Abstract
Purpose
During tibial tubercle transfer, popliteal vessels are at risk from drills and screws. The risk is around 0.11%, as described in the literature. We reviewed knee injected CT scan for analysis of the location of arteries, identified landmarks allowing minimizing risks, and defined a safe zone.
Material and method
Distances between the posterior cortex and arteries were measured on CT scans from 30 adults (60 knees) at three levels (proximal part of the tibial tuberosity, 20 mm and 40 mm distally). Data were used to create a “risk map” with different angular sectors where the frequency of the presence of arteries was analyzed in each area. We also analyzed the position of 68 screws of 47 patients who underwent a medial tibial tuberosity transfer.
Results
The nearest distance between artery and the posterior tibial cortex was found at the level corresponding to the top of the tuberosity with less than 1 mm, while the largest distance was found at the distal level. We were able to define a safe zone for drilling through the posterior tibial cortex which allows a safe fixation for the screws. This zone corresponds to the medial third of the posterior cortex. When the safe zone is not respected, screws that overtake the posterior cortex may be close to arteries as observed for 37 of the 68 screws analyzed.
Conclusion
We described new landmarks and recommendations to avoid this complication during tibial tuberosity transfer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular injury is a rare but potentially devastating complication after orthopaedic surgery. The popliteal artery (PA) is the most concerned with 5% of injuries due to knee orthopedic surgery [1,2,3,4,5,6]. Previous studies have focused on prevention of vascular injuries during arthroplasties and osteotomies around the knee [7,8,9] but there is a paucity of literature regarding vascular risks related to interventions like drilling isolated screws for tuberosity fixation after osteotomy of the anterior tibial tuberosity (ATT) [10]. Although there is not an extensive evaluation of the risk of vascular complications during anterior tibial tuberosity fixation in the literature, popliteal artery injuries have been presented as case reports [8, 10] and Bernhoff reported an incidence of 0.11% in a group of 1831 tibial tubercle osteotomies between 1998 and 2011 [11]. With regard to the high number of procedures performed each year, the frequency is probably low and may be estimated in the same order as arthroscopy which is also a minimally invasive procedure: Small [2] reported the incidence of injury to the popliteal artery during knee arthroscopy is nine in 400,000 cases, and DeLee [1] reported this incidence to be six in 120,000 cases. Payne et al. [12], in 2015, reported in a series of 787 procedures a 4.6% overall risk of complications for osteotomy of ATT, but did not mention arterial complications, which means that the risk is probably lower than one in 1000 cases.
Although rare during arthroscopy [1,2,3,4], injury to vascular structures may occur and several studies have been conducted to localize the popliteal artery at the level of the joint line. The popliteal artery is known to be located just posterior to the posterior horn of the lateral meniscus at the joint line; however, the proximity of the vascular structures to a screw that overtakes the posterior cortex of the proximal tibia has never been characterized. We therefore sought to better quantify the risk of damage to major blood vessels from drilling or screwing around the proximal tibia and to assess qualitatively the localization of the vasculature at the level of the tibial tuberosity.
Our hypothesis was that studying the localization of the popliteal artery at the level of the tibial tuberosity in a large group of subjects might reveal the presence of anatomic variances with regard to the position of the artery at the level of the tibial tuberosity. The risk occurrence of arterial injuries reported in cases reports [8, 10, 11] during routine procedures of osteotomy of the anterior tibial tuberosity was the rationale for this suggestion.
The aims of this study were (1) to measure on CT scan of patients with three-dimensional (3D) reconstructions, the distances between the posterior cortex of the tibia and the popliteal and leg arteries; (2) to qualitatively describe the sectors where the vessels are at risk, and to establish a safe zone for screw insertion; (3) analyze the position of screws in a clinical series of patients who had had a ATT osteotomy.
