Abstract
Purpose
Lateral epicondylitis (LE), a common disease, especially in middle age, causes decreased productivity and economic losses. The first-line treatment for LE is conservative and consists of topical and oral anti-inflammatory drugs, ice application, and brace use. If the first-line treatment fails, second-line treatment modalities, which are generally invasive, are offered. Second-line therapeutic regimens include saline, corticosteroid, or platelet-rich plasma injections. Dry needling is relatively new. We hypothesized that dry needling would be at least as effective as first-line treatment for LE. We compared the outcomes of first-line treatment and dry needling.
Methods
The study allocated 110 patients into groups using online randomization software. After completing the Patient-rated Tennis Elbow Evaluation (PRTEE), patients in group I received dry needling, whereas those in group II received first-line treatment, consisting of ibuprofen 100 mg twice a day and a proximal forearm brace. The patients were evaluated after three weeks and six months.
Results
The study ultimately analyzed 92 patients. Although both treatment methods were effective at three weeks, dry needling was significantly more effective than the first-line treatment at six months.
Conclusion
Because of the low complication rate, dry needling is a safe method, and it might be an effective treatment option for LE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral epicondylitis (LE), a common disease, especially in middle age [1,2,3], causes decreased productivity and economic losses [4, 5]. The first-line treatment for LE is conservative, consisting of topical and oral anti-inflammatory drugs, ice application, and brace use. This treatment might fail to resolve the complaints of some patients, and second-line therapy modalities, which are generally invasive, are offered. Second-line treatments include saline, corticosteroid, or platelet-rich plasma injections [6, 7]. Dry needling is relatively new. Although it has been used in the management of myofascial pain [8], low back pain [4], trigger points [9], and rotator cuff tears [9], there are only two reports of dry needling in LE [3, 10].
We hypothesized that dry needling would be at least as effective for LE as first-line treatment. Therefore, this study compared the pain relief and the improvement in functional disability of first-line treatment with those of dry needling in LE patients.
Methods
Informed consent was obtained from all of the participants, and the rights of the subjects were protected. After Institutional Review Board approval was obtained for the study, patients who had pain at the lateral epicondyle for more than three months and who had pain during forced forearm supination, forced wrist extension, and forced third finger extension on physical examination were diagnosed with lateral epicondylitis. Direct x-rays of the elbow were obtained to rule out radio-humeral joint arthritis, osteochondritis dissecans, or osteonecrosis. Patients with cervical radiculopathy or posterior interosseous nerve entrapment were excluded from the study.
Assuming that the standard effect size would be 0.54, it was decided to enroll 55 cases in each group at 80% power and a 95% confidence interval. The patients were enrolled consecutively and randomized into two groups using online randomization software [11].
After the Patient-rated Tennis Elbow Evaluation (PRTEE) score was determined, dry needling was performed on the patients in group I and first-line treatment was given to group II.
After cleaning the skin with povidone-iodine, we inserted five 0.25 × 25-mm stainless steel needles (Yao Tong, Barcelona, Spain) in the trigger point regions, which were the most painful areas at the lateral epicondyle, of those in group I (Fig. 1). The needles were directed through the skin and fascia to the bone (3–5 mm). They were rotated three to four times and left in place for ten minutes. Following needle withdraw, the insertion site was compressed firmly to avoid excessive bleeding. Applications were repeated twice per week for a total of five sessions. All interventions were performed by a single, experienced physiotherapist. Patients were not allowed to take any other medication during the trial.
The first-line treatment given to patients in group II consisted of a non-steroidal anti-inflammatory drug (ibuprofen 100 mg, 2 twice per day) and a proximal forearm brace for three weeks. Patients were advised to wear their brace continuously, except while sleeping and showering.
The patients were told not to use any other treatment, including ice application, topical nonsteroidal anti-inflammatory drugs, or other oral medications, during the trial so as not to affect the outcomes during follow up. Patients were told that they would be excluded from the study if they did not comply with this prohibition.
The clinical evaluation was performed by authors who did not participate in the intervention. Patients were evaluated using the PRTEE score at three weeks and six months. The third week corresponded to seven days after the last needling sessions in group I and the last day of the first-line treatment in group II.
