Abstract
Aim of study
A prospective study to evaluate the results of monosegmental fixation; fixation of the fractured level with the adjacent vertebra sharing the same disc, in selected types of lumbar and thoracic fractures. This technique aims at saving motion levels by fusion of the only affected motion segment without sacrificing other levels.
Methods
Forty patients enrolled in this study between August 2011 and October 2013. The inclusion criteria were recent thoracic or lumbar vertebral fractures (less than 2 weeks). The fracture involves only one of the end plates of the vertebrae (either the superior or the inferior). The other end plate and both pedicles should be intact. The exclusion criteria were cervical fractures, fractures that include both end plates or pedicles of the vertebra, fracture dislocation, and load sharing classification score more than seven. All patients underwent monosegmental fixation with pedicle screw fixation. Eight patients were supplemented with interbody grafts. Radiological evaluation was done to assess local kyphosis angle, degree of compression of the anterior column, the degree of comminution, retropulsed fragment, neural canal compromise, integrity of the affected end plate, exclusion of pedicle fracture, and most important to assure that only one end plate is affected. All patients were assessed neurologically according to Frankel grading system. Patient were assessed by Denis pain scale and Denis work scale.
Results
The age of the patients was of a mean of 34.5 years old. All patients were Frankle E at time of presentation and remained the same post-operative. The mean operative time from incision time to end of skin closure was 74.2 min. The mean blood loss was 230 ml. The pre-operative degree of local kyphosis; was of a mean 8.22°. This was improved to 2.25° at the immediate postoperative x-rays. At two years follow up, the loss of correction was of a mean 0.85° which was insignificant. The pre-operative percentage of height lost improved from a mean of 56.05 % to post-operative mean of 90.125 %. At the end of follow up, no pseudoarthrosis cases or metal failure were noticed.
Discussion
Thoracic and lumbar fractures are common in young adults. Surgical treatment offers early rehabilitation and preserves spine alignment. Monosegmental fixation technique in selected types of dorsal and lumbar fractures offers spine stability and preserves motion segments. It fuses only one motion segment that is prone for later instability or deformity. Reconstrcution of the anterior column can be achieved through TLIF approach in combination of monosegmental fixation to achieve 360° fusion.
Conclusion
Monosegmental fixation is an effective technique. It can save motion segments in young patients with adequate spine stability and good functional outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary goal of treatment of the thoracolumbar fracture is keeping patients alive, protecting from further neural damage, obtaining stability by reconstructing anatomical alignment of spinal columns, and returning patients to the workplace through early mobilization and rehabilitation. These fundamental principles have not been changed for decades. However, there has been an ongoing controversy in determining treatment methods until now [1]. Different schools of thoughts for each modality, ranging from conservative management with reduction by pillow and extending today to anterior/posterior instrumentation systems for fixation, have proved that neither is an ideal method and much more needs to be done to reach an ideal modality of management [2, 3].
Transpedicular fixation by pedicle screws became the gold standard fixation technique for thoracic and lumbar fractures. Each fracture morphology and ability to withstand stresses dictates the appropriate approach of treatment. A common opinion is to obtain the most stable fixation by fixing as few vertebrae as possible with neural canal decompression [4].
This study offers the results of a limited intervention; monosegmental (one level) fixation, for certain common types of thoracic and lumbar vertebral fractures.
Patients and methods
This is a prospective study that was done between August 2011 and October 2013. A written consent was taken from every patient enrolled in this study, and the research was done according the ethics committee rules in our institute.
It enrolled 40 patients with thoracic or lumbar vertebral fractures. All the patients underwent monosegmental (the fractured vertebra and adjacent one only) posterior fixation and fusion.
The inclusion criteria were recent thoracic or lumbar vertebral fractures (less than 2 weeks). The fracture involves only one of the end plates of the vertebrae (either the superior or the inferior). The other end plate and both pedicles should be intact. This can be compression, burst or flexion distraction injuries.
According to Denis classification these are compression fractures (type B - involvement of superior end plate, type C - inferior end plate), burst fractures (type B: fracture of the superior end-plate. Type C: fracture of the inferior end-plate, flexion distraction injuries (one level ligamentous injury) [5].