Material and methods
Patients demographics
The positioning of the popliteal and leg arteries in 60 knees of 30 patients (18 men, 12 women) who had had an angio-CT scan for various indications was retrospectively analyzed. All images were obtained with the knee completely extended. Patients with a previous history of fractures, tumors or knee deformities, of surgical procedures (bone or arteries), or popliteal and leg arteries occlusions were excluded. Patients whose CT scan presented any soft-tissue or bone abnormalities in the proximal region of the tibia were also excluded. The angio-CT’s were selected, randomized, and anonymized from databases of three hospitals in Europe (HEGP – Paris France; Victor Dupouy hospital – Argenteuil France; Epicura hospital – Baudour Belgium). The patients had a median age of 50 years (range 18–77 years). Scans had to contain images from the thoracic region to the toes of the patient. The evaluation protocol used was CT acquisition reference mAs/actual 250 mAs, 120 kV, exposure time 0.5 seconds, reconstruction thickness 0.6 mm, reconstruction spacing 0.4 mm, and display field of view 170 mm. Perfusion of patients allowed adequate visualization of arteries in all knees and legs. From the two dimensional axial views, three dimensional reconstructions were made using Osirix® software (Pixmeo, Bernex, Switzerland) on a personal computer. According to the field of view (42 cm) and matrix (512 × 512) of the CT scan images, the accuracy and the reproducibility of measurements, the precisions of measures were 1 mm +/− 0,2 mm and 1 +/− 0,5 degree. The height of patients was obtained and when missing was estimated from formulas [13] according to the length of the femur measured on the CT scan.
Measurements on CT scan
The distances from the posterior tibial cortex to the popliteal and leg arteries were measured (using the 3D model of Osirix® software) at three different levels of the proximal region of the tibia (Fig. 1). The first measurement was made at the top of the ATT at the location where a most proximal screw could be inserted (level 1). The second was made 20 mm distally, at the most prominent point of the ATT, which is the most frequent location for screw drilling (level 2). The third measurement was made 40 mm distally to the top of the ATT through the anterior tibial cortex, representing the possible entry point of a distal screw fixing the ATT (level 3). The diameter of the artery was measured at each level (Fig. 1). The closest (from the posterior cortex) and most medial artery was selected for measurement. To correct the position variation of the patient in the CT scan, we used when necessary the CT scan torsion of the tibia as proposed in the literature [14, 15] by merging two pictures, one of the proximal tibia and one of the ankle cut with the two malleolus and did a reslicing process according to the tibial torsion.
Assessing the vascular risk by sector
The aim of this part of the study was to create a “risk map”. We first designed a map with three different surface areas at the posterior part of the tibia by drawing on each CT scan cut two curves parallel to the posterior border of the proximal tibia and distant by 5 mm and 10 mm (Fig. 2). We drew these curves at the three levels of the tibial tuberosity. On this map, four different angular sectors (each of 10 degrees) posterior to the proximal tibia were determined as follows: we merged two pictures of CT scan [14, 15], one of the proximal tibia and one of the ankle at the level of the two malleolus; then we draw at each level a line starting on the proximal tibia at the center of the ATT, perpendicular to the bi-malleolus line. From this medial line, we drew laterally four sectors of 10 degrees each (Fig. 2 and Video 1). Twelve different zones were therefore delimited, numbered from A to L, behind the posterior proximal tibia at each level. We evaluated the frequency of the presence of the artery in each of these 36 areas (Fig. 2a). We also reported the exact position of the popliteal artery and performed measurement of the surface of each zone to compare this area with the surface section of the artery and with the surface section of a screw. We also determined zones where the artery was never present to determine a safe zone.
We measured the theoretical distance from the ATT (entry points of the screws) to the artery using the 3D model of Osirix® software at the three different levels of the proximal region of the tibia, and analyzed the results with regard to the height of the patient to know if it was possible to predict patient risk that a too long screw overtakes the posterior cortex.
Assessing retrospectively the screw position on radiographs of patients
We retrospectively analyzed the position, orientation (axial and sagittal), and overtaking length of 68 screws on a multi-centric cohort (Epicura hospital - Baudour Belgium; Erasme hospital – Bruxelles Belgium) of 47 patients previously operated for medial ATT transfer (according to Elmslie-Trillat procedure). The screws’ orientation in the axial plane was determined by trigonometry using the measurement of the screw length projection on anterior and lateral radiographs. Knowing the screw length and measuring the distance between the head and the end of the screw, the angle of the screw with an antero-posterior axis was calculated using the following trigonometric formula: angle β = tan−1(screw length on face X-ray/screw length on profile X-ray). This angle was corrected to be reported perpendicular to the bi-malleolar line [16, 17]. Then using the direction of the screw in the axial plane and the overtaking length, the position of the distal extremity of the screws was reported on the “risk map” (Fig. 2b), using a reslicing process to merge the pictures.
