Abstract
Introduction
The resection of os trigonum or posterior talar process as treatment for posterior ankle impingement is an established operation. However, the authors encountered several painful stress reactions in the posterior subtalar joint during follow-up resulting in persisting incapacity to do sports.
Methods
From March 2011 to July 2015, 29 patients with 30 feet were operated (22 endoscopic, 8 open resections). Average follow-up time was 43 ± 13 months. Complications were grouped into “none”, “temporary disadvantage” and “permanent damage”. The following radiographic parameters were measured: (1) length of posterior talar process or os trigonum, (2) length of the uncovered calcaneal joint surface after resection, (3) amount of resection.
Results
The rate of permanent damage was 13.3% (4 of 30 feet), and all four of these patients developed a painful stress reaction in the posterior subtalar joint. One temporary disadvantage (persistent pain for three months) was found. All patients with major complications showed retrospectively what we call the “risk configuration” —the radius of the talus ending within the subtalar joint. The length of the uncovered calcaneal joint surface was therefore significantly larger (6.4 mm ± 3.33) in feet with permanent damage than in feet without (1.06 mm ± 2.15, P < 0.001).
Conclusion
The resection of os trigonum or posterior talar process has a complication rate of 13.3% with persisting inability to do sports due to painful stress reaction in the posterior subtalar joint. The only risk factor found was the “risk configuration”. In such cases, the resection has to be made not anterior into the subtalar joint and patients have to be informed about this possible complication.
Study design
Retrospective case series; Evidence Level 4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior ankle impingement syndrome is a frequent problem in patients who regularly engage in activities involving strong and repetitive plantar flexion such as ballet, running, soccer, hockey, and gymnastics [1,2,3,4,5,6]. Possible reasons include a symptomatic os trigonum, a prominent posterior talar process, a fractured posterior talar process or flexor hallucis longus (FHL) entrapment and posterior soft tissue impingement [1, 7]. If conservative treatment such as injections, rest, and physiotherapy failed, surgery is necessary [2, 8,9,10,11]. The standard surgical treatment consists of the debridement of soft tissue, the release of the FHL-tendon and a resection of the os trigonum or the prominent posterior talar process.
While open and arthroscopic approaches have been described, the scientific literature has especially focused on the advantages of the endoscopic over the open surgery (Table 1). The complications reported so far were mainly peri-operative complications summarized in Table 1. Excluding the study of Nikisch [12] (because the complications can not be attributed to the indications and only 46 out of 189 operations were due to os trigonum) and three cases of Kim [5] (which had just posterior soft tissue impingement), there were a total of 266 resections of os trigonum or posterior talar process with an average follow up of 26 months. Of these 8% (21/226) suffered from complications: transient nerve problems (8), permanent nerve problems (9), infections (1), chronic regional pain syndrome (CRPS) (1), and permanent pain (2).
However, among the patients treated by the authors, there were several young athletes who had resection of os trigonum or posterior talar process that were correctly performed from a surgical point of view, but patients later developed persistent pain due to painful stress reaction in the posterior subtalar joint. As a result they were permanently unable to do sports. There is no literature on this issue yet. The aim of this study was to describe and understand the cause of this persisting inability of some patients to do sports after a resection of os trigonum or posterior talar process. The hypothesis of the study was that feet developing this problem have a different osseous configuration of the posterior subtalar joint than feet with an unproblematic post-operative course.
Therefore, the study questions were:
-
1.
What is the complication rate after resection of os trigonum or posterior talar process?
-
2.
What risk factors can be extracted from radiographs of patients’ ankles (size of os trigonum or posterior talar process, amount of resection, uncovered subtalar joint surface)?
-
3.
What risk factors can be extracted from patients’ history?
Materials and methods
Materials
Between March 2011 and July 2015, 30 feet were operated in 29 patients (17 male, 12 female, average age 32 ± 14 years, range 16–70 years). The diagnosis was os trigonum in 22 feet and a prominent posterior talar process in 8 feet. Inclusion criteria were that (1) patients underwent resection of an os trigonum or posterior talar process due to posterior impingement after failed conservative treatment, and that (2) complete pre- and post-operative data sets (including clinical parameters, pre- and post-operative radiographs and MRI/CT in the follow-up where applicable) were available. Exclusion criteria were incomplete charts or radiographic data. The latest follow-up took place in December 2016. Average follow-up time was 43 ± 13 months (range 18–69 months).
