Abstract
Purpose
Posterior reduction and pedicle screw fixation is a widely used procedure for thoracic and lumbar vertebrae fractures. Usually, the pedicle screws would be removed after the fracture healing and screw tunnels would be left. The aim of this study is to evaluate the effect of screw tunnels on the biomechanical stability of the lumbar vertebral body after pedicle screws removal by finite element analysis (FEA).
Methods
First, the CT values of the screw tunnels wall in the fractured vertebral bodies were measured in patients whose pedicle screws were removed, and they were then compared with the values of vertebral cortical bone. Second, an adult patient was included and the CT images of the lumbar spine were harvested. Three dimensional finite element models of the L1 vertebra with unilateral or bilateral screw tunnels were created based on the CT images. Different compressive loads were vertically acted on the models. The maximum loads which the models sustained and the distribution of the force in the different parts of the models were recorded and compared with each other.
Results
The CT values of the tunnels wall and vertebral cortical bone were 387.126±62.342 and 399.204±53.612, which were not statistically different (P=0.149). The models of three dimensional tetrahedral mesh finite element of normal lumbar 1 vertebra were established with good geometric similarity and realistic appearance. After given the compressive loads, the cortical bone was the first one to reach its ultimate stress. The maximum loads which the bilateral screw tunnels model, unilateral screw tunnel model, and normal vertebral model can sustain were 3.97 Mpa, 3.83 Mpa, and 3.78 Mpa, respectively. For the diameter of the screw tunnels, the model with a diameter of 6.5 mm could sustain the largest load. In addition, the stress distributing on the outside of the cortical bone gradually decreased as the thickness of the tunnel wall increased.
Conclusions
Based on the FEA, pedicle screw tunnels would not decrease the biomechanical stability and strength of the vertebral body. A large diameter of screw tunnel and thick tunnel wall were helpful for the biomechanical stability of the vertebral body.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pedicle screws play an important role in the treatment of thoracic and lumbar spinal diseases. Since it was first used in 1963 [1], pedicle screw fixation became popular in spinal surgery due to the effect of three-column stabilization and good clinical outcomes. Posterior reduction and pedicle screw fixation is a widely used procedure for thoracic and lumbar vertebral fracture. For young patients, the implanted pedicle screws usually need to be removed after one to two years when the vertebral fracture is healed [2], and the screw tunnels will be left in the fractured vertebral body. Would the tunnels affect the biomechanical stability of the vertebral body? Few studies reported about this.
Finite element analysis (FEA) is a numerical technique, which subdivides a large problem into small, simple parts and creates a model to solve boundary value problems [3]. It is considered to be more valuable than cadaveric study because it can simulate the complexity of stress distribution and displacement for the spinal biomechanical study [4]. In this study, we use FEA to evaluate the effect of screw tunnels on the biomechanical stability and strength of the fractured vertebral body after pedicle screws were removed.
Materials and methods
This study was approved by the ethics committee of the hospital. All patients signed informed consent before they were included in this study.
Measurement of the CT values of screw tunnel wall and the vertebral cortical bone
A total of 30 patients with lumbar vertebral fracture who underwent surgical treatment in our hospital were included in this study. All the fractures were classified as types A and B of AO Magerl classification [5], without spinal dislocation and spinal cord compression, and unilateral/bilateral vertebral pedicles were intact. All the patients underwent one staged posterior open reduction, short-segmental instrumentation combined with pedicle screw fixation at the level of fracture (unilateral/bilateral). The instrumentation segments included one vertebra above and below the fractured one. No posterior decompression procedure was conducted in these patients. After one to two years follow up, the implants of the patients were removed according to Jeon et al’s criterion [2].
The inclusion criteria for patients were as follows: (1) 20-40 years old; (2) the fractured vertebral body was fixed with unilateral or bilateral pedicle screws; (3) the fractures were healed and pedicle screws were removed. Patients who have obvious osteoporosis, endocrine system diseases, vertebral tumors, tuberculosis, ankylosing spondylitis, and other vertebral structural destructive diseases were excluded from this study.