Statistical analysis
Statistical analysis was performed using software XLSTAT® (Addinsoft) for Windows. The descriptive analysis presented the observed data in the form of tables, expressed using means, min and max, along with illustrative graphs. Continuous variables were angle, distances ATT-A; POST-A; height; abdominal perimeter; distance between femoral heads. A p-value <0.05 was considered significant. The inferential analysis was composed of the following methods: numerical variables were compared between pairs of sub-groups using the T-student and ANOVA tests. Linear regression was used to determine correlations between measurements.
Results
Proximity of arterial structure to posterior cortex of tibia and entry point of a screw
The first objective was to measure the distances between the artery and the posterior cortex at the three different levels of the proximal tibia. Table 1 shows the mean and confidence interval at 95% of the distances at the three levels, according to gender and age group. On average within the entire proximal tibia, the distance between the artery and the posterior tibial cortex was 12 mm [95% CI 10-13 mm]. The minimal distance was at the superior margin of the tibial tubercle where the only septal tissue is the posterior articular capsule: at this level 1, in 8.4% of the angio CT scans, the artery was very close to the bone (Fig. 3a), less than 5 mm; in one case the distance was <1 mm. The distance increased at levels 2 and 3, with the posterior tibial muscle separating the vessels from the posterior tibia. No correlation was found for age, gender, and obesity.
a This picture illustrates the presence of an anterior tibial artery attached to the posterior cortex of the tibia (Level 1). b Example of screw overtaking the posterior cortex in a zone at risk (presence of the artery). The artery presence frequency in this zone is 11.7%. c Schematic representation in a zone of a screw of 4 mm and of an artery (real proportions)
Qualitative analysis of angular sectors at risk
Figure 2 provides the frequency with which the artery traversed each zone (Fig. 2a). When considering the vascular risks of a screw, the risk in each zone depends on the cross-section areas of the zone itself, of the artery and of the screw. For the surface of each zone, we considered that in each row (for example the row situated at a distance less than 5 mm from the posterior cortex, with zones A, B, C, D), the surface was similar (within 4 mm2). The surface of each zone indicated in Table 3 was on average 0.45 cm2 (range 0.34 to 0.52cm2). The cross-section area of the artery is reported in Tables 2 and 3: 0.13 cm2 at levels 1 and 2, but only 0.07 cm2 at level 3. The cross-section area of a screw of 4 mm diameter is also 0.13 cm2. This means that at level 1 and 2 (Fig. 3b and c), when the artery and a screw of 4 mm diameter are in the same zone, the sum of their cross-section areas (0.26 cm2) is about 50% of the surface of the zone (0.45 cm2). We observed that it was rare to find the artery posterior to the superio-medial aspect of the posterior tibial cortex. This is the safe zone, at each level. This zone corresponds approximately to the medial third of the surface at each level and is represented in Fig. 4 in green. A video constructed using Osirix® software and Sketchup® (Google, Mountain View, Californie USA) and Movavi video editor® softwares (Movavi, Saint Louis, Missouri, USA) is made available to the reader, showing the risk map in three dimensions (Video 1).