Non-operative and operative treatment
The diagnosis was made on grounds of clinical symptoms (persistent posterior ankle pain, with or without restricted range of motion), clinical exam (posterior ankle pain in forced plantar flexion which got worse when the examiner pushed a finger into the posterolateral or posteromedial ankle, possibly restricted range of motion), and radiographs (obvious os trigonum or excessively long posterior talar process, which may get compressed between tibia and calcaneus in plantar flexion). Standard upright radiographs included a lateral foot, antero-posterior ankle, and, where necessary, a hindfoot alignment view. All patients underwent first a non-operative treatment (rest, no sports, pain medication) including a radiographically guided infiltration of the os trigonum or prominent posterior process under local anaesthetic and the concomitant administration of cortisone, which served at once as diagnostic test and therapy. If these measures did not lead to a permanent pain relief after three to six months, an MRI was made to rule out other pathology (if an MRI had not already been made in the first clinical assessment). In such cases the MRI typically showed oedema within the os trigonum or posterior talar process as well as in the surrounding bone, especially in the synchondrosis towards the talus [3, 20]. In six cases the MRI did not lead to a clear explanation of the clinical symptoms and for this reason a single-photon-emission computed tomography (SPECT) was added.
If clinical symptoms, clinical examination, radiological findings and positive infiltration all confirmed the diagnosis, then patients underwent surgery. Concomitant pathology was addressed in the same operation. On 14 feet an isolated resection of os trigonum or posterior talar process was carried out. On 16 feet a total of 20 combined surgeries were carried out: chronic ankle instability with lateral and / or medial ligament repair (n = 10), gastrosoleus-release for Achilles-tendinitis (n = 2), anterior ankle impingement arthroscopically with shaving and resection of anterior osteophytes (n = 2), microfracture for osteochondral defect (n = 1), lateral sliding calcaneal osteotomy due to hindfoot varus and chronic ankle instability (n = 1), FHL-transfer due to Achilles-tendinopathy (n = 1), neurolysis of the sural nerve (n = 1), tarsal tunnel release (n = 1) and Haglund-resection for symptomatic insertional Achilles tendinitis (n = 1).
All patients were operated by two fellowship-trained foot and ankle surgeons with more than ten years of experience. There were 22 endoscopic and eight open resections. Open resections were performed in case of combined surgery to proceed faster. In open surgery, depending on the concomitant procedures, a posterolateral or posteromedial approach was chosen and the os trigonum or the posterior process was resected. The endoscopic procedure was performed as described by Van Dijk [21]; the impinging soft tissue as well as the FHL-tendon were debrided and the posterior process reduced and controlled under fluoroscopy.
The post-operative treatment varied depending on the kind of surgery. If patients had an isolated resection, patients had to use crutches for one to two weeks but were allowed to put as much weight as tolerated. In cases of ligament repair, calcaneal osteotomy or FHL-transfer, patients were required to put only part of their weight on the foot for six to12 weeks.
Methods
The study was carried out in accordance with the Declaration of Helsinki. It was approved by the ethical review board of the authors’ university and all subjects gave informed written consent. All pre-operative and post-operative charts were evaluated. All patients who had made a full recovery (and needed no further medical attention) were contacted by telephone in December 2016 and were invited for a final follow-up. The cases were then divided into three groups according to their post-operative recovery using the categories of Goslings and Gouma [22]. Patients who experienced no complications were assigned to group 1; patients who had to face a temporary disadvantage such as haematoma, swelling, loss of sensibility or prolonged pain (<3 months of duration) were assigned to group 2; patients who were left with a permanent damage such as inability to do sports due to persistent pain or subtalar arthrodesis as a consequence were assigned to group 3.
All patients had a follow-up six to12 weeks after surgery, and another one after a year; additional consultations were scheduled where necessary. If, after using the operated foot normally for three months, a patient was still experiencing pain, then an MRI was made. If the MRI was inconclusive, a SPECT was done.
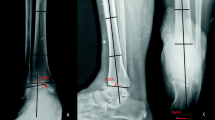
Radiographs were routinely taken either two to three days after surgery or during the first follow-up six to12 weeks after surgery. Radiographs were evaluated on a digital high-resolution picture archiving system by a radiologically trained physician. The analysis was based solely on lateral ankle radiographs that were taken from an angle of 10–15 degrees of internal rotation, which ensured that the medial and lateral talar surface overlapped. In order to measure the pre-operative size of the os trigonum or the posterior talar process (Fig. 1) the authors started by drawing a vertical reference line at the intersection of the talar radius and the calcaneus (arrow in Fig. 1) [23]. Then the following radiographic parameters were measured (Fig. 1): (1) length of posterior talar process or os trigonum dorsally from the reference line; (2) length of the uncovered subtalar joint after resection ventrally from the reference line; and (3) amount of bony resection.
