Abstract
Purpose
Spinal epidural haematoma (SEH) is a common complication after lumbar spinal decompression surgery, and symptomatic SEH usually causes devastating neurological deficits. Although different risk factors for post-operative SEH have been reported, few studies focused on patients’ laboratory tests. The purpose of this study was to analyze the incidence of symptomatic SEH following lumbar spinal surgery, as well as identify the risk factors for it.
Methods
Patients who underwent posterior lumbar spinal decompression surgery between January 2010 and August 2016 were included in this study and their medical records were retrospectively reviewed. Those who developed post-operative symptomatic SEH after the surgery were identified. The risk factors for SEH were analyzed by univariate and multivariate regression analysis.
Results
In total, 2715 patients were included in this study and 31 (1.14%) were identified with post-operative symptomatic SEH. Of these patients, 19 were males and 12 were females, with an average age of 59.39 ± 11.66 years. After multivariate logistic regression analysis, low serum calcium level (P = 0.025), blood type A (P = 0.04), increased estimated blood loss (P = 0.032), prolonged surgical duration (P = 0.018), and decreased post-operative globulin (P = 0.016) were identified as the independent risk factors for post-operative SEH following lumbar spinal surgery. Furthermore, prolonged surgical duration (odds ratio = 3.105) was the strongest risk factor for SEH.
Conclusion
Based on a large population investigation, the incidence of symptomatic SEH following lumbar spinal decompression surgery was 1.14%. Blood type A, increased estimated blood loss, and prolonged surgical duration were identified as the independent risk factors for post-operative SEH while two new risk factors, including low serum calcium level and decreased post-operative globulin, were firstly identified in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal epidural haematoma (SEH) is a relatively rare complication following spinal surgery, mostly occurring in lumbar spinal surgery. Although the asymptomatic SEH has been detected by magnetic resonance imaging (MRI) in 15-89% of patients undergoing spinal surgery [1,2,3], the incidence of symptomatic SEH was only 0.1-0.4% [4,5,6]. However, post-operative symptomatic SEH usually caused severe neurological symptoms by compressing the spinal cord and nerve roots, including paralysis, bowel and bladder dysfunction, saddle anesthesia, lower extremities weakness and numbness [7]. In most symptomatic cases, SEH needs a revision surgery for evacuation, haemostasis, and decompression in order to save the function of spinal cord and nerve roots. Thus, understanding the risk factors for post-operative SEH is helpful for the surgeon to timely diagnose the serious complication and prevent it.
Previous studies have reported a variety of risk factors for post-operative SEH after spinal surgery, including pre-operative diastolic blood pressure, advanced age, high body mass index, coagulopathy, intra-operative use of gelfoam, multilevel procedures, increased estimated blood loss, post-operative drain output, increased systolic blood pressure after extubation, and so on [2, 6, 8]. However, some of the factors were still controversial and identified just based on a small population. Additionally, most of the studies were focused on patients’ characteristics and procedure-related factors. Few studies paid attention to the correlation of laboratory tests and post-operative SEH, especially the liver, kidney function, and electrolyte results of patients.
The purpose of this study was to analyze the incidence of symptomatic SEH and identify the risk factors for it following lumbar spinal surgery based on a large population analysis.
Materials and methods
Study design
This study was approved by the ethics committee of our hospital and all patients signed informed consent before participation. Patients who underwent posterior lumbar spinal decompression surgery between January 2010 and August 2016 were included in this study. Decompression surgery included surgery for spinal canal and foraminal stenosis resulting from lumbar spinal degenerative diseases, except for spinal tumor, infection, deformity, and vertebral fracture. Patients with coagulopathy or coagulation disorder were excluded from this study.
All patients underwent surgery with general anesthesia. Four senior spine surgeons performed the surgery. No haemostasis medicine was used pre-operatively and intra-operatively for patients. Anticoagulation therapy was not used in patients in order to decrease the potential confounding variables for the risk factors analysis. All patients were given physical therapy for the prophylaxis of post-operative deep venous thrombosis. Subfascial drains were performed in all patients before closing the incision. The drains were removed when the drainage volume was less than 50 ml/24 h.
Identification of SEH
In this study, patients with post-operative SEH who required revision surgery for haematoma evacuation after the primary lumbar spinal decompression surgery were identified for analysis. The diagnosis of SEH was based on the neurological symptoms and confirmed by following MRI examination or surgical findings. The symptoms of developing post-operative SEH included: (1) severe back pain at the surgical level; (2) unilateral or bilateral low extremity radicular pain; (3) bladder and/or bowel dysfunction; (4) low extremity weakness and numbness.
