Abstract
Purpose
To explore the diagnosis, treatment, and clinical prognosis of patients with both unstable pelvic fractures and concomitant acetabular fractures.
Material and methods
We retrospectively analyzed 21 cases of unstable pelvic fractures with concomitant acetabular fractures treated between January 2013 and December 2014. All 21 patients (18 males, 3 females), aged 43.5–55 years (range: 21–55 years), underwent surgery within four to 15 days (average = 6.5 days) after injury. We evaluated the pre-operative diagnoses, surgical approaches, types of fixation used, and prognoses.
Results
All 21 patients were followed-up for six to 18 months. The quality of post-operative pelvic fracture reduction (determined using the Matta scoring criteria) was excellent in five cases, good in 12, and fair in four. The clinical outcomes at the final follow-up (scored using the Majeed criteria) were excellent in ten cases, good in eight, and fair in three. The quality of post-operative acetabular fracture reduction (determined using the Matta scoring criteria) was excellent in five cases, good in 11, and poor in five. Hip joint function was evaluated at the final follow-up (using the D’Aubigné scoring system) and was excellent in eight cases, good in nine, and fair in four. The healing time was 12–18 weeks for pelvic fractures and 12–22 weeks for acetabular fractures. Post-operative wound infections in two patients were controlled after second operations featuring debridement and irrigation. We found no instance of heterotopic ossification, ischemic necrosis of the femoral head, or iatrogenic vascular or nerve injury.
Conclusions
Good therapeutic outcomes in patients with unstable pelvic fractures and concomitant acetabular fractures can be achieved via accurate diagnosis, careful pre-operative planning, a well-performed operation, effective reduction and surgical fixation, and appropriate exercise to allow functional rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic fractures often occur secondarily to high-energy injuries, primarily traffic accidents and falls from height, and occur along with multiple injuries at other bodily locations. Pelvic fractures are associated with high mortality and disability rates [1]. In the Tile classification system, type B (rotationally unstable) and C (rotationally and vertically unstable) pelvic fractures are both considered unstable. Emergency trauma control and restoration of pelvic ring stability are critical if such patients are to survive [2]. As malunion of pelvic fractures often triggers long-term dysfunction, surgical reduction and fixation are required to restore stability and assist patients to commence early functional exercises. Both acetabular and intra-articular fractures require anatomical reduction and internal fixation. The anatomy and fracture type are frequently both complex, such that surgery is often challenging. Also, no consensus has emerged on either the choice of surgical approach or the fixation method. When an unstable pelvic fracture and an acetabular fracture co-occur, the combined injury has a greater impact. After early trauma control to save the patient’s life, we face the challenge of conducting very difficult reduction and fixation of both pelvic and acetabular fractures.
We conducted a retrospective analysis of the outcomes of 21 patients with combined fractures treated from January 2013 to December 2014.
Materials and methods
General information
The exclusion criteria were age below 18 years, an open pelvic fracture, and no surgical treatment within 20 days of injury. We included 21 patients (18 males and 3 females) aged 21–55 years (mean = 43.2 years). The causes of injury were traffic accidents in 15 cases and falls from a height in six. Emergency treatment included trauma control (mainly fixation of the pelvic girdle or temporary anterior external fixation to control the pelvic volume), combination treatment of the internal disease and associated injuries, and trauma life-support [3]. All patients underwent regular X-ray and thin-section computed tomography (CT) examinations upon admission.
Based on the medical imaging data and the Tile classification [4], we diagnosed 12 type B and nine type C pelvic fractures. The acetabular fracture type was determined using the Letournel-Judet classification [5]; there were 11 transverse fractures, five double-column fractures, three fractures of both the posterior column and posterior wall, and two anterior column fractures (Table 1). Other injuries were present in 18 cases, including chest injuries in ten, craniocerebral injuries in three, and abdominal injuries in five. All patients received appropriate and timely treatment. Fractures in other parts of the body included three intertrochanteric fractures, two fractures of the femoral neck, three lumbar fractures, two ankle fractures, and two fractures of the femoral shaft. Three patients exhibited symptoms of injury to the cauda equina.
