Abstract
Purpose
To evaluate the efficacy and safety of a posterior-only approach for L5 corpectomy, with lumbopelvic fixation for treatment of secondaries, infections, or burst fractures.
Methods
Between 2010 and 2013, 17 patients with L5 pathology had corpectomy through a posterior-only approach, with reconstruction of the anterior column using titanium cages filled with bone graft. The indication for surgery was presence of secondaries in nine patients, spondylitis and spondylodiscitis in five patients and burst fractures due to high energy trauma in three patients. All patients underwent detailed neurological examination as well as plain radiography, computed tomography, and magnetic resonance imaging studies.
Results
This study included 17 patients (8 males and 9 females) with a mean age of 48.3 years. The mean operative time was 186.1 minutes with mean blood loss of 744 ml. No intra-operative or immediate post-operative complications were encountered. Three patients died during follow-up due to advanced malignancy. The remaining 14 patients were followed-up for a mean of 24.9 months. One patient had cut through of L3 screws two years after surgery requiring metal removal. One patient had asymptomatic broken screw, with no need for further intervention.
Conclusions
L5 corpectomy is a challenging procedure indicated for treatment of various cases of metastasis, infections, or comminuted fractures. The posterior approach is safe, efficient, and allows both rigid posterior stabilization and anterior reconstruction after L5 corpectomy without the need for an anterior approach and its possible related morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The fifth lumbar vertebra is the largest vertebra in the human vertebral column and it has specific anatomical and biomechanical properties [1]. Corpectomy of L5 for treatment of tumours, infections or trauma is a challenging procedure and is usually done through combined anterior and posterior approaches with high morbidity, long hospital stay, and a long rehabilitation period [1,2,3,4].
Few reports describing L5 corpectomy using a posterior only approach exist in the literature, most of them are case reports [5, 6]. Posterior-only L5 corpectomy avoids possible morbidities associated with a combined approach, with much less operative time and faster patient rehabilitation.
The aim of this prospectively followed case series was to document the safety and efficacy of L5 corpectomy with titanium cage reconstruction through the posterior only approach for treatment of various pathologies involving the fifth lumbar vertebra. To the best of our knowledge, this is the first prospective case series describing L5 corpectomy through a posterior-only approach.
Patients and methods
Between 2010 and 2013, all patients with L5 pathology requiring corpectomy were operated on through the posterior-only approach for pedicle-screw fixation and L5 corpectomy with reconstruction of the anterior column by titanium mesh or expandable cage filled with bone graft. This included patients with secondaries, infections or burst fractures of L5 vertebra. All patients underwent thorough physical and neurological examination. Plain radiography, computed tomography (CT) scan and magnetic resonance imaging (MRI) studies of the lumbosacral spine were performed for all patients. The indications for surgery were intractable back pain, radicular pain, or neurological deficits. All patients signed an informed consent to be included in this case series.
The operative technique started with positioning of the patient in the prone position over a radiolucent table. Standard midline posterior approach was done exposing the posterior elements of the operated upon region of the spine. Pedicle screws were inserted in the standard technique [7] and their position was checked by intraoperative radiograph. In the first two cases, single-level fixation from L4 to S1 was used. However, after that two-level fixation extending from L3 to the pelvis using iliac screws was routinely used for more rigid fixation. One patient needed fixation from L1 to the pelvis due to combined fractures of L2 and L5.
A temporary rod was inserted after that on the non-operating side depending on the pathology. Laminectomy was done with unilateral facetectomy; thus exposing both the exiting and traversing nerve roots, and exposing L4–5 and L5-S1 disc spaces.
After complete discectomy of both L4–5 and L5-S1, corpectomy was started by excision of the pedicle and the adjacent parts of the body through the window between the exiting and the traversing nerve roots, while protecting them and the dura using nerve root retractors. Corpectomy was continued using bone curettes, spine osteotomes, Kerrison rongeurs and bone nibblers. If complete corpectomy was planned as in tumor cases, the temporary rod was changed to the other side and the procedure was repeated on the opposite side, removing the other facet joint, pedicle and the remaining parts of the body.