All the included patients underwent lumbar spine CT scan after the pedicle screws were removed, and then the CT values of the screw tunnel wall and cortical bone of the fractured vertebral body were measured and compared.
Establishment of three-dimensional finite element model of lumbar 1 vertebra
An adult patient was included and a CT scan was performed for the lumbar spine (slice thickness: 0.75 mm). The CT images of lumbar 1 (L1) were obtained and stored in DICOM format (Digital Imaging and Communications in Medicine). All the images were then imported into Mimics 17.0 software to build a three-dimensional (3-D) finite element model of the L1 vertebral body. After that, the model was imported into Hypermesh 13.0 software (Altair, USA) for further analysis. The L1 finite element model consisted of a thick layer of cortical bone outside and dense cancellous bone inside. The thickness of the vertebral cortical bone was set as 1 mm.
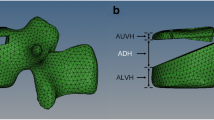
The unilateral/bilateral screw tunnels models were also created by Mimics 17.0 software. The screw diameters (D) ranged from 4.5 mm to 6.5 mm. The thicknesses of the screw tunnel wall ranged from 1.0 mm to 2.0 mm, and the tunnel length was set as 45 mm (Fig. 1). All the models were meshed and analyzed by Hypermesh 13.0 and Abaqus 6.14 (SIMULIA, USA). In this study, we focused on a single lumbar vertebral body with pedicle screw tunnels. All the materials used in these models were considered to be isotropic, homogeneous, and linearly elastic. The elastic properties of the different parts of the vertebral body derive from the literature [6, 7].
Different loads were vertically acted on the cortical bone of the upper vertebral endplate of different models. If one part of the vertebral body reached its ultimate stress, the load acting on the upper endplate of the vertebra was recorded. The loads were then compared with each other.
Statistical analysis
The measurement results were expressed as mean ± standard deviation (SD). All the statistical analysis was performed by IBM SPSS statistics 19.0 software (Armonk, NY, USA). LSD tests were used to analyze the CT values of cortical bone and screw tunnel wall. P < 0.05 was considered to be statistically significant.
Results
CT values of the screw tunnel wall and vertebral cortical bone
According to the CT images, a bony wall formed outside of the pedicle screw after it was removed (Fig. 2). Based on the measurement, the CT values of screw tunnel wall and vertebral cortical bone were 387.126±62.342 and 399.204±53.612, respectively, which were not significantly different (P=0.149). It meant that the screw tunnel wall gradually developed into cortical bone during the period of vertebral fracture healing.
The maximum loads different vertebral models can sustain
Previous studies reported that the ultimate stress which the vertebral cortical bone can sustain is 193 Mpa, while the vertebral cancellous bone can sustain 2.37 Mpa. Each part of the vertebral body corresponded to a value of maximum load when the loads acted on the upper endplate. In this study, we chose the smallest corresponding value as the maximum load for different models. The reason was if the load acted on the model was larger than the smallest corresponding value, one part of the vertebra would break. In this FEA, we selected the load which the cortical bone corresponded as the maximum load of the model sustained. The maximum loads of the different vertebral models sustained are displayed in Table 1. It was larger in the model with screw tunnel than that of normal vertebral model. Additionally, the maximum load in the bilateral tunnels model was larger than that of the unilateral tunnel model (Table 1).
The maximum loads of screw tunnel models with different sustainable diameters
The bilateral screw tunnels models with different diameters were established. The diameters of the screw tunnels included 4.5 mm, 5.5 mm, and 6.5 mm, respectively. We also chose the load which the cortical bone corresponded as the maximum load of the vertebral body sustained. The results are demonstrated in Table 2. As the diameters of the screw tunnel increased, the loads which the vertebral model could sustain increased, too. The model with a tunnel diameter of 6.5 mm could sustain the largest load.
The stress distribution on the models with different thicknesses of tunnel wall
The models with different thicknesses of bilateral screw tunnels wall were created in this study. In order to make clear the influence of different thicknesses of tunnel wall on the biomechanical stability of the vertebral body, loads were given to the upper endplate of the vertebra and the stress distributing on the cortical bone was recorded. The results are shown in Table 3. Based on the analysis, the von Mises stress distributing on the cortical bone of the vertebra gradually decreased as the thickness of the tunnel wall increased. It meant that a large thickness of tunnel wall would help to decrease the stress on the cortical bone.