Data collection
In order to analyze the risk factors for post-operative SEH, a case control study was carried out. Each patient with SEH was matched with three controls who underwent lumbar spinal decompression surgery at the same period but without post-operative complications. The match was performed according to patient’s age, gender, and diagnosis. All the medical records of patients in the two groups were reviewed with a follow up period of 30 days. Patients’ characteristics and peri-operative factors, including the laboratory test results, were collected for the analysis.
Statistical analysis
All the continuous variables were presented as average ± standard deviation. Univariate analysis was firstly carried out to identify the potential risk factors associated with SEH. For continuous variables, the student t test was used to compare the outcomes between the two groups. For dichotomous variables, χ2 tests or Fisher’s exact test were performed. Multivariate logistic regression analysis was then conducted to identify the independent risk factors for SEH. A P < 0.05 was considered as significant. All the analysis was performed using SPSS 19.0 (IBM, Chicago, IL).
Results
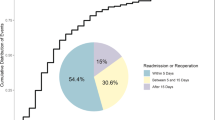
According to the inclusion and exclusion criteria, a total of 2715 patients were included in this study. Among these patients, 31 (1.14%) were identified with postoperative symptomatic SEH. Nineteen of them were males and 12 were females, with an average age of 59.39 ± 11.66 years. Another 93 patients who underwent posterior lumbar spinal decompression surgery at the same period were included as the control group. No significantly statistical differences were found on age, gender, and diagnosis between SEH and control groups (P > 0.05).
Univariate analysis
Patients’ characteristics and pre-operative factors were compared between the SEH group and control group (Table 1). The results showed that patients in the SEH group had significantly lower concentrations of platelet (P = 0.031), total protein (P = 0.007), albumin (P = 0.013), serum calcium (P < 0.001), and lower glycated hemoglobin (P = 0.009) than those in the control group. Additionally, patients with SEH had a significant higher proportion of blood type A than those without SEH (P = 0.022). The outcomes indicated that these factors were potentially associated with postoperative SEH.
The univariate analysis results for the intraoperative factors between patients with and without post-operative SEH were displayed in Table 2. It indicated that multilevel surgical segments (P < 0.001), prolonged surgical duration (P = 0.021), increased estimated blood loss (P < 0.001), and large allogeneic blood transfusion (P = 0.042) were significantly related to post-operative SEH.
For the postoperative factors, the comparison results between patients in SEH group and control group were demonstrated in Table 3. The globulin and serum level of calcium in patients with SEH were significantly lower than those in control group (P = 0.009 and 0.003).
Multivariate analysis
All related factors identified by univariate analysis were finally included for the multivariate logistical regression analysis to detect the independent risk factors for post-operative SEH. Table 4 showed the multivariate analysis results. Based on the analysis, low serum calcium level (P = 0.025), blood type A (P = 0.04), increased estimated blood loss (P = 0.032), prolonged surgical duration (P = 0.018), and decreased post-operative globulin (P = 0.016) were identified as the independent risk factors for SEH. Moreover, prolonged surgical duration (odds ratio = 3.105) was the strongest risk factor for SEH after lumbar spinal surgery.
Discussion
Although symptomatic SEH is rare following spinal surgery, the consequence of it is devastating, causing spinal canal compromise and nerve roots compression, which usually leads to permanent neurological dysfunction [9]. Several studies have reported the incidence of post-operative SEH, but the samples included in these studies were relatively small [3]. During the past five years, some large population studies have been carried out for post-operative SEH analysis. Kao et al. [10] reviewed over 15,500 lumbar spine surgeries and identified an incidence of 0.16% patients with post-operative SEH. Aono et al. [4] analyzed the medical records of 6356 patients who underwent spine surgery and found that the incidence of SEH was 0.50% in lumbar laminectomy and 0.67% in lumbar interbody fusion surgery. In another large population study, Yamada et al. [11] retrospectively reviewed 8250 patients who underwent spinal decompression procedure, and found the incidence of SEH was 0.39% in patients with lumbar procedures. In the present study, the incidence of symptomatic SEH following posterior lumbar spinal surgery was 1.14%, which was a little higher than those reported in previous studies. The reasons for this may be the long surgical time and large estimated blood loss during the surgery in SEH patients, both of which were finally identified as the risk factors for SEH in our study.
