months old in group 1 and group 2, respectively (P = 0.008). The distribution of Tönnis system categories did not significantly differ between the two groups (P = 0.80). In group 1, 22 children with Tönnis stage 3 or 4 underwent preliminary traction for two weeks. In group 2, nine children with stage 3 or 4 tolerated two weeks of traction, but three children with these stages only underwent traction for a week with decreased compliance. The mean AI at the initial visit was 40.21 ± 2.44 in group 1 and 39.2 ± 2.24 in group 2 (P = 0.28). The CEAs were all negative and the c/b ratios in the two groups were without significance (P = 0.33). In addition, Sharp’s angle was 50.21 ± 2.17 in group 1 and 49.47 ± 1.84 in group 2 (P = 0.24). The distributions of the initial teardrop shape did not differ between the two groups (P = 0.83).
All patients of both groups exhibited stable concentric reduction during two CRs, as revealed on concurrent arthrograms, and none required a different surgical option. The number of normal classifications according to Miyake’s criteria was 1 (3.6%) and 0 (0%); there were 7 (25%) and 1 (5.9%) everted classifications, 16 (57.1%) and 7 (41.2%) intermediate classifications, and 4 (14.3%) and 8 (47.1%) inverted classifications in group 1 and group 2, respectively. There was only one blocked classification, and that occurred in group 2 alone. Moreover, the distributions were not significantly different (P = 0.06). The Severin criteria at the final follow-up showed 22 children of type I (78.6%) and six of type II (21.4%) in group 1, and 13 of type I (76.5%), three of type II (17.6%), and one of type III (5.9%) in group 2, without significance (P = 0.42). The AI, CEA, c/b ratio, and Sharp’s angle were significantly improved in both groups (P < 0.05), but the differences in improvement were without significance (P > 0.05). The findings of AVN from simple radiographs were observed in three children in both groups at the final follow-up. Two type II hips according to the Bucholz-Ogden system and one type I hip were found in group 1. In group 2, two type I hips and one type III hip were seen at the final follow-up. Surgery was performed in the child with a type III hip who was seven years old. Overall clinical outcomes were satisfactory and no child in either group demonstrated a poor grade according to McKay’s criteria. There were no significant differences in clinical outcomes between the two groups (P = 0.38).
Discussion
When DDH is detected at birth, it can usually be corrected with the use of a harness or brace. If not diagnosed at birth, however, the condition remains unnoticed until the child begins to walk. At this time, treatment options are more complicated and provide less predictable results. Many authors have suggested that the indications for treatment should be based on the quality and stability of the initial reduction, and that CR is indicated only when a concentric and stable reduction of the hip can be obtained. Good results from CR have been reported in many studies, but success rates range widely, from 57 to 94% [10, 13,14,15,16,17,18,19]. The various rates mainly derive from the heterogeneities of the age distributions in each study, as noted by Murray [20]. Before the 2000s, the highest success rate (88%) was reported by DeRosa [17], and it is interesting to note that 72% of the patients in that study were six months old or less, suggesting that CR is more successful in younger patients. In the late 2000s, Murray [20] reported a success rate of up to 94% in CR for young children, with rates of 64% for patients less than six months old and 36% for those less than five months old. Murray concluded that at least two factors might contribute to the high success rate. One factor suggested was the acceptance of a 70° hip abduction, but never forced abduction, at the time of CR to achieve stability. The rationale that the degree of abduction not be harmful was supported by the relatively low rate of AVN in their patients.
