Abstract
Objective
The object of the present meta-analysis is to compare the effectiveness of transforaminal epidural steroid injection (TFESI) and interlaminar epidural steroid injection (ILESI) for treating patients with low back pain (LBP) secondary to lumbosacral radicular pain.
Methods
A systematic search was performed in the PubMed and Embase databases and the Cochrane Library for relevant literature published through January 2016. The randomized controlled trials (RCTs) and controlled observational studies were selected, which did not only compare TFESI with ILESI but also reported the available data. The Cochrane Collaboration’s Handbook and Newcastle-Ottawa Scale (NOS) were used for the methodological quality assessments of the RCTs and observational studies respectively. The meta-analysis was performed using the Revman 5.2 software.
Results
A total of 931 patients from nine RCTs and four observational studies were subjected to meta-analysis. In primary outcomes, the TFESI patients experienced superior pain relief compared with the TFESI patients in RCTs (P = 0.01), but not in observational studies (p = 0.63). The pooled data of RCTs showed that the TFESI group presented superior clinical results in terms of visual analogue scale (VAS) than the ILESI group (p = 0.0005). Moreover, the numeric rating scale (NRS) specifically favored TFESI in the RCTs (p < 0000.1). Similar functional improvement and oswentry disability index (ODI) score were observed between TFESI and ILESI in RCTs (P = 0.62). In secondary outcomes, meta-analysis of RCTs and observational studies revealed that there were no statistically significant differences between both groups in regard to procedure frequency, surgery rate, and ventral epidural spread.
Conclusions
According to the results of meta-analysis, TFESI to manage LBP provides superior short term pain relief and equal functional improvement when compared to ILESI. It has not shown a statistically significant difference between both groups with regard to procedure frequency, surgery rate, and ventral epidural spread.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP), which is the most common form of lumbosacral radicular pain, is the leading cause of disability [1–3]. Lumbar disc herniation (LDH) and spinal stenosis (SS) is the main aetiology of LBP [4–6]. Numerous modalities of treatment, including conservation approaches, traditional or minimally invasive surgery and interventional techniques have been commonly used for management of low back pain [7–10].
Among various procedural interventions for LBP, epidural steroid injection (ESI) is widely utilized for multiple indications including LBP with or without LDH, SS, and radiculitis [2, 11–13]. Via the lumbar transforaminal or interlaminar route, local anesthetics or steroids is injected into the site of pathology to limit inflammatory response from injures, impeding the nociceptor transmission and interrupting the pain spasm-cycle [14]. Several systematic reviews and meta-analyses have concluded that both epidural injections with steroids or with local anesthetic alone provided significant pain relief and functional improvement in managing chronic LBP secondary to LDH or SS, and the inclusion of steroids confers no advantage compared to local anesthetic alone [15–19]. Even though both transforaminal injection and interlaminar injection can deliver medication into the epidural space, there are important differences between the two approaches. The transforaminal approach is considered to transmit the medication more closely to the primary site of pathology, requiring less volume than the interlaminar route [20]. Moreover, multiple studies [12, 21–28] and systematic reviews [20, 29] have shown that lumbar transforaminal epidural steroid injections (TFESI) to treat lumbosacral radicular pain provides superior short-term (≤1 year) pain relief and functional improvement compared with interlaminar epidural steroid injections (ILESI).
In contrast, recent studies have suggested that TFESI was equivalent in pain relief and functional improvement to ILESI for the management of LBP secondary to lumbosacral radicular pain [30–35]. A few randomized controlled trials have focused on evaluating the efficacy of TFESI and ILESI, and the available studies are limited by their small sample size, thereby resulting in controversy over the clinical benefits of TFESI and ILESI. Although several systematic reviews concerning the clinical efficacy between TFESI and ILESI have been performed [20, 29, 34, 35], the valid data are not pooled and analyzed. In addition, a number of new RCTs have recently emerged. Therefore, the objective of this study is to compare the clinical outcomes between the two procedures by a meta-analysis.