Pre-operative preparation
Before surgery, the X-ray and CT reconstruction data were carefully analyzed. For complicated fractures, three-dimensional (3D), actual-size printed models (provided by the Digital Division of our Department of Orthopaedics) were used to determine fracture type, assess fracture locations, measure the extent of displacement of pelvic anterior and posterior ring fractures, assess the extent of displacement of acetabular fractures, and evaluate the extent of damage to the articular surface.
We selected appropriate surgical approaches and methods of fixation. For fractures of the posterior pelvic ring, we chose either open reduction and fixation by fixing steel plates to the sacroiliac joint, or closed reduction and fixation using sacroiliac joint screws. For fractures of the anterior pelvic ring, fixation featured the placement of pubic symphysis or pubic ramus plates, or percutaneous screws. For acetabular fractures, the single ilioinguinal approach was our first choice, but posterior fixation or a combined anterior and posterior approach was chosen for patients with severely comminuted double-column fractures or combined fractures of the posterior wall. Routine pre-operative preparation was implemented, and the operation planned in detail, after patients were evaluated by the Department of Anaesthesia in consultation with other departments to ensure that there was no contraindication to surgery. The average interval between injury and surgery was 6.5 days (range: 4–15 days).
Surgical methods
All operations proceeded under general anaesthesia. We initially performed reduction and internal fixation of ipsilateral femoral fractures, thus rendering traction during surgery more convenient. Most patients were placed in the supine position. Patients in whom acetabular fractures were to be fixed by a combined anterior and posterior approach, or a posterior approach alone, were placed in the lateral floating position. The surgical areas were disinfected and surgical drape sheets were placed; patients were repositioned as needed during the procedure.
We first performed fixation of any displaced fracture of the posterior pelvic ring. For patients exhibiting sacroiliac joint separation or a displaced fracture of the iliac wing that ran across the sacroiliac joint, the operation was performed via an ilioinguinal approach to the first window, to fully expose the dislocation or iliac wing fracture. Under direct vision, we performed fracture reduction and fixation using shaped steel plates and screws. For severe fractures in Denis zones I and II, we initially performed closed reduction of the sacral displacement fractures and then proceeded to fixation under X-ray guidance; we percutaneously placed one or two sacroiliac joint screws in the contralateral cortex.
We next treated the acetabular fractures. In patients with double-column, anterior column, or T-shaped fractures, we first attempted a single anterior approach. Using three windows of the ilioinguinal approach, the anterior column and posterior bones were repositioned and the anterior column fractures fixed with plates and screws; the posterior column fractures were fixed with extension screws (from front to back). If reduction of the posterior fracture was difficult, the patient was turned over and fixation proceeded via the posterior Kocher-Langenbeck approach. In those with fractures of the posterior wall, the Kocher-Langenbeck approach was routinely used.
Finally, we repaired fractures of the pelvic anterior pelvic ring. Such injuries usually featured separation of the pubic symphysis, or were fractures of the superior and inferior pubic rami. In those with fractures of the pubic bone, reduction was performed via an ilioinguinal approach, followed by fixation using shaped steel plates or percutaneous placement of hollow nails into the pubic bones. In those with separations of the pubic symphysis, fixation featured the use of steel plates or hollow nails.
Post-operative treatment
Surgical drainage tubes were placed for 24–72 h, abdominal bandages were applied under pressure, and antibiotics were prescribed for three to seven days. After the drainage tubes were removed, conventional anticoagulants were given to prevent thrombosis. Appropriate medications were prescribed for patients with neurological symptoms, and rehabilitative exercise was commenced. At eight weeks post-surgery, patients were allowed to walk with crutches, and at 12 weeks they were allowed to try free walking according to the extent of healing. Several post-operative X-rays (pelvic front view, iliac oblique view, and obturator oblique view) were taken and CT examinations performed.