And according to AO classification it includes subtype A1 (wedge or impaction fracture), subtpe A3 (incomplete burst fracture), subtype B2 (ligamentous disruption with or without osseous involvement) [6].
All the fractures according to the load sharing classification score is less than seven [7].
The exclusion criteria were cervical fractures. Fractures that include both end plates or pedicles of the vertebra, fracture dislocation, and load sharing classification score more than seven.
No osteoporotic fractures were included in this study.
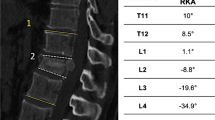
All patients were assessed neurologically according to Frankel grading system. Local kyphosis angle and degree of compression of the anterior column (anterior vertebral lost height) are assessed in the plain x-rays. Axial and sagittal CT scan cuts were mandatory to assess the degree of comminution, retropulsed fragment, neural canal compromise, integrity of the affected end plate, exclusion of pedicle fracture and most important to assure that only one end plate is affected. MRI is done if the patient has neurological impairment or suspicion of posterior ligamentous complex injury.
The procedure was done under general Anesthesia in prone position. The level of fracture was checked by image intensifier before incision to minimize the wound. Posterior midline approach with subperiosteal muscle dissection to the tip of transverse process was carried out. Insertion of the top loading pedicle screws in the affected vertebra is toward the intact endplate; Cephalo caudal direction if the superior endplate is affected or caudal to cephalic direction if the lower endplate is fractured. The other vertebra fixed is the one shares the same disc with the fractured end plate. The contoured rod was mounted to the screws. Distraction was done for ligamentotaxis, indirect decompression, and reduction of the lost height. Correction of local kyphosis and reduction of the vertebral height was checked by an image intensifier.
Anterior column support can be achieved through trans foraminal approach. Trans foraminal disc excision and interbody grafting with or without a cage can add to the anterior column support especially if the anterior vertebral height was not regained. In the presence of neurological impairment posterior laminectomy as a decompression procedure can be added.
Posterior and posterolateral fusion was done by autogenous bone graft.
Second day ambulation was allowed in a brace. Post-operative x-ray was done for assessment of accuracy of pedicle screws placement, deformity correction and restoration of vertebral body height.
Patient discharge was planned 48 hours post-operative. The follow up schedule was 21 days post-operative for removal of stitches, six weeks post-operative, and every three months till the end of follow up.
The patient is assessed clinically and radiologically for maintenance of reduction, metal failure, and progress of fusion.
Patients were assessed by Denis pain scale [8] and Denis work scale [9] at two year follow up (Fig. 1).
Results
The age of the patients enrolled in this study ranged from 19 to 52 years old with a mean of 34.5 years old. Seventeen patients were due to motor car accidents, 15 patients due to fall from height, and eight patients due to sport injuries.
Nineteen patients had compression fracture (15 patients type B, four patients type C), 16 patients had burst fracture (12 patients type B, four patients type c), and five patients had flexion distraction injuries. Sixteen patients had fractures at the thoracolumbar junction (between T10-L2), 11 patients at lumbar region, seven patients at the dorsal region, and six patients had noncontiguous spine fractures, none of them were in the cervical region. Fourteen patients had other limb fractures.
All patients were neurologically intact (Frankle E) at time of presentation.
All patients underwent monosegmental fixation and fusion. Five patients were supplemented with interbody cage and three patients with interbody graft through trans foraminal approach. The mean operative time from incision time to end of skin closure was 74.2 minutes. The mean blood loss was a of mean 230 ml.
The delay to surgery was a mean of three days, and hospital discharge was a mean of four days. This delay was observed in the poly trauma patients due to management of other non spinal injuries. In patients with only spine fracture the hospital discharge was 48 hours post-operative except for three patients due to prolonged wound discharge.
All patients remained Frankle E post-operative. Patients without contraindications for weight bearing; as lower limb fractures; were able to ambulate second day post-operative with a brace. The brace was used for the first month of the post-operative period.
The average follow up period was 28.4 months. Patients with follow up less than 24 months were excluded from the study.