Methods
Search strategy
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [36], this meta-analysis was performed for comparing TFESI and ILESI in treating patients with LBP. We performed systematic searches of the relevant literature contained in PubMed, Embase, and the Cochrane Library for studies published up to January 2016. The following keywords were used for the database research: “chronic low back”, “lower extremity pain”, “lumbar disc herniation”, “spinal stenosis”, “radiculitis”, “radicular pain”, “sciatica”, “epidural injections”, “epidural steroid”, “selective nerve root blocks”, “nerve root injections”, “nerve blocks”, “transforaminal”, “interlaminar”, and “interspinous”. The search was limited to English publications, although it was not limited to RCT and included all study designs. In addition, references from each article comparing two routes were also manually screened until no additional studies were found.
Inclusion and exclusion criteria
The following inclusion criteria for the articles selected were applied: 1) patients’ LBP were secondary to LDH or lumbar SS; 2) eligible RCT and observational studies that directly compare TFESI and ILESI; 3) at least one of the following data was presented: visual analogue scale (VAS), Oswentry disability index (ODI), numeric rating scale (NRS), effective pain and functional relief, procedure frequency, surgery rate, and ventral spread; 4) patients were followed-up at least two weeks. We excluded from the final analysis: 1) review articles, abstracts, letters and case report; 2) a lack of consistent use of fluoroscopic guidance; 3) absent of any outcome of interest and studies not available in English.
Data extraction
After duplicate publications were deleted, two investigators (GW and BC) independently screened all titles and abstracts related to inclusion criteria, and thereafter reviewed the full text when the study was considered to be relevant or not clear. Then, the following data was independently extracted from each eligible study: first author, publication date, number of patients, demographic information, intervention characteristics and all the outcome parameters which consisted of VAS, ODI, NRS, number of patients with effective pain and functional relief, procedure frequency, surgery rate, and ventral epidural spread. Any discrepancies were resolved through group discussion. Extracted data were entered into a standardized Excel file and checked by another author (CSZ).
Assessment of methodological quality
Two authors (GW and BC) independently utilized two different tools to assess the methodological quality of the included RCTs or observational studies. For RCTs, the Cochrane Collaboration’s Handbook was applied, and the following criteria: adequate sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other potential sources of bias [37]. For observational studies, the Newcastle-Ottawa scale (NOS) was used for the methodological quality assessment, with three aspects of selection, comparability, and outcome [38]. The quality of each study was graded as low (0–3), moderate (4–6), and high (7–9). Discrepant opinions were resolved by discussion and consensus.
Statistical analysis
The meta-analysis of RCT and observational studies was performed separately using Review Manager 5.2 software, when there were available data that could be combined. For continuous results, the mean and standard deviation (SD) were used to calculate the mean difference (MD) and 95 % confidence interval (CI). For dichotomous outcomes, such as in the number of events, the relative ratio (RR) and the 95 % CI were computed. The heterogeneity between studies was tested by using the I2 statistic and the χ2 test. When I2 statistic >50 % or P < 0.1, the data was considered to have substantial heterogeneity and a random-effects model was selected. Otherwise, a fixed-effects model was applied to estimate the overall summary effect size. A value of P < 0.05 was regarded as statistically significant. When heterogeneity existed, a sensitivity analysis was performed to evaluate the influence of the individual study on the pooled results by omitting every single study per iteration.
Results
Study selection
The primary literature search identified 956 potentially relevant titles. After discarding the duplicate studies and reading the titles and abstracts of the articles, 929 publications were excluded. The remaining study was further assessed for eligibility based on the full text articles. Although three studies included caudal epidural steroid injection as part of their research protocol [12, 27, 28], only data on TFESI or ILESI were included for analysis. Eventually, nine RCTs [21, 24, 26–28, 30–32, 39] and four observational studies [12, 22, 25, 33] were identified for data collection and critical assessment. The process of literature selection is presented in Fig. 1.
Study characteristics
The main characteristics of the included RCTs and observational studies are summarized respectively in Tables 1 and 2. The 13 eligible studies assessed a total of 931 participants (RCTs: 242 for the TFESI group, 263 for the ILESI group; observational studies: 128 for the TFESI group, 178 for the ILESI group), with ages ranging from 35 to 67 years. Plenty of patients received injections at L4-L5 or L5-S1 levels. In the majority of studies, VAS and NRS were applied to measure pain rating scores, and ODI was used to evaluate functional ability. A 50 % or greater pain relief from baseline on VAS was considered significant.