Statistics
Average and standard deviation (SD) were calculated for all descriptive and radiological data. A comparison was made using an independent t-test (Statistica 12, Statsoft, Tusla, USA) between the group without permanent damage (group 1 and 2) and the group with permanent damage (group 3) with respect to the length of the os trigonum or posterior talar process pre-operatively, length of the talar process post-operatively, the resulting amount of resection and the uncovered subtalar joint surface. P-values below 0.05 were considered significant.
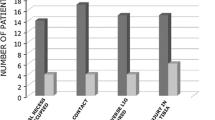
Results
Twenty-five out of 30 feet healed as expected (group 1). In one case a temporary disadvantage occurred (transient pain resolved after three months) (group 2). In four out of 30 feet (13.3%) permanent damage occurred (group 3), whereby all four feet developed a painful stress reaction in the posterior part of the posterior subtalar joint of 5–10 mm diagnosed by MRI and/or SPECT-CT. The patients, while not suffering from pain in daily life, were unable to do any sports after surgery. This was disappointing in particular because these patients were able to do sports before the operation (albeit activities were restricted by pain caused by the posterior ankle impingement), and pain levels became incapacitating after surgery. Two patients were treated with subtalar arthrodesis in the follow-up and two chose to give up sports.
The length of the posterior talar process or os trigonum in all patients was 9.37 ± 2.89 mm (os trigonum: 8.62 ± 2.62 mm) pre-operatively and 0.64 ± 1.8 mm post-operatively (Tables 2 and 3). The uncovered subtalar joint surface post-operatively was 1.77 ± 2.92 mm. In complicated cases, the amount of resection was even smaller (rather than larger) than in unproblematic cases. This was because in complicated cases the pre-operative length was also smaller (Tables 2 and 3).
An analysis of the cases in group 3 revealed a specific configuration of the subtalar joint (Figs. 2, 3 and 4): the radius of the talus ended within the subtalar joint (anterior to the edge of the articular surface of the calcaneus; Figs. 2, 3 and 4). We call this the ‘risk configuration’ (RC). Cases of group 3 consequently had a significantly larger free subtalar joint surface after surgery (6.4 ± 3.33 mm) than feet without major complications (1.06 ± 2.15 mm, P < 0.001). An analysis of the entire patient group revealed that 36% of all feet had RC. Hence, feet with RC had a 36% risk of a major complication (4 out of 11 cases, odds ratio = 23.4, 95% confidence interval 1.1–489.9). RC feet with major complications had a larger free subtalar surface than RC feet without major complications (7/26, 3.94 ± 2.44 mm, P = 0.19). However RC-feet without complications had similar pre-operative length and amount of resection as feet with major complications (Tables 2 and 3).
SPECT-CT and MRI of the same athlete as in Fig. 2 showing the onset of painful stress reactions in the posterior subtalar joint with incapacity of sports requiring subtalar fusion after two years
As regards risk factors in the patients history, the reported initiating events were acute ankle sprains (n = 12), acute ankle sprains in pre-existing chronic ankle instability (n = 3), chronic ankle instability (n = 5), plantarflexion trauma (n = 2), plantarflexion trauma with ankle sprain (n = 1), prior ankle fractures (n = 3) and intensive sports (professional tennis player, marathon runner, soccer player, n = 4).
Looking retrospectively at the four cases with permanent damage, we find the following. (1) Two of them were os trigonum (of those one had earlier fractured the posterior talar process) and two were prominent posterior talar process. (2) All four cases had only an isolated resection by endoscopic technique and no additional surgeries. (3) Re-evaluating the pre-operative MRIs of these cases, we found that one already showed a slight stress reaction in the posterior part of the posterior subtalar joint; one showed a loss of cartilage; and two had no additional pathologies. However, five out of the 26 feet without complications showed slight degenerative changes (loss of cartilage, sclerosis, subchondral cysts) and remained uneventful during the entire follow-up.
Discussion
The resection of os trigonum or posterior talar process for posterior ankle impingement is an established operation. However, the authors found that 13% of patients remain unable to do any sports due to the onset of painful stress reaction in the posterior subtalar joint. All patients with permanent complications showed what we call the risk configuration: the radius of the talus ending within the subtalar joint.