Follow-up
Patients were hospitalized for ten to 25 days (average = 13 days), after which they were followed-up every month. At each follow-up, regular X-rays were taken (with CT done as necessary) to assess healing and functional recovery; guidance on weight-bearing and rehabilitative exercises was also imparted.
Results
The average surgical duration was 3.1 hours (range: 2.5–6.0 hours). The mean blood loss was 1200 mL (range: 500–4000 mL). Post-operatively, nine patients had haemoglobin levels <7 mg/dL and received transfusions of allogeneic red blood cells.
The quality of postoperative pelvic fracture reduction (using the Matta criteria) [6] was excellent in five cases, good in 12, and fair in four; the excellent-plus-good rate was thus 81%. The quality of post-operative acetabular fracture reduction (using the same criteria) was excellent in five cases, good in 11, and poor in five, the excellent-plus-good rate was thus 77% (Table 1).
All patients were followed-up for six to 18 months (average 9 months). The healing time was 12–18 weeks (average = 14.5 weeks) for pelvic fractures and 12–22 weeks (average = 15.5 weeks) for acetabular fractures. The clinical outcomes at the final follow-up (scored using the Majeed criteria) [7] were excellent in ten cases, good in eight, and fair in three; the excellent-plus-good rate was thus 85%. Hip joint function was evaluated at the final follow-up using the D’Aubigné criteria [8] and was excellent in eight cases, good in nine, and fair in four; the excellent-plus-good rate was thus 81% (Table 1).
We encountered two cases of post-operative infection; these were confirmed (on second operation) to be superficial infections of the subcutaneous tissues. The infections were controlled by debridement and irrigation. Three patients who exhibited neurological symptoms recovered by four to six months postoperatively. We encountered no instance of failure to heal, heterotopic ossification, iatrogenic vascular or nerve injury, ischemic necrosis of the femoral head, or post-traumatic arthritis.
Discussion
Unstable pelvic fractures combined with acetabular fractures are not uncommon in patients with pelvic trauma, being present in about 15% of such patients [9]. Combined fractures of both the pelvis and acetabulum are mostly secondary to high-energy injury; severe fractures of this type are associated with high-level mortality. Appropriate emergency measures, secondary reconstruction, and orthopaedic expertise are key if such patients are to survive [10, 11]. After comprehensive trauma care and advanced life-support, the patients of the present study were able to undergo secondary reconstructive surgery. The peculiar anatomical features and locations of both the pelvis and acetabulum render the surgical treatment of pelvic and acetabular fractures especially challenging.
Most unstable pelvic fractures are displaced in complicated ways. In those with acetabular fractures, displacement of the articular surface of the bone, the presence of comminuted and compressed bone, and the unique anatomy involved render accurate diagnosis difficult. Therefore, when planning treatment, we used both conventional imaging data and advanced, actual-size 3D printing techniques. These techniques yielded the required diagnostic information in a complete, accurate, and directly viewable manner, allowing us to fully understand the type and degree of displacement (Figs. 1, 2, 3 and 4).