Three-dimensional reconstruction of the posterior part of proximal tibia. a and b example of arteries path c and d representation of the 3D safe map (arteries were never observed in these areas) according to our results. In green a safe zone acceptable to drill or screw, in orange a zone were arteries have never been observed but too thick to drill or screw safely
Assessing screw position on radiographs of patients after surgery
We analyzed the position of 68 screws in 47 patients: 11 patients had two ATT screws, three patients had bilateral surgery with one screw in each side, and one had two screws in each side. Among these 68 screws, 25 had overtaken the posterior cortex at level 1, 32 at level 2, and 11 at level 3. Screws had overtaken the posterior cortex of the tibia with a mean value of 5.4 mm (range 1 to 13 mm). When the position of the extremity of the screw was reported on the map risk (Figs. 2b and 3b), the risk of iatrogenic vascular lesion could be assessed. We considered that the risk was high when there was less than 5 mm between the screw and the artery, and when the screw and the artery were in the same zone (Fig. 3c). At level 1, 32% of the screws had high (> 40%) cumulated frequency (sum of frequencies of presence of arteries in each areas among the path of each screw) of presence of artery among their path, 36% of screws had medium (between 20% and 40%) cumulated frequency of presence of artery among their path, 23% had low (<20%) cumulated frequency of presence of artery among their path, and 9% had a null frequency of presence of artery among their path. At level 2, percentages of screws were 26% (high), 34% (medium), 3%(low), and 37% (null). At level 3, percentages of screws were 10% (high), 0% (medium), 30% (low), and 60% (null). All in all, only six screws were in a totally safe zone. When checking screws that are at risk to overlap the posterior cortex, we found that there was a correlation between the height of the patient and the distance from the ATT to the artery (Fig. 5). However, there was no correlation between the height of the patient and the distance from the posterior cortex to the artery. This means that when the height of the patient increases, the surgeon needs to increase the length of the screw for bi-cortical fixation, but the risk remains the same since the distance from the posterior cortex to the vessel does not increase with size of the patient.
The three diagrams at the top of the picture represent the regression curves illustrating the correlation at each level between the height (H) of the patient in centimeters and the distance D in cm from the tibial tuberosity to the popliteal artery. The three diagrams in the lower part of the picture represent the regression curves illustrating the correlation at each level between the height (H) of the patient in centimeters and the distance d in cm from the posterior cortex to the popliteal artery
Discussion
Characterizing the vascular pattern around the knee from the perspective of fixation of the ATT with screws is important when considering potential complications. The risk of vascular complications during anterior tibial tuberosity fixation has mostly been reported as case reports [8, 10], and the frequency is approximately 0.11% [11]. However, we confirm in this study the close proximity of the artery to the posterior cortex with risk of arterial injury, as the vessels, on the opposite side of the surgical field, cannot be seen and protected during the procedure. The popliteal artery and leg arteries are the most anterior structures of the posterior region of the knee. To decrease the risk of vascular complications during screw drilling and placement, we found that the danger zone is located slightly laterally to the intercondylar fossa.
Our findings are similar to those published in the literature even if measurements were done with different landmarks and different techniques. Matava [18] analyzed 14 cadavers and showed that the popliteal artery was located posteriorly and laterally to the insertion of the PCL in all knees, in extension. Keser [19] as well reported that at knee joint level, the popliteal artery was located posteriorly to the insertion of the PCL. This location may cause injury to the popliteal artery in the case of repair or excision of the posterior corn of the lateral meniscus, and also in procedures for PCL reconstruction [20, 21]. Ahn [22] using angiography measured the distance between the tibial insertion of the PCL and the popliteal artery and found that the distance from the midpoint of the PCL to the popliteal artery was 4.4 ± 3.2 mm.