Risk of bias in included studies
The risk of bias of the included RCTs is presented in Fig. 2. All RCTs [21, 24, 26–28, 30–32, 39] had low risk of bias for random sequence generation, incomplete outcome data and selecting reporting. The method of concealment of allocation was reported in four studies [24, 26, 28, 31]. Four of the nine studies [26, 28, 31, 32] performed patient blinding, and all trials demonstrated assessor blinding, with the exception of one study [32]. Regarding other bias, two studies [21, 28] had been unclear. Four observational studies were assessed using NOS (Table 3). All of them had won seven stars, considered as relatively high-quality.
Primary outcomes
Pain relief
The available data regarding post-injection follow-up pain relief in both TFESI and ILESI group were provided in four RCTs [21, 27, 30, 32] and two observational studies [12, 33]. The outcome from the pooled analysis of four RCTs showed that patients in the TFESI group had a significant pain relief compared to those in the ILESI group (RR 1.28, 95 % CI 1.05–1.57, P = 0.01; Fig. 3), whereas this difference was not observed in two observational studies (RR 1.06, 95 % CI 0.82–1.38, p = 0.63; Fig. 3). There were no indications of statistical heterogeneity in RCTs (P = 0.27, I2 = 24 %) and the observational studies (P = 0.6, I2 = 0 %).
Data of VAS pain scores were available from four RCTs [24, 28, 32, 39] and two observational studies [22, 33]. Pooled estimates from four RCTs indicated that the TFESI patients had a significant reduction on VAS (MD −0.69, 95 % CI −1.08 to -0.30, p = 0.0005; Fig. 4), and significant heterogeneity was not observed (P = 0.64, I2 = 0 %). On the contrary, Pooled estimates from two observational studies showed that there was no significant difference between the two groups (MD −10.88 95 % CI −32.54–10.78, p = 0.32; Fig. 4), and it should be noted that significant heterogeneity was detected in the observational studies (I 2 = 99 %, P < 00001).
Furthermore, two RCTs [26, 27] and one observational study [25] evaluated the pain relief by the method of NRS between the TFESI group and the ILESI group. The pooled outcome from two RCTs showed that the TFESI patients experienced superior pain relief compared with the ILESI patients (MD −3.02, 95 % CI −4.03–-2.00, p < 0000.1; Fig. 5). No statistical heterogeneity was discovered (I 2 = 0 %, P = 0.56). The same effects were observed in one observational study (RR −2.70, 95 % CI −4.17 to -1.23, P = 0.0003, Fig. 5).
Functional improvement
Two RCTs [31, 32] and one observational study [22] reported data on functional improvement. Meta-analysis of the functional improvement events displayed no significant difference in both groups (RR 1.08, 95 %CI 0.79–1.47; P = 0.64, heterogeneity test, P = 0.2 and I2 = 38 %, Fig. 6). However, in one observational study, the functional improvement rate was significantly higher in the TFESI group (14/25) than in the ILESI group (6/24) (RR 2.24, 0.02, 95 % CI 1.03–4.86, P = 0.04, Fig. 6).
Data of ODI were available from four RCTs [26–28, 32] and one observational study [22]. We performed the meta-analysis to investigate the effects of functional improvement in both groups, even though the heterogeneity was high (P = 0.04, and I2 = 63 %). A random effect model of the pooled data revealed no significant difference (MD −1.10, 95 % CI −5.43–3.23, P = 0.62, Fig. 7). However, the observational study suggested that TFESI was more effective than ILESI in improving functional status (MD −22.4, 95 % CI −24.52 to -20.28, P < 00001, Fig. 7).