A variety of risk factors for postoperative SEH have been reported in previous studies [2, 6, 8]. Different from the literature, this study was just focused on patients with degenerative lumbar spinal diseases, and patients with spinal tumour, infection, deformity, and fracture were excluded, which would decrease the potential confounding factors for the analysis. Based on the analysis, blood type A, increased estimated blood loss, and prolonged surgical duration were finally identified as the independent risk factors for post-operative SEH after lumbar spinal surgery in our study. In addition, some new risk factors, including low serum calcium level and decreased post-operative globulin, were firstly detected for SEH in the present study.
The finding of blood type A as a risk factor for postoperative SEH was rarely reported in previous studies. Awad et al. [8] reviewed the records of 14,932 patients undergoing spinal surgery and found Rh-positive blood type significantly increased the risk for SEH, but the authors did not give the reason for it. In our study, patients with blood type A had a significantly higher rate of SEH than patients with other blood types. The reason for it was unclear, but this result will remind surgeons to pay attention to patients’ blood type before performing lumbar spinal surgery.
Similar to previous studies, increased estimated blood loss was identified as the risk factor for post-operative SEH in our study. The reason for this may be that large blood loss during the surgery would result in coagulation dysfunction and haemorrhage. Furthermore, increased blood loss would cause low haemoglobin and more allogeneic blood transfusion, which aggravated coagulation dysfunction. Kazui et al. [12] reported that a haematoma volume greater than 25 cm3 was a strong risk factor for haematoma enlargement in patients with spontaneous intracerebral haemorrhage. Awad et al. [8] indicated that estimated blood loss >1 L was one of the risk factor for post-operative SEH after spinal surgery. Thus, spine surgeons should try their best to perform haemostasis during lumbar decompression surgery to reduce the incidence of SEH.
Although prior studies have rarely reported the relationship between surgical time and post-operative SEH following lumbar spinal surgery, we found that prolonged surgical duration was significantly associated with post-operative SEH. Prolonged surgical duration usually led to a large estimated blood loss and low post-operative haemoglobin, which increased the risk of post-operative SEH [8]. On the other hand, prolonged surgical duration would increase the probability of epidural venous plexus injury, which was significantly related to post-operative SEH [13]. In addition, several studies have reported that a multilevel procedure was an important risk factor for SEH following spinal surgery [2, 5, 6]. One of the reasons was a multilevel procedure would increase the surgical duration and finally result in a high risk of post-operative SEH. We also found that prolonged surgical duration (odds ratio = 3.105) was the strongest risk factor for SEH in our study. Thus, spine surgeons should reduce the surgical duration so as to decrease the rate of post-operative SEH.
As a new finding risk factor for SEH, low serum calcium level was not reported in prior literature. In the current study, we found pre-operative low serum calcium level was significantly correlated with post-operative SEH. Calcium is an important cofactor for the function of coagulation cascade and plays a critical role in the tenase and prothrombinase complexes function [14, 15]. It mediates the binding of the complexes to the phospholipid surfaces expressed by platelets and helps procoagulant microparticles or microvesicles shed from them [16]. When the concentration of serum calcium decreases, the function of blood clot will be impaired and the risk of haemorrhage increases. So, it’s helpful to keep the preoperative serum calcium at normal level for patients undergoing lumbar spinal surgery.
Another new risk factor for post-operative SEH was decreased post-operative globulin in the present study. Based on the analysis, the decrease of globulin after lumbar spinal surgery significantly increased the risk of SEH. Globulin is one part of the serum protein. It is reported that globulin takes part in the formation of coagulase-thrombin [17], and plays an important role in blood coagulation [18]. Thus, the decreased serum globulin level would impair the coagulation function of patients.
Based on the present study, surgeons should pay attention to the risk factors for post-operative SEH before carrying out lumbar spinal surgery, and keep the pre-operative laboratory test results at normal levels. In addition, taking effective measures to shorten the surgical duration and stopping bleeding carefully during the operation are more important for decreasing the incidence of SEH. Furthermore, post-operative abnormal serum globulin level should be corrected and the coagulation function of patients should be monitored after the surgery. If the symptoms of SEH were developed after lumbar spinal surgery, emergency surgical decompression is necessary in order to save the neurological function.
In the present study, although several new independent risk factors were identified for post-operative SEH, there were still some limitations. First, it is a retrospective study and some information were incomplete in the patients, which may affect the analysis outcomes. Second, some peri-operative factors were not reported in our study because of insufficient data, such as pre-operative systolic and diastolic blood pressure, body mass index, and surgical history. Third, all patients with post-operative SEH were identified according to the revision surgery. Some patients who developed SEH but did not undergo revision surgery may be missed because of no records. Thus, a prospective, multicentre study is helpful to verify the results of this study.