For insertion of the cage, L4 and L5 nerve roots were gently retracted using nerve-root retractors. Then a suitable cage filled with bone graft was slid downward and obliquely above the L5 nerve root until it reached the end plate of S1. The cage was finally pushed forward and straightened under L5 end plate (Fig. 1). Controlled compression through the pedicle screws secured the position of the cage between the two bony end plates and its position was checked by intraoperative radiograph. Finally, the other rod was inserted and the wound was closed in layers over a suction drain (Fig. 2).
Illustration of the operative steps: a Insertion of pedicle screws and a rod on one side. b Laminectomy and facetectomy exposing both the exiting and traversing nerve roots. c Excision of the pedicle, body, L4/5 and L5/S1 discs creating enough space for cage insertion. d Protection of L4 and L5 nerve roots using nerve root retractor. e Insertion of the cage filled with bone chips obliquely above L5 nerve root. f Sliding the cage until it rests on the S1 end plate. g The cage is pushed anteriorly and straighten. h Adjustment of the cage position between the end plates. i Insertion of the other rod with gentle compression to secure the cage position
The excised body was sent for histopathological examination in cases with tumors and for microbiological examination in cases with infection. Broad-spectrum antibiotic therapy was started after surgery for three days. In cases of infections, it was changed according to the culture and sensitivity results. All patients were allowed weight-bearing as early as tolerated without a brace. As per our standard procedures, post-operative radiographs were taken on the second day after surgery (Fig. 3). All patients were discharged within one week after surgery unless otherwise indicated. Standard follow-up visits were done post-operatively at two weeks, two months, six months, 12 months, and then every year. Post-operative adjuvant chemotherapy or radiotherapy for cases with tumour was delayed until there was complete wound healing.
A 47-year-old woman with history of previous mastectomy for breast cancer two years ago. a Pre-operative CT and MRI showing L5 metastasis causing pathological fracture. b Post-operative AP and lateral plain X-rays after L5 corpectomy and reconstruction using titanium mesh cage with fixation from L3 to the pelvis using iliac screws. c One-year follow-up CT scan with stable construct
The operative time, operative blood loss and changes in neurological status were documented for all patients. Fusion was assessed on plain X-rays by bridging bone between the end plates without lucencies in between. However, the presence of metal cage may mask the bridging bone inside, and the stability of the construct was judged by absence of any change in cage position on serial follow-up images. CT or MRI was done during the follow-up period if needed.
Results
This study included 17 patients (eight males, nine females) with a mean age of 48.3 years (range, 16–67 years). Nine patients had metastasis of L5 (five breast cancer, two renal carcinoma, one thyroid carcinoma and one lung carcinoma), five patients had spondylodiscitis, and three patients had burst fractures due to high energy trauma.
Pre-operative neurological examination revealed weak extensor hallucis longus in one patient with L5 metastasis, with full recovery 1 month after surgery. One patient with burst fracture had cauda equina syndrome pre-operatively with improvement of the sphincteric function and sensation after surgery, but with residual foot drop requiring tendon transfer one year after surgery (Fig. 4). No neurological deterioration occurred after surgery.
A 22-year-old man presented to the emergency department after a fall from 10 m height. a Pre-operative CT scan showing burst fracture of L5 with marked canal compromise together with compression fracture of L2. b Postoperative AP and lateral plain X-rays after L5 corpectomy and reconstruction using titanium mesh cage with fixation from L1 to the pelvis using iliac screws. c One-year follow-up AP and lateral X-rays showing healing of L2 facture and solid L4/S1 fusion. d Lateral view after removal of L1, L2, L3 and iliac screws. e One-year follow-up CT scan after removal of screws, with bridging bone inside the cage
The mean operative time was 186.1 min (range, 164–225 min). The mean operative blood loss was 744 ml (range, 400–1,100). No intra-operative or immediate post-operative complications were encountered in this study.
Three patients with L5 metastasis died during the follow-up due to advanced malignancy. The remaining 14 patients were followed-up for a mean of 24.9 month (range, 14–38 month).
Radiological evaluation revealed stable implants in 12 out of the surviving 14 patients until the last follow-up. One patient, 16 years old with L5 burst fracture and single level fixation had a broken S1 screw after one year, but was without symptoms or change in cage position. Radiological examination showed bridging bone across the cage (Fig. 5). This patient was followed for two years and did not need any further intervention. Actually, this patient was the first one in this series, after which the surgical procedure was changed to double-level fixation from L3 to the pelvis for more secure fixation.