Secondary outcomes
Procedure frequency
Four RCTs [26–28, 30] and three observational studies [22, 25, 33] were included in the analysis of events of repeated injection. In RCTs, the meta-analysis indicated no significant difference between both groups in the rate of repeated injection (RR 0.78, 95 % CI 0.42–1.46, P = 0.43; Fig. 8). Similar results were shown in the observational studies (RR 1.07, 95 % CI 0.81–1.41, P = 0.62; Fig. 8). It should be noted that significant heterogeneity was detected in the RCTs (P = 0.05, I2 = 62 %) but not the observational studies (P = 0.58, I2 = 0 %).
Surgery rate
One RCT [28] and three observational studies [22, 25, 33] reported the number of patients that underwent surgery during the follow-up. The RCT suggested that neither TFESI (6.67 %) nor ILESI (10 %) resulted in lower rate of surgery when compared with each other (RR 0.67, 95 % CI 0.12–3.71, P = 0.64, Fig. 9). Moreover, there was no indication of statistical heterogeneity in three observational studies (P = 0.52, I2 = 0 %), and a fixed-effect model of the pooled data revealed no significant difference in surgery rate between the two groups (RR 0.72, 95 % CI 0.31–1.67, P = 0.44, Fig. 9).
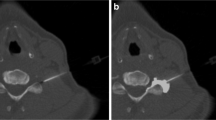
Ventral epidural spread
Three RCTs [21, 30, 39] presented data of ventral epidural spread. The pooled estimates did not identify statistically significant differences in the TFESI and ILESI groups by using random-effect model (RR 0.94, 95 % CI 0.74–1.19, P = 0.61, Fig. 10). There was significant heterogeneity between the included studies (P = 0.04, I2 = 69 %).
Sensitivity analysis
A series of sensitivity analysis were conducted to assess the stability of synthesis results and to identify sources of heterogeneity by removing every single study and analyzing the effect on overall results. According to the analysis results, there was not a particularly influential study among all selected studies, apart from the impact of Chai’s study [30] on procedure frequency. Exclusion of the Chai’s trial dramatically altered the results on procedure frequency, resulting in statistic difference between TFESI and ILSEI groups (RR = 0.55, 95 % CI 0. 34–0.88, P = 0.01; heterogeneity, I2 = 0 % and P = 0.37). This heterogeneity may have been due to differences of adjuvant therapies included individual patient exercise routines and analgesic drug therapy. Due to the small number of studies included, we did not undertake a publication bias assessment.
Discussion
This is a further meta-analysis of nine RCTs and four observational studies to evaluate the efficacy of TFESI and ILESI in the treatment of LBP with lumbosacral radicular pain. In the pooled study of around 931 participants from 13 studies, we chose VAS, NRS, and ODI to assess pain relief and functional improvement of patients post-operatively. The primary finding from our study consistently suggested that clinical results of the TFESI were significant different from those of the ILESI on pain relief, whereas equivalent functional improvement was observed in both groups. In terms of procedure frequency, surgery rate and ventral epidural spread, the results of this review showed that there was no significant difference between the two approaches.
To our knowledge, three systematic reviews [13, 34, 35] evaluating the clinical effectiveness of TFESI vs. ILESI have been published recently. What they found was in disagreement with the result of our meta-analysis which showed TFESI was clinically significantly superior to ILESI in the treatment of pain. Nevertheless, an equivalent functional improvement in both groups was revealed in our study and consistent with the result of the above three reviews. The difference may be partially ascribed to small sample size and different score systems in the previous three systematic reviews, which may result in publication bias. Moreover, transforaminal epidural injection considered as a specific route was the targeted delivery of the injectate to the typical site of nerve root compression, nevertheless the interlaminar epidural injection was regarded as a non-specific approach since the injectate is free to extend within the posterior epidural space with possible flow anteriorly, cephalad, and caudad [40, 41]. The SS or LDH patients usually were accompanied by the epidural ligaments fibrosis, scar tissue, hypertrophies of postlongitudinal ligaments, hypertrophied lateral recess, which may prevent interlaminar techniques from delivering injectate directly to the ventral aspect of the lumbar nerve root sleeve and the dorsal aspect of the disc herniation where inflammatory and mechanical reactions occur [23, 42, 43]. Whereas, the transforaminal technique was easier to deliver injectate into the ventral or anterior epidural space compared with the interlaminar technique. Thus, this might explain reasons that TFESI was more effective than ILESI in treating LBP originated from SS and LDH. Moreover, TFESI may be a more effective treatment method for reduction of radiating leg pain, and study of patients with radiating leg pain is worth conducting in the future. However, it was noted that the pooled data of two low-evidenced non-RCTs showed no significant difference in effective pain relief. With respect to the assessment of functional improvement on ODI, there was no significant difference between both groups in RCTs. However, the heterogeneity test showed significant values. A possible explanation is that the confounding variables, which included the baseline scores or disease status, opioid intake, physical therapy, and follow-up time, may have impacted the outcomes. Through sensitivity analysis, we found that the heterogeneity became insignificant after eliminating the Kamble’s trial [28], whereas this did not affect the results.