The complication rate reported in the literature was 8% (21/226) and mainly reflected peri-operative complications (Table 1). No cases of painful stress reaction in the posterior subtalar joint are reported hitherto in the literature. The following explanations for the onset of painful stress reactions in the posterior subtalar joint seem possible. First, one might hypothesize that the resection of the os trigonum or posterior talar process can increase dorsal subtalar instability because of the reduction of the osseous containment. This reduction is insignificant in everyday contexts because the remaining part of osseous containment is able to withstand the forces caused by ordinary movements. The reduction becomes significant, however, when a patient does sports and the joint has to withstand vertical forces of up to five times the patient’s bodyweight combined with shear forces caused by the stop-and-go and lateral movements that are typical of athletic activities [24]. This would explain why patients remain asymptomatic as long as they just walk and only develop pain when they do sports. This theory is supported by the fact that we encountered a history of ankle instability in 21 out of 30 patients and only two patients suffered from a plantar flexion trauma, which is reported to be the most common reason for a fracture of the posterior talar process or activated os trigonum in the literature [7]. Many of our patients also had concomitant surgery, which shows that an activated os trigonum or symptomatic posterior talar process are often not an isolated pathology. We therefore hypothesize that instability may also be a reason for making these pathologies symptomatic in the subtalar joint. Second, all patients with permanent complications also showed a talar oedema. The oedema can be seen as the effect of a stress reaction due to higher joint pressure caused by the reduced joint surface after resection [25]. Third, it is difficult to distinguish retrospectively between a fractured posterior talar process and an os trigonum [7, 16, 26]. One of the complicated cases was an earlier fractured posterior talar process that was accompanied by cartilage damage of the accident seen pre-operatively as slight degenerative changes in the subtalar joint in the MRI. After the resection, the symptoms became worse. However, also five out of the 26 complication-free feet showed slight degenerative changes pre-operatively and remained uneventful during the entire followup. A pre-existing cartilage damage is therefore not a predictor for permanent damage.
In the literature there is no recommendation as regards the amount of resection. The resection of the posterior talar process is an established treatment in posterior ankle impingement [4, 15, 17, 19] and 26 out of 30 feet became pain-free. Only two studies report the pre-operative size of the os trigonum to be 1.1–2.5 cm, which is even larger than in our study [2, 27]. Nevertheless we have to conclude that our resection was too large in cases with RC (Table 2). We therefore recommend making the resection in patients with RC smaller, preferably not anterior into the subtalar joint, and perform the operation under fluoroscopic control to avoid such complications in the future.
All four permanent damages occurred in isolated arthroscopic resections. We therefore conclude that neither the approach nor the concomitant surgeries contribute to the complication rate. This is because the soft tissue approach has no influence on the mechanical consequences of the resection and a concomitant ankle ligament repair might be beneficial rather than harmful according to our hypothesized explanations.
This study has several limitations. First, it is a retrospective study and 16 of 30 feet also had additional surgery. However, in our view, these other operations (e.g. ligament repairs, calcaneal osteotomy, Achilles tendon surgery) did not contribute to the complication rate, which is supported by the fact that all cases with permanent damage had no additional surgery. On the contrary, Ahn reports that the complication rate could be higher if complex foot and ankle surgery had been performed earlier or simultaneously [2]. A study with only isolated resections could be needed in the future. Second, this is the first study assessing the length of the posterior talar process or os trigonum. Therefore a reference line had to be defined. However no previous studies operate with lines of this kind or recommend how much to resect (Table 1). Third, one could argue that the concept of risk configuration should have been developed on MRI images and not on radiographs. However, during an operation, the surgeon can only rely on the amount of resection on the radiographs of the image intensifier. Therefore we aimed to develop a concept that can be applied during surgery.
Conclusion
The resection of os trigonum or posterior talar process had a complication rate of 13% with painful stress reactions in the posterior subtalar joint during follow up which can be career-ending in athletes. We identified a risk factor which we called the “risk configuration”. The defining feature of this configuration was that the talar radius ends inside the subtalar joint. In such cases, the resection should be made sparingly, preferably not anterior into the subtalar joint, and patients have to be informed about possible future complications.