In conclusion, based on a large population investigation, the incidence of symptomatic SEH after lumbar spinal decompression surgery was 1.14%. After matching for a case control study, blood type A, increased estimated blood loss, and prolonged surgical duration were confirmed as the independent risk factors for post-operative SEH while some new risk factors, including low serum calcium level and decreased post-operative globulin, were also identified in our study. Spine surgeons should pay attention to these risk factors and make a timely diagnosis of SEH if the patient develops neurological deficit after lumbar spinal decompression surgery.
References
Mirzai H, Eminoglu M, Orguc S (2006) Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech 19:171–177
Sokolowski MJ, Garvey TA, Perl J 2nd, Sokolowski MS, Cho W, Mehbod AA, Dykes DC, Transfeldt EE (2008) Prospective study of postoperative lumbar epidural hematoma: incidence and risk factors. Spine 33:108–113
Modi HN, Lee DY, Lee SH (2011) Postoperative spinal epidural hematoma after microscopic lumbar decompression: a prospective magnetic resonance imaging study in 89 patients. J Spinal Disord Tech 24:146–150
Aono H, Ohwada T, Hosono N, Tobimatsu H, Ariga K, Fuji T, Iwasaki M (2011) Incidence of postoperative symptomatic epidural hematoma in spinal decompression surgery. J Neurosurg Spine 15:202–205
Amiri AR, Fouyas IP, Cro S, Casey AT (2013) Postoperative spinal epidural hematoma (SEH): incidence, risk factors, onset, and management. Spine J: Off J North Am Spine Soc 13:134–140
Kou J, Fischgrund J, Biddinger A, Herkowitz H (2002) Risk factors for spinal epidural hematoma after spinal surgery. Spine 27:1670–1673
Cabana F, Pointillart V, Vital J, Senegas J (2000) Postoperative compressive spinal epidural hematomas. 15 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot 86:335–345
Awad JN, Kebaish KM, Donigan J, Cohen DB, Kostuik JP (2005) Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br Vol 87:1248–1252
Raasck K, Habis AA, Aoude A, Simoes L, Barros F, Reindl R, Jarzem P (2017) Spontaneous spinal epidural hematoma management: a case series and literature review. Spinal Cord Series Cases 3:16043
Kao FC, Tsai TT, Chen LH, Lai PL, Fu TS, Niu CC, Ho NY, Chen WJ, Chang CJ (2015) Symptomatic epidural hematoma after lumbar decompression surgery. Eur Spine J 24:348–357
Yamada K, Abe Y, Satoh S, Yanagibashi Y, Hyakumachi T, Masuda T (2015) Large increase in blood pressure after Extubation and high body mass index elevate the risk of spinal epidural hematoma after spinal surgery. Spine 40:1046–1052
Kazui S, Minematsu K, Yamamoto H, Sawada T, Yamaguchi T (1997) Predisposing factors to enlargement of spontaneous intracerebral hematoma. Stroke 28:2370–2375
Groen RJ, Ponssen H (1990) The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci 98:121–138
Huang LH, Ke XH, Sweeney W, Tam JP (1989) Calcium binding and putative activity of the epidermal growth factor domain of blood coagulation factor IX. Biochem Biophys Res Commun 160:133–139
Rodgers GM, Cong JY, Goll DE, Kane WH (1987) Activation of coagulation factor V by calcium-dependent proteinase. Biochim Biophys Acta 929:263–270
Sinha D, Seaman FS, Walsh PN (1987) Role of calcium ions and the heavy chain of factor XIa in the activation of human coagulation factor IX. Biochemistry 26:3768–3775
Miale JB (1949) The role of staphylocoagulase in blood coagulation; the reaction of staphylocoagulase with coagulase-globulin to form coagulase-thrombin. Blood 4:1039–1048
Miale JB (1952) The role of coagulase-globulin in blood coagulation and its thromboplastic action. Am J Clin Pathol 22:218–230
Funding
This work is supported by the Department of Science and Technology Program of Jiangxi Province, China (No. 20162BCB22022, 20162BCB23057).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the medical research ethics committee of our hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liu, JM., Deng, HL., Zhou, Y. et al. Incidence and risk factors for symptomatic spinal epidural haematoma following lumbar spinal surgery. International Orthopaedics (SICOT) 41, 2297–2302 (2017). https://doi.org/10.1007/s00264-017-3619-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3619-7