The pre-operative degree of local kyphosis; the angle between the upper end plate of the upper vertebra and lower end plate of the lower vertebra to be fixed; was of a mean 8.22°. This was improved to 2.25° at the immediate post-operative x-rays. At two years follow up, the loss of correction was of a mean 0.85° which was insignificant and did not affect the final outcome.
The percentage of height lost was measured in relation to the lower vertebra multiplied by 100 (anterior height of the fractured vertebra in the lateral view x-ray divided by the anterior height of the vertebra below multiplied by 100). The pre-operative percentage of height lost improved from a mean of 56.05 % to post-operative mean of 90.125 %. At the end of follow up, no pseudoarthrosis cases or metal failure were noticed.
According to Denis functional back pain scale at two years follow up, 13 patients were P1 (no pain), 16 patients were P2 (minimal pain with no need for medication), nine patient were P3 (moderate pain with occasional use of medication), and two patients were P4 (moderate to severe pain with constant use of medications). No patients were P5 (severe pain with chronic use of medication).
According to Denis work scale at one year follow up, 12 patients were W1 (return to previous work heavy duty or physical activities), 15 patients were W2 (Able to return to previous work, sedentary, or return to heavy work with restraint), eight patients were W3 (unable to return to previous work but works in another function), two patients were W4 (unable to return to work full time), and three patients were W5 (unable to return to work). The pain, need for medications, and decreased ability to work were observed in polytraumatized patients and in patients with pre-operative history of back pain (Table 1 and Fig. 2) (Fig. 3).
Discussion
Traumatic thoracic and lumbar factures mostly occur in young and middle age active people. Non-operative treatment of fractures without neurologic deficits with bed rest, postural reduction, and bracing has been proposed, with variable results [2]. Frankel et al. [10] reported that treatments using postural reduction would be enough and that it would be possible to make patients mobile after restoring their stability by long-term relaxation. This is usually followed by long term rehabilitation and a considerable lag to return to their normal life, activity, and work capabilities. Jacobs et al. [11] performed comparative studies between surgical methods and temporizing methods, and found that surgical methods were better than temporizing ones at overcoming fractures, restoring neurological functions, moving patients early, and decreasing complications.
One of the main concerns of spine surgeons is to save motion segments. This can be achieved either by motion preservation techniques or by limitation of the number of fused motion segments without affection of spine alignment and stability.
According to AO classification of lumbar and dorsal spine fractures, subtype A1 (wedge or impaction fracture) and subtpe A3 (incomplete burst fracture) are commonly encountered. They involve fracture of only one endplate of the vertebra. These fractures are considered unstable if there is loss of height more than 50 %, local kyphosis more than 30°, retropulsed fragment more than 50 % or injury of posterior ligamentous complex [1]. The classic treatment for such fractures—with load sharing score less than 7—is to fix one level above and one level below the affected vertebra.
The risk of kyphosis is due to gradual settling of the discs into the fractured endplates and vertebral body [12]. Many authors studied the changes in the disc space adjacent to the fractured end plate and they came to a conclusion that these changes are responsible for the late progressive kyphosis which occurs in fractures treated conservatively or surgically after removal of implants [13].
Mono segmental posterior fixation and fusion of the abovementioned types of fractures means to fix only one level; single motion segment that shares the fractured end plate. This motion segment is the one at risk for late kyphosis due to future changes that may occur in this disc. If the pedicle screws have good anchorage in the unaffected part of the fractured vertebra and the other endplate is intact, there is no need to fix or fuse the motion segment which shares the intact end plate.
Monosegmental fixation can save motion segments in this young active population. Also on long term aspects, decreasing the number of fused levels decreases the risk of adjacent segment disease [14]. This is more pronounced in cases of noncontiguous spine fractures.
This technique can be considered as a limited intervention if compared to the traditional treatment. It allows early mobilization, adequate fixation, and less pain. It complies a smaller incision and a shorter hospital stay, therefore, earlier rehabilitation and better cost effectiveness.