References
Abramowitz Y, Wollstein R, Barzilay Y, London E, Matan Y, Shabat S, Nyska M (2003) Outcome of resection of a symptomatic os trigonum. J Bone Joint Surg Am 85-A(6):1051–1057
Ahn JH, Kim YC, Kim HY (2013) Arthroscopic versus posterior endoscopic excision of a symptomatic os trigonum: a retrospective cohort study. Am J Sports Med 41(5):1082–1089
Calder JD, Sexton SA, Pearce CJ (2010) Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med 38(1):120–124
Galla M, Lobenhoffer P (2011) Technique and results of arthroscopic treatment of posterior ankle impingement. Foot Ankle Surg 17(2):79–84
Kim HK, Jeon JY, Dong Q, Kim HN, Park YW (2013) Ankle arthroscopy in a hanging position combined with hindfoot endoscopy for the treatment of concurrent anterior and posterior impingement syndrome of the ankle. J Foot Ankle Surg 52(6):704–709
Russell JA, Kruse DW, Koutedakis Y, McEwan IM, Wyon MA (2010) Pathoanatomy of posterior ankle impingement in ballet dancers. Clin Anat 23:613–621
Chao W (2004) Os trigonum. Foot Ankle Clin N Am 9:787–796
Blake RL, Lallas PJ, Ferguson H (1992) The os trigonum syndrome. A literature review. J Am Podiatr Med Assoc 82(3):154–161
Horibe S, Kita K, Natsu-ume T, Hamada M, Mae T, Shino K (2008) A novel technique of arthroscopic excision of a symptomatic os trigonum. Arthroscopy 24(1):121e1–121e4
Richards DT, Guerra JJ, Council D (2010) Arthroscopic excision of the os trigonum: using the posteromedial portal safely. Am J Orthop (Belle Mead NJ) 39(8):379–381
Willits K, Sonneveld H, Amendola A, Griffin JR, Griffin S, Fowler PJ (2008) Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy 24(2):196–202
Nickisch F, Barg A, Salzmann CL, Beals TC, Bonasia DE, Phisitkul P, Femino JE, Amendola A (2012) Postoperative complications of posterior ankle and hindfoot arthroscopy. J Bone Joint Surg Am 94(5):439–446
Guo QW, Hu YL, Jiao C, Ao YF, Tian de X (2010) Open versus endoscopic excision of a symptomatic os trigonum: a comparative study of 41 cases. Arthroscopy 26(3):384–390
Marumoto JM, Ferkel RD (1997) Arthroscopic excision of the os trigonum: a new technique with preliminary clinical results. Foot Ankle Int 18(12):777–784
Noguchi H, Ishii Y, Takeda M, Hasegawa A, Monden S, Takagishi K (2010) Arthroscopic excision of posterior ankle bony impingement for early return to the field: short-term results. Foot Ankle Int 31(5):398–403
Park CH, Kim SY, Kim JR, Lee WC (2013) Arthroscopic excision of a symptomatic os trigonum in a lateral decubitus position. Foot Ankle Int 34(7):990–994
Tey M, Monllau JC, Centenera JM, Pelfort X (2007) Benefits of arthroscopic tuberculoplasty in posterior ankle impingement syndrome. Knee Surg Sports Traumatol Arthrosc 15(10):1235–1239
Veazy BL, Heckman JD, Galindo MJ, McGanity PL (1992) Excision of ununited fractures of the posterior process of the talus: a treatment for chronic posterior ankle pain. Foot Ankle 13(8):453–457
Weiss WM, Sanders EJ, Crates JM, Barber FA (2015) Arthroscopic excision of a symptomatic Os Trigonum. Arthroscopy 31(11):2082–2088
Kubosch EJ, Erdle B, Izadpanah K, Kubosch D, Uhl M, Südkamp NP, Niemeyer P (2016) Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int Orthop 40(1):65–71
Van Dijk CN, Scholtern PE, Krisp R (2000) A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy 16(8):871–876
Gosslings JC, Gouma DJ (2008) What is a surgical complication? World J Surg 32(6):952
Kolb A, Willegger M, Schuh R, Kaider A, Chiari C, Windhager R (2017) The impact of different types of talus deformation after treatment of clubfeet. Int Orthop 41(1):93–99
Badekas T, Takvorian M, Souras N (2013) Treatment principles for osteochondral lesions in foot and ankle. Int Orthop 37(9):1697–1706
Radke S, Vispo-Seara J, Walther M, Ettl V (2001) Transient bone marrow edema of the foot. Int Orthop 25:263–267
Hedrick MR, McBryde AM (1994) Posterior ankle impingement. Foot Ankle Int 15:2–8
Mann HA, Myerson MS (2010) Treatment of posterior ankle pain by excision of a bipartite talar fragment. J Bone Joint Surg (Br) 92-B:954–957
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
The study was approved by the ethical review board. This study was carried out in accordance with the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Frigg, A., Maquieira, G. & Horisberger, M. Painful stress reaction in the posterior subtalar joint after resection of os trigonum or posterior talar process. International Orthopaedics (SICOT) 41, 1585–1592 (2017). https://doi.org/10.1007/s00264-017-3489-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3489-z