Discussion
Thoracic and lumbar vertebral fracture is a popular injury to the spine. Open reduction and internal fixation is one of the most effective methods for the treatment of it. Since the pedicle screw was invented and applied to spinal surgery, it has played an important role in the surgical treatment of vertebral fracture. Posterior pedicle screw fixation has the effect of three-column stabilization and can significantly restore the height of the fractured vertebrae [8], which makes it more effective in treating spinal vertebral fracture. However, few studies focused on the biomechanical stability of vertebral body after the pedicle screw was removed.
Recently, the three-dimensional finite element method (FEM) was successful used in the analysis of spinal biomechanics [9–11]. With the updating of computer technologies, three-dimensional nonlinear model established by FEM can vividly imitate the vertebral body and intervertebral disc, and can directly or indirectly add surrounding ligaments and muscles to the model, which makes the imitation real and perfect [12]. The vertebral model created by the three-dimensional FEM can comprehensively reflect spine-related biomechanical properties, and in addition, it easily analyzes the stress distribution of the different parts of the vertebra. Thus, we used three-dimensional FEM to analyze the biomechanical stability and strength of vertebral body with screw tunnels.
It was reported that the CT value can represent the density of bone [13], serving as a significant parameter to reflect bone nature and was generally considered able to reflect 70∼80% of bone strength [14]. In this study, we found that the CT values of the tunnel wall were similar to those of the cortical bone, which meant the tunnel wall developed into cortical bone after pedicle screw implantation. This phenomenon can be explained by Wolff’s law [15]. Since the screw was implanted into the vertebral body, there were compressive loads acting on the cancellous bone around the screw. Gradually, the tunnel wall remodeled and corticalization occurred. Thus, in our study, the material properties of the tunnel wall would refer to the cortical bone during the FEA.
Based on the analysis, the cortical bone of the vertebral body reached its ultimate stress first. Therefore, the load corresponding to the ultimate stress of cortical bone was considered to be the maximum load which the vertebral body can sustain. In order to compare the maximum loads between the normal vertebral model and screw tunnel model, different loads were given on the upper endplate of the models. Based on the results, the maximum load which the screw tunnel model can sustain was larger than that of the normal vertebral model, and the bilateral screw tunnels model could sustain a larger load than that of unilateral screw tunnel. It indicated that pedicle screw tunnels would not decrease the biomechanical stability and strength of the fractured vertebra after pedicle screws removal.
Matsukawa et al [16] found that the size and length of the pedicle screw would affect the fixation strength of vertebral body, and a diameter larger than 5.5 mm and length longer than 35 mm are ideal for pedicle screw fixation. However, few studies focused on the influence of diameter of screw tunnel and thickness of tunnel wall on the biomechanical stability of vertebral body. In order to figure it out, we further analyzed the maximum loads which the vertebral models with different tunnel diameters and thicknesses of wall can sustain by FEA. The results indicated that the diameter of the tunnel would affect the maximum load of the vertebra; and the larger the diameter was, the greater the maximum load which the vertebral model could sustain. It suggested that a large diameter of screw tunnel would increase the biomechanical strength of the vertebral body. In addition, we also analyzed the stress distributing on the cortical bone of the models. It revealed that increasing the thickness of the tunnel wall would decrease the stress on the cortical bone, which meant a thick tunnel wall was helpful for the strength of vertebral body.
Although this study gave a positive support for the idea that pedicle screw tunnel would not decrease the biomechanical stability and strength of the vertebral body, some limitations were detected in it. For example, we just established one single lumbar vertebral model, and the superior and inferior intervertebral discs, the posterior ligaments, muscles, and tendons were omitted from it. This model could not fully simulate the stress distribution and biomechanics of the human spine. So, further animal study and biomechanical analysis is needed to verify the results of this study.