In secondary outcomes, an equal frequency of ESI through both TF and IL approaches was observed respectively in four RCTs [26–28, 30] and three observational studies [22, 25, 33] in our meta-analysis. On account of inconsistent subjective indications of repeated injection and the differences of adjuvant therapies, the results should be interpreted discreetly. Some studies [27, 30] suggested that repetitive injections could increase the clinical efficacy via TF or IL routes, which may be in part related to the cumulative effect of epidural steroid. The TFESI group did not have high repeat numbers of injections in spite of the more effective pain relief in TFESI group in our meta-analysis. Multiple studies also illustrated patients that had undergone LBP could reduce the rate of spinal surgery in the short term, when treated with epidural injections [11, 44–47]. In our studies, we evaluated the rates of surgery between the TFESI group and the ILESI group by the pooled data of three observational studies [22, 25, 33], and we did not find a significant difference in both groups. Similar results were observed in one RCT [28]. However, it is arguable that the follow-up time is inconsistent or there no sufficient time to make decisions regarding the effectiveness of LESI, especially in terms of preventing surgery. Besides, the limited long-term effectiveness of ESI was associated with numerous factors, including the duration of action of the steroid, procedure frequency, and disease progression of the patient.
The different clinical effects of the two techniques were in connection with ventral epidural spread of the injectate. The patients with TFESI had greater incidence of ventral epidural spread of injectate which corresponded to a better outcome when compared to interlaminar injection [23, 26, 48]. The targeted site of interface of the disk and the exiting root was often situated in the ventral epidural space, whereas the injectate from the interlaminar route may be prevented from diffusing from the posterior epidural space to the ventral epidural space. Nevertheless, our meta-analysis based on only three RCTs [21, 30, 39] suggested that the transforaminal approach was balanced with the interlaminar route for placing contrast into the ventral epidural space. This finding may be explained by the fact that the limited numbers of patients did not have sufficient power to detect differences in the ventral epidural spread between the two groups.
The results of this study may be applied to interventional pain management practices utilizing the superiority of TFESI over ILESI. Even though the adverse event rates of both approaches were not evaluated in our studies because of a few complications reported and the short-term follow-up time, the choice between ILESI and TFESI should be based on documented efficacy and effectiveness but not driven by safety concerns [49]. Moreover, this meta-analysis was conducted on RCTs and observational studies respectively, and all of them were of high quality. The RCT would minimize the recall and selection bias and provide strong evidence for TFESI in managing LBP with lumbosacral radicular pain in the short term (≤1 year). Meantime, the observational studies could further confirm the pooled results of the RCTs.
However, a number of potential limitations should be taken into account when interpreting our results. First of all, doses, injectate volumes or types of glucocorticoids, and analgesic drug therapy in each trial were not exactly the same, which is likely to have an impact on the results of our meta-analysis. Second, the limited numbers of RCTs, sample size, lack of long term follow-up, and appropriate outcome parameters maybe bring about inconsistencies in our results. Thirdly, we did not perform a publication bias assessment because of the relatively limited quantity of included studies. Finally, there is no consistency or standardization of indications (HVID and SS) and operation procedure utilized for either TFESI or ILESI between studies. Although the evidence may be imperfect, the results of this meta-analysis have implications for clinical practice, which can guide physicians and patients to make the appropriate choice for treating LBP with lumbosacral radicular pain by TFESI or ILESI.