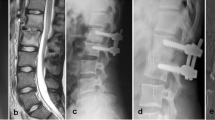
A 16-year-old girl presented to the emergency department after a motor vehicle accident. a Pre-operative CT scan showing burst fracture of L5 with canal compromise. b Postoperative AP and lateral plain X-rays and CT scan after L5 corpectomy and reconstruction using expandable titanium cage with L4 to S1 pedicle screws fixation. c One-year follow-up CT scan showing stable cage position with one broken S1 screw. d Three-year post-operative CT scan with solid L4 to S1 fusion without change in the position of the cage or the broken screw
Another patient with L5 corpectomy done for infection developed cut-through of L3 screws two years after surgery and after complete bony union across L4-S1. He was treated by removal of the screws and was followed-up for one year after that, without further intervention (Fig. 6).
A 33-year-old man. a Pre-operative MRI showing L4–5 spondylodiscitis with marked destruction of L5. b Post-operative AP and lateral plain X- rays after L5 corpectomy and reconstruction using titanium mesh cage with L3 to ilium fixation. c Two-year follow-up X-rays showing cut-through of L3 screws but with stable cage and bridging bone through L4-S1. So, only metal removal of the L3 and iliac screws was done
Discussion
The lumbosacral junction has specific anatomical and biomechanical properties and constitutes a challenge for spine surgeons [8]. Diseases affecting the three columns of the L5 vertebra, such as trauma, tumour, or infection, usually require L5 corpectomy with reconstruction of the resulting defect by cages to support the anterior column [9], together with posterior stabilization in order to tolerate the maximal loads of the spine at this level.
Most reports in the literature on L5 corpectomy combine a posterior approach either open or percutaneously for posterior instrumentation together with an anterior approach for corpectomy and reconstruction of the anterior column [1, 3, 4]. This combined approach is usually associated with high morbidity, long operative time, more blood loss, and long hospital stay and rehabilitation period [6]. Moreover, the anterior approach to L5 has a particular risk due to the bifurcation of the common iliac vessels in front of it, and subjecting them to injury during an anterior approach that may result in catastrophic complication [10].
In this study, a single approach was done to achieve posterior rigid stabilization, 360° neural decompression if needed and perfect anterior column reconstruction without exposing the patient for the morbidity of the combined approaches or the possible vascular complication of an anterior surgery. The technique of inserting a mesh cage filled with bone chips after a single- or double-level posterior corpectomy for tuberculosis of the lumbar spine has been described in a previous publication, without reported nerve root injuries [11]. Gentle manipulation of the cage between the nerve roots allows proper insertion without significant traction on the nerve roots.
On the other hand, insertion of the cage after L5 corpectomy through an anterior approach is not always an easy job due to the limitation of space by the vascular anatomy. Many authors reported on extending the corpectomy to L4 or S1 to overcome this limitation; despite that, the pathology was limited to L5 [12, 13].
Dai et al. [14] reported on anterior-only corpectomy and instrumentation of L5 for treatment of non-traumatic cases. However, their patients were kept in bed for one month post-operatively due to less rigid fixation. In this series, all patients were allowed to ambulate as early as tolerated due to rigid fixation. This provided both physical and psychological advantages for the patients and avoided prolonged recumbency and its hazards.
Shousha et al. [1] reported three technical difficulties during L5 corpectomy. Firstly, as mentioned above, the complex vascular anatomy with the bifurcation of the common iliac vessels in front of L5 and the possibility of injuring them. A posterior-only approach avoids this complication.
The second technical difficulty was that the lumbosacral junction is a transition zone between the mobile lumbar spine and the relatively fixed sacrum subjecting the implants to higher loads and greater stress with a high rate of pseudoarthrosis [15, 16]. However, the rigid posterior fixation from L3 to the pelvis together with a strong titanium cage supporting the anterior column provides good fixation that can tolerate maximum loads over the implants until bone healing. This may explain the absence of pseudoarthrosis in this series.