In conclusion, we conducted a study to analyze the effect of pedicle screw tunnels on the biomechanical stability of vertebral body, and found that the maximum load of the screw tunnel model sustained was larger than that of the normal vertebral model. In addition, a large diameter of tunnel and a thick tunnel wall were helpful for the biomechanical stability and strength of the vertebral body. However, further study and biomechanical tests are needed to verify these results.
References
Roy-Camille R, Saillant G, Mazel C (1986) Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res 203:7–17
Jeon CH, Lee HD, Lee YS, Seo JH, Chung NS (2015) Is it beneficial to remove the pedicle screw instrument after successful posterior fusion of thoracolumbar burst fractures? Spine 40(11):E627–E633
Geng JP, Tan KB, Liu GR (2001) Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent 85(6):585–598
Papini M, Zdero R, Schemitsch EH, Zalzal P (2007) The biomechanics of human femurs in axial and torsional loading: comparison of finite element analysis, human cadaveric femurs, and synthetic femurs. J Biomech Eng 129(1):12–19
Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3(4):184–201
Zhang QH, Teo EC (2008) Finite element application in implant research for treatment of lumbar degenerative disc disease. Med Eng Phys 30(10):1246–1256
Chen CS, Chen WJ, Cheng CK, Jao SH, Chueh SC, Wang CC (2005) Failure analysis of broken pedicle screws on spinal instrumentation. Med Eng Phys 27(6):487–496
Ayberk G, Ozveren MF, Altundal N, Tosun H, Seckin Z, Kilicarslan K, Kaplan M (2008) Three column stabilization through posterior approach alone: transpedicular placement of distractable cage with transpedicular screw fixation. Neurol Med Chir (Tokyo) 48(1):8–14
Du CF, Yang N, Guo JC, Huang YP, Zhang C (2016) Biomechanical response of lumbar facet joints under follower preload: a finite element study. BMC Musculoskelet Disord 17:126
Tsouknidas A, Sarigiannidis SO, Anagnostidis K, Michailidis N, Ahuja S (2015) Assessment of stress patterns on a spinal motion segment in healthy versus osteoporotic bony models with or without disc degeneration: a finite element analysis. Spine J 15(3 Suppl):S17–S22
Choi KC, Ryu KS, Lee SH, Kim YH, Lee SJ, Park CK (2013) Biomechanical comparison of anterior lumbar interbody fusion: stand-alone interbody cage versus interbody cage with pedicle screw fixation -- a finite element analysis. BMC Musculoskelet Disord 14:220
Zanjani-Pour S, Winlove CP, Smith CW, Meakin JR (2016) Image driven subject-specific finite element models of spinal biomechanics. J Biomech 49(6):919–925
Turkyilmaz I, Tumer C, Ozbek EN, Tözüm TF (2007) Relations between the bone density values from computerized tomography, and implant stability parameters: a clinical study of 230 regular platform implants. J Clin Periodontol 34(8):716–722
Kopperdahl DL, Morgan EF, Keaveny TM (2002) Quantitative computed tomography estimates of the mechanical properties of human vertebral trabecular bone. J Orthop Res 20(4):801–805
Frost HM (1994) Wolff’s Law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod 64(3):175–188
Matsukawa K, Yato Y, Imabayashi H, Hosogane N, Abe Y, Asazuma T, Chiba K (2016) Biomechanical evaluation of fixation strength among different sizes of pedicle screws using the cortical bone trajectory: what is the ideal screw size for optimal fixation? Acta Neurochir (Wien) 158(3):465–471
Acknowledgements
This work is supported by the Orthotek Laboratory, Shanghai University.
Author information
Authors and Affiliations
Contributions
Jia-Ming Liu and Yu Zhang contributed equally to this study and share the first authorship.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work is supported by the fund of Department of Science and Technology Program of Jiangxi Province, China (No. 20162BCB22022, 20162BCB23057).
Ethical approval
This study was approved by the medical research ethics committee of our hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liu, JM., Zhang, Y., Zhou, Y. et al. The effect of screw tunnels on the biomechanical stability of vertebral body after pedicle screws removal: a finite element analysis. International Orthopaedics (SICOT) 41, 1183–1187 (2017). https://doi.org/10.1007/s00264-017-3453-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3453-y