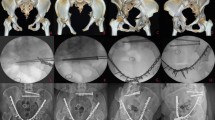
A male patient, 29 years old, had a Tile B pelvic fracture with acetabular transverse fractures on the left side caused by a motor vehicle accident (a). On day six after injury, the acetabular fractures were treated with anterior open reduction followed by internal fixation with steel plates and hollow screws. The pubic symphysis separation was reset and then stabilized by percutaneous hollow screw fixation. The quality of both pelvic and acetabular reductions was scored as excellent (b). The x-ray film showed good fracture healing 16 weeks after surgery (c)
A female patient, 21 years old, had a right-sided Tile C pelvic fracture with acetabular transverse fractures caused by a fall from a 10 metre height (a). The diagnosis was confirmed by the presurgical life-size 3D printing model of the fractures (b). The operation was conducted 5 days after injury. During the surgery it was found difficult to use the single anterior approach; therefore, the combined (anterior and posterior) approach was taken to implement reduction and fixation. The dislocated sacroiliac joint was reset and then stabilized using steel plate and screw fixation; the acetabular transverse fractures were treated with reduction followed by fixation with steel plates and hollow screws; pubic ramus fractures were stabilized with percutaneous hollow-screw fixation. The postoperative x-ray film showed excellent reduction of the pelvic fracture and good reduction of the acetabular fracture (c). Based on the x-ray film, the pelvic fracture had healed by 16 weeks after surgery and the acetabular fracture had healed by 21 weeks (e)
A female patient, 48 years old, had a Tile B pelvic fracture with acetabular transverse fractures on the right side caused by a car accident (a). On day 6 after injury, the acetabular fractures were treated with anterior open reduction followed by internal fixation with two steel plates . The quality of both pelvic and acetabular reductions was scored as good (b). The X-ray of three months (c), half a year (d), 1 year (e) and 1.5 years (f) after surgery showed the fracture healing
A female patient, 33 years old, had a Tile C pelsssvic fracture with acetabular double column fractures on the left side and anterior column on the right side caused by high falling (a). On day 5 after injury, the acetabular fractures were treated with anterior open reduction followed by internal fixation with four steel plates on the left side and one plate on the right side. One hollow screw fix the sacroiliac joint on the right side. The quality of both pelvic and acetabular reductions was scored as excellent (b). The X-ray of three months (c), half a year (d), 1 year (e), and 1.5 years (f) after surgery showed the fracture healing
In the present study, most acetabular fractures were transverse and column fractures, consistent with earlier reports [12]. Takashi et al. [12] reported that transverse fractures were the most common acetabular fractures found in combination with pelvic fractures, accounting for about two-thirds of all cases.
The choice of surgical approach, order of fixation, and optimal method for treatment of unstable pelvic and concomitant acetabular fractures all remain controversial. We first performed reduction and fixation of the posterior pelvic ring and then treated the acetabular fracture. Finally, we reduced and fixated injuries to the anterior pelvic ring.
Injuries to the posterior pelvic ring are principally longitudinal or compression fractures of the sacrum, sacroiliac joint dislocations, or fractures of the iliac wing that are displaced across the sacroiliac joint (crescent-shaped fractures). During reduction and fixation of fractures of the posterior pelvic ring, serious sacral fractures were treated via closed reduction followed by percutaneous stabilization of the sacroiliac joint with hollow, modular anchorage screws. In patients with certain Tile B pelvic fractures (i.e., those in which the sacral bone was partially compressed), fixation of the anterior pelvic ring was used to restore ring stability. In patients with sacroiliac joint dislocations or iliac wing fractures proceeding across the sacroiliac joint, we used an ilioinguinal approach to the first window, followed by reduction and fixation with shaped steel plates and screws under direct vision.
In patients with acetabular fractures, after reduction and fixation of the posterior pelvic ring, the bones of the back served as the “main bone” reference during gradual resetting of the fractures. In line with the conclusions of a previous study [13], we consider that most acetabular fractures (including displaced fractures of the posterior column) can be treated via a single anterior approach. Therefore, during pre-operative disinfection and surgical draping, we always prepared with the potential need for a combined (anterior and posterior) approach in mind, but we first used an ilioinguinal approach only to reset and fix all acetabular bones. Fractures of the posterior column were fixed using hollow screws for modular anchorage. When it was difficult to reduce posterior pelvic ring bones, either during the operation or when the preoperative diagnosis suggested that the posterior wall was fractured, we preferred the posterior Kocher-Langenbeck approach.
Injuries to the anterior pelvic ring are typically fractures of the superior and inferior rami of the pubis, and separation of the pubic symphysis. After we treated posterior pelvic ring and acetabular fractures, anterior pelvic ring fractures were usually reset using shaped steel plates, screw fixation, or percutaneous fixation with hollow nails.