The statistical analysis was performed using SPSS-21.0 (Statistical Package for the Social Sciences; SPSS, Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant. Needling data were compared before and after using the paired sample t-test, and differences between groups were analyzed with the independent t-test.
Results
Although we planned to enroll 110 patients, the study was completed with 92 patients. Two (3.9%) patients in the dry needling group could not tolerate the intervention, one had a local haemorrhage, and one was lost to follow up. In the control group, 14 (25%) patients tried other therapies during the six month follow-up period. Therefore, 18 patients were excluded from the study.
There were no differences between groups in terms of sex, age, dominant arm, and PRTEE scores before the treatments. The mean age of the patients was 47.7 years in group I and 48 years in group II. Overall, 78% of the patients were female, and 22% of the study group suffered LE in their dominant arms.
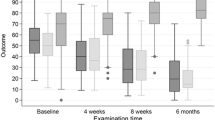
In both groups, significant differences were detected at the three week follow up (Table 1). However, the control group showed no effects at the six month follow up, whereas dry needling was effective at both three weeks and six months.
In both groups, a significant difference (p < 0.05) in PRTEE (pain and function) scores was detected between before and after treatment at three weeks. Although the mean PRTEE (pain and function) score of the control group at six months was higher than that before treatment, the difference was not significant (Table 2).
Three patients (5.8%) from group I had complications: two patients could not tolerate the pain during the intervention and one had a local hemorrhage.
Discussion
Lateral epicondylitis (LE), which is also known as tennis elbow, periostitis, extensor carpi radialis brevis-tendinosis, and epicondylalgia, is obscure and controversial. Because inflammatory cells are absent in LE, the term periostitis has fallen into disuse [5, 12]. LE is common, especially in middle age [12]. Studies report no gender difference, whereas tobacco consumption and forceful supination activities are risk factors [12].
Another controversial issue in LE is its pathophysiology. Although some publications advocate that the cause of LE is overuse trauma [3, 6, 12], recent publications do not confirm this understanding. New studies show that the main pathophysiological hallmark of tendinopathy is neovascularity and disorganized collagen fibers. However, the cause of the degenerative changes and pain is unclear. Mechanical, neural, and vascular problems and healing failure are blamed for the pathophysiology of LE [5, 10, 13].
Finally, the treatment in LE is also controversial. The main treatment of LE is non-surgical and involves anti-inflammatory drugs, brace use, corticosteroid and/or local anesthetic injection, and extracorporeal shock wave therapy [3, 5, 6, 10]. However, these methods have not been shown to be more effective in the long-term than watchful waiting [13,14,15,16]. When non-surgical methods are not effective, invasive techniques, such as dry needling, platelet-rich plasma injections, and surgical intervention, are an option [10]. However, the best treatment must be effective, practical, and inexpensive to enable better recovery and a rapid return to work.
Dry needling involves the insertion of thin monofilament needles without injectate into, alongside, or around nerves, muscles, or connective tissues for the management of pain and dysfunction in neuromusculoskeletal conditions [3, 17, 18]. Over the years, dry needling has become popular. However, the support for dry needling in the literature remains insufficient [4, 17, 19, 20]. Moreover, the method of dry needling is controversial [19], including where the needles should be inserted, which type of needle or how many needles should be used, how much time should be waited after inserting the needles, and how often needling should be performed.
The literature includes two trials of dry needling in LE. Stenhouse et al. compared the outcomes of dry needling with those of dry needling combined with autologous conditioned plasma injections in 28 patients who had refractory LE. They performed dry needling with a 23-gauge injector needle as a peppering technique in which the needle perforated the tendon 40–50 times within about two minutes [3]. Mishra et al. recruited 225 refractory LE patients to compare the outcomes of platelet-rich plasma and dry needling. They applied dry needling as a peppering technique in which a 10-L injector needle penetrated the tendon five times [10]. Both studies reported that the outcome of autologous blood injection techniques was not significantly superior to that of dry needling [3, 10]. Our study differed from these two in the style of needling, the exclusion of refractory cases, and the use of dry needling in the study group (rather than in a control group). The previous studies used thick needles, whereas we used thin ones because we think that thin needles reflect dry needling better. Our study is unique in the literature as it investigated the effectiveness of the real dry needling. Therefore, we had to start our investigations about dry needling by comparing the results of dry needling with first line treatments. Since we demonstrated the effectiveness of this approach, subsequent studies should compare second-line treatments, such as corticosteroid or platelet-rich plasma techniques, with dry needling. Another essential difference from other studies is that, to avoid the effects of the previous interventions on our results, we did not enroll refractory cases.