Wang et al. [15] in their study about recurrence of kyphosis after short posterior fixation in thoracolumbar burst fractures noticed the importance of anterior wedge angle—vertebral body height—rather than the segmental angular parameters. They emphasized the need for anterior column reconstruction if the anterior vertebral height was not regained. Anterior reconstruction nowadays can be done through TLIF or PLIF approaches [16, 17]. These approaches can be easily applied with monosegmental fixation to ensure 360° fusion and prevent late kyphosis. Our cases show that interbody cages can be used safely without sinking if the endplate is not comminuted. In cases of multiple fracture lines extending to the end plate—comminuted end plate—we think it is more wise to use only bone graft to reconstruct the anterior column.
At the end of follow up of this study, there was no significant loss of post-operative correction. There was no single case of metal failure. The functional outcome of the patients enrolled in this study was satisfactory for the patients and surgeons.
Conclusion
Monosegmental fixation is an effective technique for commonly encountered types of thoracic and lumbar fractures. It can save motion segments in young patients with adequate spine stability and good functional outcomes.
References
Kim B-G, Dan J-M, Shin D-E (2015) Treatment of thoracolumbar fracture. Asian Spine J 9(1):133–146. doi:10.4184/asj.2015.9.1.133
Dai LY, Jiang LS, Jiang SD (2008) Conservative treatment of thoracolumbar burst fractures: a long-term follow-up results with special reference to the load sharing classification. Spine (Phila Pa 1976) 33:2536–2544
Shin TS, Kim HW, Park KS, Kim JM, Jung CK (2007) Short-segment pedicle instrumentation of thoracolumbar burst-compression fractures: short term follow-up results. J Korean Neurosurg Soc 42:265–270
Singh R, Rohilla RK, Kamboj K, Magu NK, Kaur K (2014) Outcome of pedicle screw fixation and monosegmental fusion in patients with fresh thoracolumbar fractures. Asian Spine J 8(3):298–308. doi:10.4184/asj.2014.8.3.298,
Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 8(8):817–31
Reinhold M, Audigé L, Schnake KJ, Bellabarba C, Dai L-Y, Oner FC (2013) AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J 22(10):2184–2201. doi:10.1007/s00586-013-2738-0
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine 19(15):1741–1744
Denis F, Armstrong GW, Searls K, Matta L (1984) Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res 189:142–149
Liu S, Li H, Liang C et al (2009) Monosegmental transpedicular fixation for selected patients with thoracolumbar burst fractures. J Spinal Disord Tech 22:38–44
Dickson JH, Harrington PR, Erwin WD (1978) Results of reduction and stabilization of the severely fractured thoracic and lumbar spine. J Bone Joint Surg 60A:799–805
Jacobs RR, Casey MP (1984) Surgical management of thoracolumbar spinal injuries. Clin Orthop Relat Res 189:22–35
Shin T-S, Kim H-W, Park K-S, Kim J-M, Jung C-K (2007) Short-segment pedicle instrumentation of thoracolumbar burst-compression fractures; short term follow-up results. J Korean Neurosurg Soc 42(4):265–270. doi:10.3340/jkns.2007.42.4.265
Cumhur OF, Robert R, Van DR, Lino MP, Wouter JA, Abraham JV (1998) Changes in the disc space after fractures of the thoracolumbar spine. JBJS Br 80b(5):833–839
Epstein NE (2015) Adjacent level disease following lumbar spine surgery: a review. Surg Neurol Int 6(Suppl 24):S591–S599. doi:10.4103/2152-7806.170432
Wang X–Y, Dai L-Y, Xu H-Z, Chi Y-L (2008) Kyphosis recurrence after posterior short segment fixation in thoracolumbar burst fractures. J Neurosurg 8(3):246–254. doi:10.3171/SPI/2008/8/3/246
Schmid R, Krappinger D, Blauth M, Kathrein A (2011) Mid-term results of PLIF/TLIF in trauma. Eur Spine J 20:395–402
Schmid R, Krappinger D, Seykora P, Blauth M, Kathrein A (2010) PLIF in thoracolumbar trauma: technique and radiological results. Eur Spine J 19:1079–1086
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ibrahim, F.M.F., Abd EL-rady, A.ER.M. Mono segmental fixation of selected types of thoracic and lumbar fractures; a prospective study. International Orthopaedics (SICOT) 40, 1083–1089 (2016). https://doi.org/10.1007/s00264-016-3152-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3152-0