The third challenge was the bony anatomy of L5 with high lordosis angle and large defect after corpectomy. In this study, a titanium mesh or expandable cage filled with bone graft was used, and this was sufficient to fill the defect after L5 corpectomy until complete bony fusion.
In this study, the average blood loss was 744 ml, which is much less than that reported in combined approaches, which reached 3.2 L in some studies [1]. Overall, the posterior approach for the lumbar spine is a simple approach that is familiar to all spine surgeons, which carries little risk for vascular or visceral injury, and minimizes recovery time.
Conclusion
L5 corpectomy is a challenging procedure indicated for treatment of tumors, infection, or comminuted fractures of L5. The posterior-only approach is safe, efficient, and provides rigid posterior stabilization, 360o neural decompression, and anterior reconstruction after L5 corpectomy without the need for the anterior approach and its possible related morbidity.
References
Shousha M, El-Saghir H, Boehm H (2014) Corpectomy of the fifth lumbar vertebra, a challenging procedure. J Spinal Disord Tech 27(6):347–351
Gallia GL, Sciubba DM, Bydon A, Suk I, Wolinsky J-P, Gokaslan ZL et al (2007) Total L-5 spondylectomy and reconstruction of the lumbosacral junction. J Neurosurg Spine 7(1):103–111
Shimada Y, Hongo M, Miyakoshi N, Kasukawa Y, Ando S, Itoi E et al (2007) Giant cell tumor of fifth lumbar vertebrae: two case reports and review of the literature. Spine J 7(4):499–505
Detwiler PW, Porter RW, Crawford NR, Apostolides PJ, Dickman CA (1999) Lumbosacral junction fixation and fusion after complete L-5 spondylectomy: case report. Neurosurg Focus 7(6):E5
Kocis J, Wendsche P, Visna P (2008) Complete burst fracture of the fifth lumbar vertebra treated by posterior surgery using expandable cage. Acta Neurochir 150(12):1301–1305
Hunt T, Shen FH, Arlet V (2006) Expandable cage placement via a posterolateral approach in lumbar spine reconstructions: technical note. J Neurosurg Spine 5(3):271–274
Roy-Camille R, Saillant G, Mazel C (1986) Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res 203:7–17
Kaner T, Oktenoglu T, Sasani M, Ozer AF (2012) L5 vertebrectomy for the surgical treatment of tumoral and traumatic lesions of L5 vertebra. Orthop Rev 4(1):10
Harms J, Tabasso G, Cinanni R (1999) Instrumented spinal surgery: principles and technique. Thieme, Stuttgart
Brau SA, Delamarter RB, Schiffman ML, Williams LA, Watkins RG (2004) Vascular injury during anterior lumbar surgery. Spine J 4(4):409–412
El-Sharkawi MM, Said GZ (2012) Instrumented circumferential fusion for tuberculosis of the dorso-lumbar spine. A single or double stage procedure? Int Orthop 36(2):315–324
Kuklo TR, Potter BK, Bell RS, Moquin RR, Rosner MK (2006) Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech 19(5):376–382
Fayazi AH, Ludwig SC, Dabbah M, Butler RB, Gelb DE (2004) Preliminary results of staged anterior debridement and reconstruction using titanium mesh cages in the treatment of thoracolumbar vertebral osteomyelitis. Spine J 4(4):388–395
Dai L-Y, Jiang L-S (2010) Anterior-only instrumentation and grafting after L5 corpectomy for non-traumatic lesions. Acta Orthop Belg 76(1):94
Lee Y-P, Ghofrani H, Regev GJ, Garfin SR (2011) A retrospective review of long anterior fusions to the sacrum. Spine J 11(4):290–294
Cunningham BW, Lewis SJ, Long J, Dmitriev AE, Linville DA, Bridwell KH (2002) Biomechanical evaluation of lumbosacral reconstruction techniques for spondylolisthesis: an in vitro porcine model. Spine 27(21):2321–2327
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no financial conflicts of interest in connection with this article.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Elnady, B., Shawky, A., Abdelrahman, H. et al. Posterior only approach for fifth lumbar corpectomy: indications and technical notes. International Orthopaedics (SICOT) 41, 2535–2541 (2017). https://doi.org/10.1007/s00264-017-3570-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3570-7