Fortunately, the number of vascular injuries reported in the literature during knee arthroplasty, arthroscopy or osteotomy is small, regarding the theoretical risks based on anatomical studies. Small [2, 3] reported 12 cases of vascular injuries, representing 0.54% of all complications in the case series. There were nine cases of direct trauma to the popliteal artery, one displacement of the fibrous arcade and two nonspecific injuries. Tawes [4] reported three cases in which the popliteal artery was injured during arthroscopic meniscectomy; the diagnosis was late and the lesion led to amputation. More than 50% of the patients with injuries to the popliteal artery present deficient circulation, despite palpable distal pulses. Although rare, injury to the popliteal artery during proximal osteotomy of the tibia at the level of the ATT may have devastating consequences. When fixing the osteotomy, the screw(s) violate the posterior tibial cortex, with risk of injury to the popliteal artery [23]. Only a few studies in the literature have discussed this risk [10]. Due to the fear of vascular injury, many surgeons are very careful and stop drilling when they feel the second cortex. This is safe; however, the strength of uni-cortical fixation has been shown to be inferior to bi-cortical fixation. Our results show that it is rare to find the artery directly posterior to the supero-medial aspect of the posterior tibial cortex. It is therefore safe to drill medially. One zone seems completely safe: it is located posterior to the medial third of the tibia. According to our sectors, the artery position is especially predictable at level 2 than at levels 1 and 3. Therefore, if the tuberosity is fixed with only one screw, the safety zone is at level 2 (2 cm under the top of ATT), perpendicular to the tibial crest (not up, not down) and in a direction perpendicular to the bi-malleolus line. If the screw is oriented in this direction (+/− 10° of error), it will always avoid the artery. If the drill is oriented externally perpendicular to the bi-malleolus line, level 2 is the only zone to offer safety until 20° external deviation. At levels 3 and 1 the safety zones are also a sector centered on the line perpendicular to the bi-malleolus line (+/− 10°), but the safe area is not as large (Fig. 2). To decrease vascular complications to the popliteal artery during drilling and screwing, different knee positions have been recommended based on the translation of the vessels during flexion and extension. In our study, all CT scans were performed with the knee in extension. However, since flexion knee is known to move the artery away from bone [24], knee flexion can be recommended when possible.
We recognize the limitations of our study. The screws’ orientation in the axial plane was determined on anterior and lateral radiographs; so the risk assessment of screw placement is only done from 2-D radiographs without known artery position on a CT scan. The small sample size of each group (men and women) may have led to a type II error and inability to detect a difference between the two groups. The average age of the patients in our study was substantially older than patients usually undergoing transposition of the ATT. Even if we excluded severely arthritic knees, the age of the specimens may have led to the inclusion of knees with low grade osteoarthritis, which may have affected the results of our study because the relationship between the proximal tibia and artery can differ in arthritic knees; the artery has a more tortuous course in the popliteal fossa with increasing age and posterior osteophytes might distort the position of the vessels in arthritic knees. However, this difference is reported to be minimal (1 mm) and its clinical implications questionable [25]. Therefore, the age of the patients and the inclusion of knees with low-grade osteoarthritis did not bias the results of our study. These limitations are balanced by the strengths of our study: distances between cortex and vessels were measured on 3D models with CT scan sections, allowing for determination of the shortest possible distance. However, variations in branching patterns of the popliteal artery are not uncommon (10%–15% of cases) and several variations have been reported, the most common being a high division, and hypoplastic or aplastic posterior tibial artery, but their implication in screw drilling and placement around the knee have rarely been described. The surgeon also should be aware of these variations and their prevalence to limit the risk of injury while drilling screws. We found no case in our series with a medially localized artery. However, medial localization occurs in the popliteal artery entrapment syndrome, associated with an anomalous medial head of the gastrocnemius muscle [26]. Also, a Baker’s cyst (no case in our study) may change the localization of the popliteal artery. In our series, no knee instability was present. Popliteal artery localization might be expected to be altered in cases of rotatory or combined knee instability, because the tibial plateau shifts abnormally in relation to the femur in these cases.
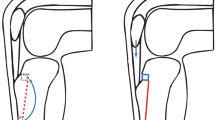
When assessing the position of the screws, patients have been treated with the Elmslie-Trillat technique and a medial transposition [27,28,29]; because the plane of the osteotomy is strictly coronal, from a theoretical point of view the surgeon will have the tendency to give a direction of the screw toward the sector at risk when the medial transposition is important (Fig. 6). However, the risk may be different according to each technique of osteotomy: the Hauser procedure [30] is a more aggressive technique, with medial and posterior transfer of the ATT, the screw directed toward the sector at risk (Fig. 6). The Fulkerson [31, 32] procedure appears less risky regarding the direction of the screw (Fig. 6). Many factors [33, 34] such as the surgical position of the operated leg may influence the surgeon.