Conclusions
As a result of our meta-analysis, the overall summary suggested that TFESI to manage LBP secondary to lumbosacral radicular pain results in superior short term pain relief but equal functional improvement when compared to ILESI. Regarding procedure frequency, surgery rate, and ventral epidural spread, it did not show a statistically significant difference between both groups. Sufficient, high-quality, prospective randomized controlled trials with large samples are required to further evaluate these two procedures.
References
Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R (2014) The global burden of low back pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:968–974. doi:10.1136/annrheumdis-2013-204428
Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, Bryce DA, Burks PA, Caraway DL, Calodney AK, Cash KA, Christo PJ, Cohen SP, Colson J, Conn A, Cordner H, Coubarous S, Datta S, Deer TR, Diwan S, Falco FJ, Fellows B, Geffert S, Grider JS, Gupta S, Hameed H, Hameed M, Hansen H, Helm S, Janata JW 2nd, Justiz R, Kaye AD, Lee M, Manchikanti KN, McManus CD, Onyewu O, Parr AT, Patel VB, Racz GB, Sehgal N, Sharma ML, Simopoulos TT, Singh V, Smith HS, Snook LT, Swicegood JR, Vallejo R, Ward SP, Wargo BW, Zhu J, Hirsch JA (2013) An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Phys 16:S49–S283
Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R (2003) Lost productive time and cost due to common pain conditions in the US workforce. JAMA 290:2443–2454. doi:10.1001/jama.290.18.2443
Cooper G, Lutz GE, Boachie-Adjei O, Lin J (2004) Effectiveness of transforaminal epidural steroid injections in patients with degenerative lumbar scoliotic stenosis and radiculopathy. Pain Phys 7:311–317
Pearson AM, Blood EA, Frymoyer JW, Herkowitz H, Abdu WA, Woodward R, Longley M, Emery SE, Lurie JD, Tosteson TD, Weinstein JN (2008) SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine 33:428–435. doi:10.1097/BRS.0b013e31816469de
Ng L, Chaudhary N, Sell P (2005) The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: a randomized, double-blind, controlled trial. Spine 30:857–862
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303:1259–1265. doi:10.1001/jama.2010.338
Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM, Fellows B, Hirsch JA (2012) Utilization of interventional techniques in managing chronic pain in the Medicare population: analysis of growth patterns from 2000 to 2011. Pain Phys 15:E969–E982
Manchikanti L, Helm Ii S, Singh V, Hirsch JA (2013) Accountable interventional pain management: a collaboration among practitioners, patients, payers, and government. Pain Phys 16:E635–E670
Manchikanti L, Pampati V, Falco FJ, Hirsch JA (2013) Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine 38:157–168. doi:10.1097/BRS.0b013e318267f463
Bicket MC, Horowitz JM, Benzon HT, Cohen SP (2015) Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. Spine J: Off J North Am Spine Soc 15:348–362. doi:10.1016/j.spinee.2014.10.011
Lee JH, Moon J, Lee SH (2009) Comparison of effectiveness according to different approaches of epidural steroid injection in lumbosacral herniated disk and spinal stenosis. J Back Musculoskelet Rehab 22:83–89. doi:10.3233/bmr-2009-0220
Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, Christo PJ, Ward SP (2012) Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Phys 15:E199–E245
Boswell MV, Hansen HC, Trescot AM, Hirsch JA (2003) Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Phys 6:319–334
Kaye AD, Manchikanti L, Abdi S, Atluri S, Bakshi S, Benyamin RM, Boswell MV, Buenaventura RM, Candido KD, Cordner H, Datta S, Doulatram G, Gharibo CG, Grami V, Gupta S, Jha SS, Kaplan ED, Malla Y, Mann DP, Nampiaparampil DE, Racz GB, Raj PP, Rana MV, Sharma ML, Singh V, Soin A, Staats PS, Vallejo R, Wargo BW, Hirsch JA (2015) Efficacy of epidural injections in managing chronic spinal pain: a best evidence synthesis. Pain Phys 18:E939–e1004
Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA (2015) Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res 473:1940–1956. doi:10.1007/s11999-014-3490-4
Meng H, Fei Q, Wang B, Yang Y, Li D, Li J, Su N (2015) Epidural injections with or without steroids in managing chronic low back pain secondary to lumbar spinal stenosis: a meta-analysis of 13 randomized controlled trials. Drug Des Dev Ther 9:4657–4667. doi:10.2147/dddt.s85524
Zhai J, Zhang L, Li M, Tian Y, Zheng W, Chen J, Huang T, Li X, Tian Z (2015) Epidural injection with or without steroid in managing chronic low back and lower extremity pain: ameta-analysis of ten randomized controlled trials. Int J Clin Exp Med 8:8304–8316
Bicket MC, Gupta A, Brown CH, Cohen SP (2013) Epidural injections for spinal pain: a systematic review and meta-analysis evaluating the “control” injections in randomized controlled trials. Anesthesiology 119:907–931. doi:10.1097/ALN.0b013e31829c2ddd
Parr AT, Diwan S, Abdi S (2009) Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: a systematic review. Pain Phys 12:163–188
Gupta R, Singh S, Kaur S, Singh K, Aujla K (2014) Correlation between epidurographic contrast flow patterns and clinical effectiveness in chronic lumbar discogenic radicular pain treated with epidural steroid injections Via different approaches. Korean J Pain 27:353–359. doi:10.3344/kjp.2014.27.4.353
Kawu AA (2012) Epidural steroid injection in patients with lumbosacral radiculopathy in Abuja, Nigeria. J Neurosci Rural Pract 3:121–125. doi:10.4103/0976-3147.98206
Lee JH, An JH, Lee SH (2009) Comparison of the effectiveness of interlaminar and bilateral transforaminal epidural steroid injections in treatment of patients with lumbosacral disc herniation and spinal stenosis. Clin J Pain 25:206–210. doi:10.1097/AJP.0b013e3181878f9e
Rezende R, Jacob Junior C, da Silva CK, de Barcellos ZI, Cardoso IM, Batista Junior JL (2015) Comparison of the efficacy of transforaminal and interlaminar radicular block techniques for treating lumbar disk hernia. Rev Bras Ortop 50:220–225. doi:10.1016/j.rboe.2015.02.016
Schaufele MK, Hatch L, Jones W (2006) Interlaminar versus transforaminal epidural injections for the treatment of symptomatic lumbar intervertebral disc herniations. Pain Phys 9:361–366
Gharibo CG, Varlotta GP, Rhame EE, Liu EC, Bendo JA, Perloff MD (2011) Interlaminar versus transforaminal epidural steroids for the treatment of subacute lumbar radicular pain: a randomized, blinded, prospective outcome study. Pain Phys 14:499–511
Ackerman WE 3rd, Ahmad M (2007) The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg 104:1217–1222. doi:10.1213/01.ane.0000260307.16555.7f, tables of contents
Kamble PC, Sharma A, Singh V, Natraj B, Devani D, Khapane V (2015) Outcome of single level disc prolapse treated with transforaminal steroid versus epidural steroid versus caudal steroids. Eur Spine J: Off Publ Eur Spine Soc, Eur Spinal Deformity Soc, Eur Sec Cervical Spine Res Soc. doi:10.1007/s00586-015-3996-9
Buenaventura RM, Datta S, Abdi S, Smith HS (2009) Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Phys 12:233–251
Ghai B, Bansal D, Kay JP, Vadaje KS, Wig J (2014) Transforaminal versus parasagittal interlaminar epidural steroid injection in low back pain with radicular pain: a randomized, double-blind, active-control trial. Pain Phys 17:277–290
Hashemi SM, Aryani MR, Momenzadeh S, Razavi SS, Mohseni G, Mohajerani SA, Esmilijah AA (2015) Comparison of transforaminal and parasagittal epidural steroid injections in patients with radicular low back pain. Anesthesiol Pain Med 5, e26652. doi:10.5812/aapm.26652v2
Rados I, Sakic K, Fingler M, Kapural L (2011) Efficacy of interlaminar vs transforaminal epidural steroid injection for the treatment of chronic unilateral radicular pain: prospective, randomized study. Pain Med (Malden, Mass) 12:1316–1321. doi:10.1111/j.1526-4637.2011.01213.x