Our treatments yielded good results. We suggest how unstable pelvic fractures with concomitant acetabular fractures may be successfully approached. However, individual variation is extensive and our sample size was small; it thus remains difficult to define an ideal replacement order or fixation method when treating patients with such fractures.
Post-operatively, we used both imaging and functional scores to assess outcomes; 80% of patients enjoyed excellent or good recovery, as previously reported [14]. No intervention was required by the three patients who had cauda equina injuries caused by trauma; all recovered to various extents after four to six months. The principal surgical complication was wound infection, possibly associated with the relatively long operative time and the large wound size. Pre-operative preparation, optimization of the surgical procedure, and preventative practices after surgery are all of critical importance.
In patients with both unstable pelvic and acetabular fractures, appropriate emergency protocols, trauma control, and advanced life-support systems afford good opportunities for secondary surgical reconstruction. Imaging data and full-size 3-D printing yield accurate and comprehensive information facilitating pre-operative diagnoses. These techniques reveal the nature and extent of fracture displacement, thus enabling surgical planning. It is important to choose an appropriate surgical approach, prepare the disinfected area carefully, place surgical drape sheets, and anticipate all issues that might be encountered during the planned procedure. Additionally, it is essential to avoid iatrogenic injury, place a post-operative drain when necessary, prevent thrombosis, and encourage well-designed rehabilitation. All of these measures contribute to the attainment of optimal therapeutic effects.
References
Karadimas EJ, Nicolson T, Kakagia DD et al (2011) Angiographic embolisation of pelvic ring injuries. Treatment algorithm and review of the literature. Int Orthop 35:1381–1390
Halawi MJ (2016) Pelvic ring injuries: emergency assessment and management. J Clin Orthop Trauma 6:252–258
Poenaru DV, Popescu M, Anglitoiu B et al (2015) Emergency pelvic stabilization in patients with pelvic posttraumatic instability. Int Orthop 39:961–965
Tile M (1988) Pelvic ring fractures: should they be fixed? J Bone Joint Surge(Br) 70:1–12
Letournel E (1980) Acetabulum fracture: classification and management. Clin Orthop 151:81–106
Matta JM, Tornetta P (1996) Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res 329:129–140
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg(Am) 78(11):1632–1645
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Joint Surg (Br) 71:304–306
Gansslen A, Pohlemann T, Paul C et al (1996) Epidemiology of pelvic ring injuries. Injury 27(Suppl 1):SA13–SA20
Vaidya R, Oliphant BW, Hudson I et al (2013) Sequential reduction and fixation for windswept pelvic ring injuries (LC3) corrects the deformity until healed. Int Orthop 37:1555–1560
Vallier HA, Cureton BA, Ekstein C et al (2011) Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma 69:677–684
Takashi S, Wade RS, David JH et al (2010) Combined injuries of the pelvis and acetabulum: nature of a devastating dyad. J Orthop Trauma 24:303–308
Zhu S, Wang M, Wu X et al (2005) Operative treatment of compound acetabular fractures through single ilioinguinal approach. Chin J Orthop Trauma 7:1025–1027
Matta JM (1994) Operative treatment of acetabular fractures through the ilioinguinal approach. A 10 -year perspective. Clin Orthop Relat Res 305:10–19
Acknowledgements
This work was supported by the National Natural Science Foundation of China (grant no. 81472146) and the Natural Science Foundation of WenZhou City (grant no. Y20160135). The funders played no role in the study design, data collection or analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics statement
All procedures involving human participants were performed in accordance with the ethical standards of our institutional and national research committees, and with those of the 1964 Helsinki declaration and later amendments thereof, or comparable ethical standards. Formal Ethics Board consent was not required for this study.
Rights and permissions
About this article
Cite this article
Cai, L., Lou, Y., Guo, X. et al. Surgical treatment of unstable pelvic fractures with concomitant acetabular fractures. International Orthopaedics (SICOT) 41, 1803–1811 (2017). https://doi.org/10.1007/s00264-017-3532-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3532-0