Figure 7 showed the different positions of the leg that allow applying our results (Fig. 7). Usually in surgery of the lower limb, all the operated limb is in the operative field, then malleoli can be easily palpated and spotted by the thumb-index clamp of the surgeon. Thereby, the bi-malleolus line can be oriented as the surgeon wishes. If ATT is not totally disrupted, the knee can be flexed. We then recommend when the foot is in neutral position, that the surgeon drills oriented perpendicular to the tibial crest and internally. If the foot is oriented internally (bi-malleolus line facing the surgeon), then the surgeon has to drill right in front of him and perpendicular to the tibial crest. If the ATT is totally disrupted, then the knee must be in extension. If the foot is in neutral position then the surgeon has to drill and screw oriented vertically and internally. If the foot is oriented internally (bi-malleolus line horizontal), then the surgeon can drill and screw vertically.
Conclusion
Screw for fixation of the anterior tibial tuberosity is at risk for posterior artery lesions. We proposed landmarks allowing safety zone identification: the entry point of the screw should be at 2 cm under the proximal part of the tuberosity and oriented perpendicular to the bi-malleolus line. If this safe zone cannot be reached, some precautions allow reducing the risk: drill stop, planning to get a mono-cortical fixation, and position the knee in flexion. According to the fact that CT scan (or MRI) is frequently performed before knee surgery, we also recommend assessing the position of the artery on the images to diagnose potential abnormities.
References
DeLee J (1985) Complications of arthroscopy and arthroscopic surgery: results of a national survey. Committee on Complications of Arthroscopy Association of North America. Arthroscopy 1:214–220
Small NC (1986) Complications in arthroscopy: the knee and other joints. Committee on Complications of the Arthroscopy Association of North America. Arthroscopy 2:253–258
Small NC (1990) Complications in arthroscopic meniscal surgery. Clin Sports Med 9:609–617
Tawes RL, Etheredge SN, Webb RL et al (1988) Popliteal artery injury complicating arthroscopic menisectomy. Am J Surg 156:136–138
Bellemans J, Stockx L, Peerlinck K et al (1999) Arterial occlusion and thrombus aspiration after total knee arthroplasty. Clin Orthop Relat Res 336:164–168
Calligaro KD, DeLaurentis DA, Booth RE et al (1994) Acute arterial thrombosis associated with total knee arthroplasty. J Vasc Surg 20:927–930
Rand JA (1987) Vascular complications of total knee arthroplasty. Report of three cases. J Arthroplasty 2:89–93
Rubens F, Wellington JL, Bouchard AG (1990) Popliteal artery injury after tibial osteotomy: report of two cases. Can J Surg 33:294–297
Zaidi SH, Cobb AG, Bentley G (1995) Danger to the popliteal artery in high tibial osteotomy. J Bone Joint Surg Br 77:384–386
Kline AJ, Gonzales J, Beach WR, Miller MD (2006) Vascular risk associated with bicortical tibial drilling during anteromedial tibial tubercle transfer. Am J Orthop (Belle Mead NJ) 35:30–32
Bernhoff K, Björck M (2015) Iatrogenic popliteal artery injury in non arthroplasty knee surgery. Bone Joint J 97–B:192–196. doi:10.1302/0301-620X.97B2.34353
Payne J, Rimmke N, Schmitt LC et al (2015) The incidence of complications of Tibial tubercle osteotomy: a systematic review. Arthroscopy 31:1819–1825. doi:10.1016/j.arthro.2015.03.028
Trotter M (1970) Estimation of stature from intact limb bones. In: Stewart TD (ed) Personal identification in mass disasters. National Museum of Natural History, Smithsonian Institution, Washington, pp 71–84
Eckhoff DG, Johnson KK (1994) Three-dimensional computed tomography reconstruction of tibial torsion. Clin Orthop Relat Res 302:42–6
Akagi M, Oh M, Nonaka T et al (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Tamari K, Tinley P, Briffa K, Breidahl W (2005) Validity and reliability of existing and modified clinical methods of measuring femoral and tibiofibular torsion in healthy subjects: use of different reference axes may improve reliability. Clin Anat 18:46–55. doi:10.1002/ca.20050