Dry needling procedures can involve remote needling and needling at trigger points [21,22,23]. We considered the trigger point of LE to be the most painful area in that region and inserted the needles there (Fig. 1). Deep dry needling was performed, and the needles were rotated three to four times after penetration. Mouse studies have shown that the manipulation techniques used when performing dry needling have different effects. Langevin et al. indicated that rotational needle manipulation leads to significantly greater fibroblastic activity in tendons [24].
Although the exact mechanism by which dry needling works is not clear, it has been suggested that this technique reduces peripheral and central sensitization [17, 18, 20, 23], which positively influences tendon healing due to increasing blood flow via local vasodilatation and collagen proliferation [7, 17, 18]. Therefore, it may be possible to restore the range of motion and reduce the local and widespread pain of LE patients.
Dry needling is generally safe. Reported complications of dry needling include soreness at the needling area, syncope responses, and local haemorrhage [4]. We encountered only one patient who had local haemorrhage. After the second intervention, she had to be excluded from the study.
We hypothesized that dry needling would be as effective as first-line treatment. Based on the before and after-treatment comparison of the PRTEE (pain and functional) scores, the dry needling group showed significant recovery at both three weeks and six months. We did not examine all the patients with ultrasonography. However, ultrasonographic images of a few patients indicated that radiological recovery of the tendon is possible with dry needling (Fig. 2). Whereas, the first-line treatment was effective at three weeks, it lost its efficacy, and the PRTEE scores of the patients increased at six months. Therefore, dry needling was significantly more effective than the first-line treatment of LE (Tables 1 and 2).
One limitation of this study was the relatively small patient group, which was primarily the result of the difficulty of convincing patients to adhere to the study protocol. One-fourth of the patients in the control group had to be excluded from the study because they used other treatment methods. A second limitation is the standardization of dry needling. Although we found successful results for dry needling, outcomes may change as a function of the technique used.
Further investigations with larger groups are needed to compare dry needling in LE. Ultrasonographic follow-up could be performed in every patient. We also believe that dry needling would be an effective treatment option in other tendinopathies.
Conclusion
Dry needling is a safe, effective treatment method for LE. Comparative studies should be conducted to compare dry needling with other treatment modalities.
References
Dwyer AJ, Govindaswamy R, Elbouni T, Chambler AF (2010) Are "knife and fork" good enough for day case surgery of resistant tennis elbow? Int Orthop 34:57–61
Okçu G, Erkan S, Sentürk M, Ozalp RT, Yercan HS (2012) Evaluation of injection techniques in the treatment of lateral epicondylitis: a prospective randomized clinical trial. Acta Orthop Traumatol Turc 46:26–29
Stenhouse G, Sookur P, Watson M (2013) Do blood growth factors offer additional benefit in refractory lateral epicondylitis? A prospective, randomized pilot trial of dry needling as a stand-alone procedure versus dry needling and autologous conditioned plasma. Skelet Radiol 42:1515–1520
Kalichman L, Vulfsons S (2010) Dry needling in the management of musculoskeletal pain. J Am Board Fam Med 23:640–646. doi:10.3122/jabfm.2010.05.090296
Krey D, Borchers J, McCamey K (2015) Tendon needling for treatment of tendinopathy: a systematic review. Phys Sportsmed 43:80–86. doi:10.1080/00913847.2015.1004296
Ozkut AT, Kilinçoğlu V, Ozkan NK, Eren A, Ertaş M (2007) Extracorporeal shock wave therapy in patients with lateral epicondylitis. Acta Orthop Traumatol Turc 41:207–210