Race and Herrings reported the results of CR for a group of children of walking age and emphasized that the level of initial reduction, rather than age, was the best predictor of future outcome [18]. It is interesting to note that, in several studies, temporary irregular ossification did not necessarily develop during follow-up due to the clinically significant AVN of the criteria used by Salter, Kalamchi, and MacEwen [14, 15, 19, 21]. Preliminary traction before CR may be a benefit of minimizing AVN during follow-up [13, 15], but definitive statistical comparisons of the benefits of traction vs. no traction have yet to be clarified [13, 14, 21]. We hypothesized that if concentric and stable reduction were achieved, age would be a less decisive factor for the final outcome. Furthermore, a comparative study of the outcomes of CR based on age has not been undertaken until now. Therefore, we compared the effectiveness of CR between two different age groups according to their walking status. The treatment algorithm used in our study allowed hyper-abduction of about 70–80° for proper concentric reduction during the initial CR without the need for forceful manipulation, as suggested by Murray [20]. We regarded the second examination six weeks after the initial CR as the most important point. An improvement in Miyake’s criteria between the initial and second arthrogram was found in some children (16/18, 89%) in group 2 (Figs. 2 and 3). Moreover, most of them showed satisfactory outcomes according to the Severin criteria and Bucholz–Ogden grading at the final follow-up. The rate of AVN determined by the Bucholz–Ogden system was 11% (3/28) and 18% (3/17) in group 1 and group 2, respectively, but clinically important surgery was required in only one patient in group 2. The overall rate of incidence was satisfactory, similar to Murray et al. [20]. We agree that this acceptably low rate of incidence of AVN originated from careful attention to the principles of preliminary traction, gentle CR performed under general anaesthesia, percutaneous adductor tenotomy, and the minimization of forceful abduction, as suggested by Zionts [5]. We observed temporary irregular ossification in 8 (29%, 8/28) patients in group 1 and 6 (35%, 6/17) in group 2. As shown by Bucholz and Ogden [13] and Zionts [5], we confirmed that it was related to the temporary partial occlusion of segments of the vascular supply to the epiphysis, with little impact on the physis and metaphysis during the follow-up period (Fig. 4). According to the concept of avascular insult to the epiphysis with sparing of the physis, we determined that these findings were not associated with subsequent growth abnormalities such as those seen after the more severe types of AVN throughout the follow-up period.
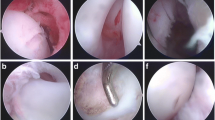
(a) A radiograph demonstrating the developmental dislocation of the right hip in a 16-month-old girl (group 2). (b) After the initial closed reduction, an arthrogram was obtained, and a definitively inverted labrum was observed. (c) Six weeks later, a second closed reduction followed by arthrography revealed improvement in terms of Miyake’s classification (an everted or intermediate labrum). (d) The final follow-up at 11 years of age revealed a well-remodeled acetabulum and a concentrated spherical head without clinical deterioration. Despite a minor deficiency in terms of acetabular coverage, the overall clinical condition was excellent
(a) A radiograph demonstrating developmental dislocation of the right hip in a 15-month-old girl (group 2). (b) After the initial closed reduction, the computed tomography angiogram revealed incomplete reduction despite the application of preliminary traction and adductor tenotomy. (c) The second reduction was associated with improved reduction status. (d) After a total of six weeks in a cast, an abduction brace was applied for a period of ten months. (e) The final follow-up (at 9 years of age) revealed a well-remodeled acetabulum and a concentrated spherical head without any clinical deterioration. Further improvement of coverage is expected
(a) A radiograph demonstrating the developmental dislocation of the left hip in a 15-month-old girl (group 2). (b) After 12 weeks with the cast, a brace was applied for a period of 8 months. (c) Twenty-two months after the first reduction, temporary irregular ossification was found in the left hip. (d) At the final follow-up (at an age of eight years old), a well-remodeled spherical head and acetabular cavity was observed
The strength of this study lies in the fact that we checked the intra-operative arthrogram twice in all patients and were therefore able to confirm changes in the soft tissues around the joint. We conclusively evaluated the status of the second reduction (in terms of good concentricity) via arthrography. CR for a developmentally dislocated hip developing after the age of walking should still be considered the primary treatment option, if prolonged immobilization using an abduction brace is tolerable.
This study had a number of limitations. First, the number of hips was not sufficient for power analysis to suggest differences in the outcomes. Instead, we compared the final clinical and radiological outcomes of the two age groups. Moreover, the upper age limit (cut-off value) for CR and the remaining potential for acetabular remodeling were unable to be determined from this study. Second, there were some difficulties in maintaining traction before the application of the hip spica cast in group 2. Older children did not tolerate the Bryant traction for the whole two-week period and, inevitably, the period of traction was irregular, with some patients only undergoing traction for a period of one week. Thus, the impact of pre-reductive traction for favourable outcomes was unclear.