Smith CC, Booker T, Schaufele MK, Weiss P (2010) Interlaminar versus transforaminal epidural steroid injections for the treatment of symptomatic lumbar spinal stenosis. Pain Med (Malden, Mass) 11:1511–1515. doi:10.1111/j.1526-4637.2010.00932.x
Benyamin RM, Wang VC, Vallejo R, Singh V, Helm Ii S (2012) A systematic evaluation of thoracic interlaminar epidural injections. Pain Phys 15:E497–E514
Chang-Chien GC, Knezevic NN, McCormick Z, Chu SK, Trescot AM, Candido KD (2014) Transforaminal versus interlaminar approaches to epidural steroid injections: a systematic review of comparative studies for lumbosacral radicular pain. Pain Phys 17:E509–E524
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6, e1000097. doi:10.1371/journal.pmed.1000097
Higgins JP, Green S ([updated March 2011]) Conchrane Handbook for Systematic Reviews of Interventions 5.1.0. The Cochrane Collaboration:Available: www.cochrane-handbook.org
Ottawa Hospital Research Institute. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.Available: http://www.ohri.ca/programs/clinicalepidemiology/oxford.asp
Candido KD, Raghavendra MS, Chinthagada M, Badiee S, Trepashko DW (2008) A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg 106:638–644. doi:10.1213/ane.0b013e3181605e9b, table of contents
Whitlock EL, Bridwell KH, Gilula LA (2007) Influence of needle tip position on injectate spread in 406 interlaminar lumbar epidural steroid injections. Radiology 243:804–811. doi:10.1148/radiol.2433060983
Andreisek G, Jenni M, Klingler D, Wertli M, Elliott M, Ulbrich EJ, Winklhofer S, Steurer J (2013) Access routes and reported decision criteria for lumbar epidural drug injections: a systematic literature review. Skelet Radiol 42:1683–1692. doi:10.1007/s00256-013-1713-5
Rosenberg SK, Grabinsky A, Kooser C, Boswell MV (2002) Effectiveness of transforaminal epidural steroid injections in low back pain: a one year experience. Pain Phys 5:266–270
Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, Slaten WK, Rao S (2002) Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehab / Assoc Acad Phys 81:898–905. doi:10.1097/01.phm.0000034953.43372.72
Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, Goette K (2000) The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am 82-a:1589–1593
Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lenke LG, Bridwell KH (2006) Nerve root blocks in the treatment of lumbar radicular pain. A minimum five-year follow-up. J Bone Joint Surg Am Vol 88:1722–1725. doi:10.2106/jbjs.e.00278
Yang SC, Fu TS, Lai PL, Niu CC, Chen LH, Chen WJ (2006) Transforaminal epidural steroid injection for discectomy candidates: an outcome study with a minimum of two-year follow-up. Chang Gung Med J 29:93–99
Ploumis A, Christodoulou P, Wood KB, Varvarousis D, Sarni JL, Beris A (2014) Caudal vs transforaminal epidural steroid injections as short-term (6 months) pain relief in lumbar spinal stenosis patients with sciatica. Pain Med (Malden, Mass) 15:379–385. doi:10.1111/pme.12318
Kozlov N, Benzon HT, Malik K (2015) Epidural steroid injections: update on efficacy, safety, and newer medications for injection. Minerva Anestesiol 81:901–909
El-Yahchouchi CA, Plastaras CT, Maus TP, Carr CM, McCormick ZL, Geske JR, Smuck M, Pingree MJ, Kennedy DJ (2015) Adverse event rates associated with transforaminal and interlaminar epidural steroid injections: a multi-institutional study. Pain medicine, Malden. doi:10.1111/pme.12896
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interests and the work was not supported or funded by any drug company.
Rights and permissions
About this article
Cite this article
Wei, G., Liang, J., Chen, B. et al. Comparison of transforaminal verse interlaminar epidural steroid injection in low back pain with lumbosacral radicular pain: a meta-analysis of the literature. International Orthopaedics (SICOT) 40, 2533–2545 (2016). https://doi.org/10.1007/s00264-016-3220-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3220-5