Tsikopoulos K, Tsikopoulos I, Simeonidis E, Papathanasiou E, Haidich AB, Anastasopoulos N, Natsis K (2016) The clinical impact of platelet-rich plasma on tendinopathy compared to placebo or dry needling injections: a meta-analysis. Phys Ther Sport 17:87–94
Ozden AV, Alptekin HK, Esmaeilzadeh S, Cihan C, Aki S, Aksoy C, Oncu J (2016) Evaluation of the sympathetic skin response to the dry needling treatment in female myofascial pain syndrome patients. J Clin Med Res 8:513–518. doi:10.14740/jocmr2589w
Saylor-Pavkovich E (2016) Strength exercises combined with dry needling with electrical stimulation improve pain and function in patients with chronic rotator cuff tendinopathy: a retrospective case series. Int J Sports Phys Ther 11:409–422
Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, Ramsey ML, Karli DC, Rettig AC (2014) Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med 42:463–471. doi:10.1177/0363546513494359
Urbaniak GC, Plouse S. Research randomizer (version 4.0). Available at: https://www.randomizer.org. Accessed 23 Jan 2016
De Smedt T, De Jong A, Van Leemput W, Lieven D, Van Glabbeek F (2007) Lateral epicondylitis in tennis: update on aetiology, biomechanics and treatment. Br J Sports Med 41:816–819
Rabago D, Best TM, Zgierska AE, Zeisig E, Ryan M, Crane D (2009) A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med 43:471–481
Hong QN, Durand MJ, Loisel P (2004) Treatment of lateral epicondylitis: where is the evidence? Joint Bone Spine 71:369–373
Rothschild B (2013) Mechanical solution for a mechanical problem: tennis elbow. World J Orthop 18:103–106
Sayegh ET, Strauch RJ (2015) Does nonsurgical treatment improve longitudinal outcomes of lateral epicondylitis over no treatment? A meta-analysis. Clin Orthop Relat Res 473:1093–1107
Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M (2013) Physiologic effects of dry needling. Curr Pain Headache Rep 17:348. doi:10.1007/s11916-013-0348-5
Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T (2014) Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev 19:252–265
Cox J, Varatharajan S, Côté P et al (2016) Effectiveness of acupuncture therapies to manage musculoskeletal disorders of the extremities: a systematic review. J Orthop Sports Phys Ther 46:409–429. doi:10.2519/jospt.2016.6270
Dommerholt J (2011) Dry needling-peripheral and central considerations. J Man Manip Ther 19:223–227. doi:10.1179/106698111X13129729552065
Tekin L, Akarsu S, Durmuş O, Cakar E, Dinçer U, Kıralp MZ (2013) The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo-controlled trial. Clin Rheumatol 32:309–315. doi:10.1007/s10067-012-2112-3
Eftekharsadat B, Babaei-Ghazani A, Zeinolabedinzadeh V (2016) Dry needling in patients with chronic heel pain due to plantar fasciitis: a single-blinded randomized clinical trial. Med J Islam Repub Iran 30:401
Ziaeifar M, Arab AM, Karimi N, Nourbakhsh MR (2014) The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther 18:298–305. doi:10.1016/j.jbmt.2013.11.004
Langevin HM, Bouffard NA, Churchill DL, Badger GJ (2007) Connective tissue fibroblast response to acupuncture: dose-dependent effect of bidirectional needle rotation. J Altern Complement Med 13:355–360
Acknowledgements
The study was carried out in İstanbul Medeniyet University Göztepe Training and Research Hospital Orthopedics and Traumatology Department.
Funding
No funding was received for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations that might pose a conflict of interest in connection with this article.
Ethical approval
Institutional Review Board approval was obtained (from İstanbul Medeniyet University Göztepe Training and Research Hospital No: 2016/0199) for the study.
Rights and permissions
About this article
Cite this article
UYGUR, E., AKTAŞ, B., ÖZKUT, A. et al. Dry needling in lateral epicondylitis: a prospective controlled study. International Orthopaedics (SICOT) 41, 2321–2325 (2017). https://doi.org/10.1007/s00264-017-3604-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3604-1