References
Kahle KW, Anderson MB, Alpert J, Stevens PM, Coleman SS (1996) The value of preliminary traction in the treatment of congenital dislocation of the hip. J Bone Joint Surg Am 72:1043–1047
Sharpe P, Mulpuri K, Chan A, Cundy PJ (2006) Differences in risk factors between early and late diagnosed developmental dysplasia of the hip. Arch Dis Child Fetal Neonatal Ed 91(3):F158–F162
Heesakkers NA, Witbreuk MM, Besselaar PP, Van Der Sluijs JA (2013) Retrospective radiographic evaluation of treatment results of developmental dysplasia of the hip in walking-age children. J Pediatr Orthop B 22(5):427–431
Imatani J, Miyake Y, Nakatsuka Y, Akazawa H, Mitani S (1995) Coxa magna after open reduction for developmental dislocation of the hip. J Pediatr Orthop 15(3):337–341
Zionts LE, MacEwen GD (1986) Treatment of congenital dislocation of the hip in children between the ages of one and three years. J Bone Joint Surg Am 68:829–846
Mitani S et al (1997) Treatment of developmental dislocation of the hip in children after walking age. J Bone Joint Surg 79(5):710–718
Quinn RH, Renshaw TS, DeLuca PA (1994) Preliminary traction in the treatment of developmental dislocation of the hip. J Pediatr Orthop 14:636–642
Berkeley ME et al (1984) Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg 66(3):412–420
Lee YK, Chung CY, Koo KH (2011) Measuring acetabular dysplasia in plain radiographs. Arch Orthop Trauma Surg 131(9):1219–1226
Cashman JP, Round J, Taylor G, Clarke NM (2002) The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up. J Bone Joint Surg Br 84(3):418–425
Liu JS, Kuo KN, Lubicky JP (1996) Arthrographic evaluation of developmental dysplasia of the hip. Outcome prediction. Clin Orthop Relat Res 326:229–237
Joseph K, MacEwen GD, Boos ML (1982) Home traction in the management of congenital dislocation of the hip. Clin Orthop 165:83–90
Bucholz RW, Ogden JA (1978) Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease. In: The hip. Proceedings of the Sixth Open Scientific Meeting of the Hip Society. CV Mosby Co., St. Louis, pp 43–63
Zadeh HG, Catterall A, Hashemi-Nejad A, Perry RE (2000) Test of stability as an aid to decide the need for osteotomy in association with open reduction in developmental dysplasia of the hip. J Bone Joint Surg Br 82(1):17–27
Mitani S, Nakatsuka Y, Akazawa H, Aoki K, Inoue H (1997) Treatment of developmental dislocation of the hip in children after walking age. Indications from two-directional arthrography. J Bone Joint Surg Br Sep 79(5):710–718
Tonnis D (1982) Congenital hip dislocation. Thieme-Stratton Inc, New York
DeRosa GP, Feller N (1987) Treatment of congenital dislocation of the hip. Management before walking age. Clin Orthop 225:77–85
Race C, Herring JA (1983) Congenital dislocation of the hip: an evaluation of closed reduction. J Pediatr Orthop 3:166–172
Malvitz TA, Weinstein SS (1994) Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am 76:1777–1792
Murray T, Cooperman DR, Thompson GH, Ballock T (2007) Closed reduction for treatment of development dysplasia of the hip in children. Am J Orthop (Belle Mead NJ) 36(2):82–84
Badgley CE (1949) Etiology of congenital dislocation of the hip. J Bone Joint Surg Am 31(2):341–356
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement and source of funding
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Additional information
Level of Evidence: Therapeutic Level II
Rights and permissions
About this article
Cite this article
Cha, S.M., Shin, H.D. & Shin, B.K. Long-term results of closed reduction for developmental dislocation of the hip in children of walking age under eighteen months old. International Orthopaedics (SICOT) 42, 175–182 (2018). https://doi.org/10.1007/s00264-017-3685-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3685-x