Tamari K, Tinley P, Briffa K, Aoyagi K (2006) Ethnic, gender, and age related differences in femorotibial angle, femoral antetorsion, and tibiofibular torsion: cross-sectional study among healthy Japanese and Australian Caucasians. Clin Anat 19:59–67. doi:10.1002/ca.20170
Matava MJ, Sethi NS, Totty WG (2000) Proximity of the posterior cruciate ligament insertion to the popliteal artery as a function of the knee flexion angle: implications for posterior cruciate ligament reconstruction. Arthroscopy 16:796–804
Keser S, Savranlar A, Bayar A et al (2006) Anatomic localization of the popliteal artery at the level of the knee joint: a magnetic resonance imaging study. Arthroscopy 22:656–659. doi:10.1016/j.arthro.2006.04.076
Audenaert E, Vuylsteke M, Lissens P et al (2003) Pseudoaneurysm complicating knee arthroscopy. A case report. Acta Orthop Belg 69:382–384
Verdonk PCM, Demurie A, Almqvist KF et al (2006) Transplantation of viable meniscal allograft. JBJS Essent Surg Tech os 88:109–118. doi:10.2106/JBJS.E.00875
Ahn J-H, Ha CW (2000) Posterior trans-septal portal for arthroscopic surgery of the knee joint. Arthrosc J Arthrosc Relat Surg 16:774–779. doi:10.1053/jars.2000.7681
Janssen RPA, Scheltinga MRM, Sala HAGM (2004) Pseudoaneurysm of the popliteal artery after anterior cruciate ligament reconstruction with bicortical tibial screw fixation. Arthroscopy 20:E4–E6. doi:10.1016/j.arthro.2003.11.025
Cuéllar A, Cuéllar R, Cuéllar A et al (2015) The effect of knee flexion angle on the neurovascular safety of all-inside lateral meniscus repair: a cadaveric study. Arthroscopy 31:2138–2144. doi:10.1016/j.arthro.2015.04.100
Wensing PJ, Scholten FG, Buijs PC, et al (1995) Arterial tortuosity in the femoropopliteal region during knee flexion: a magnetic resonance angiographic study. J Anat 187:133–9
Rich NM, Collins GJ, McDonald PT et al (1979) Popliteal vascular entrapment. Its increasing interest. Arch Surg 114:1377–1384
Trillat A, Dejour H, Couette A (1964) Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot 50:813–824
Caton JH, Dejour D (2010) Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop 34:305–309. doi:10.1007/s00264-009-0929-4
Lane J, Karnatzikos G, Gobbi A (2014) Elmslie-Trillat procedure: a distal-based procedure for patellar stabilization. In: Gobbi A, Espregueira Mendes J, Nakamura N (eds) Patellofemoral Jt. State art Eval. Manag. Springer, New York, pp 155–160
Hauser E (1938) Total tendon transplant for slipping patella: a new operation for recurrent dislocation of the patella. Surg Gynecol Obs 66:199–214
Fulkerson JP (1983) Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res 177:176–81
Fulkerson JP, Becker GJ, Meaney JA et al (1990) Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med 18:490–496
Servien E, Verdonk PC, Neyret P (2007) Tibial tuberosity transfer for episodic patellar dislocation. Sports Med Arthrosc 15:61–67. doi:10.1097/JSA.0b013e3180479464
Koëter S, Diks MJF, Anderson PG, Wymenga AB (2007) A modified tibial tubercle osteotomy for patellar maltracking: results at two years. J Bone Joint Surg Br 89:180–185. doi:10.1302/0301-620X.89B2.18358
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jacques Hernigou, Esfandiar Chahidi, Mahine Kashi, Eric Moest, Bassel Dakhil, Georges Hayek, Antoine Callewier, Frederic Schuind, Olivier Bath declare that they have no conflict of interest.
Electronic supplementary material
The video presents 3D images of a leg and arteries target and the risk map according to our results (in green areas where arteries were never observed, in red areas were arteries were observed). (MP4 50682 kb)
Rights and permissions
About this article
Cite this article
Hernigou, J., Chahidi, E., Kashi, M. et al. Risk of vascular injury when screw drilling for tibial tuberosity transfer. International Orthopaedics (SICOT) 42, 1165–1174 (2018). https://doi.org/10.1007/s00264-017-3554-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3554-7