Abstract
Purpose
Many institutions perform peripheral femoral and/or sciatic nerve blocks for analgesia after total knee arthroplasty. The aim of the present investigation was to compare the analgesic effect of an intermittent sciatic block (boluses on demand only) with a continuous infusion.
Methods
One hundred and forty patients receiving a femoral and a sciatic nerve block (SNB) by catheter were assessed. The femoral catheter was infused continuously in both groups. In the continuous group (n = 70), the sciatic catheter was used continuously as well. In the intermittent group (n = 70), after a single injection of 20 ml ropivacaine 0.75 %, injections into the sciatic catheter were performed on demand only. Frequency of injections, ventral and dorsal numerical pain scores (NRSs) of the knee, functional outcome (degree of flexion/extension) and additional opioid requirements were assessed during the post-operative period.
Results
In both groups, dorsal and ventral NRSs were below 3 at rest and below 5 during mobilisation over the complete period of assessment. Differences between the groups could not be observed. The cumulative number of supplemental injections into the sciatic catheter was higher in the intermittent group (52) compared with the continuous group (24; p < 0.05). Groups did not differ from each other with regard to functional outcome and opioid consumption.
Conclusions
The use of a sciatic block performed as intermittent bolus injection on demand only did not affect post-operative outcome parameters with regard to pain scores, functional outcome or opioid requirements. This approach might therefore be considered as an alternative to a continuous infusion concept.
ClinicalTrials.gov Identifier: NCT01843153
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is an operation associated with severe post-operative pain. Therefore, many institutions perform peripheral nerve blocks in order to reduce pain [1–3]. To provide analgesia, several different approaches have been described, including single-shot, intermittent and continuous techniques as well as femoral nerve blocks (FNBs) or sciatic nerve blocks (SNBs) alone or in combination. There is strong evidence that a continuous femoral nerve block (continuous FNB) seems to be of advantage with regard to pain scores and time to fulfilled discharge criteria [2–6]. However, the level of evidence described in the literature for a combination of a continuous FNB with an SNB seems to be moderate [1, 7–9]. Moreover, the concept of providing two blocks is more complex and leads to additional costs, especially, if a continuous post-operative regimen is planned for several days.
In our institution, a combination of FNB and SNB catheters has been routinely performed since September 2010. A continuous infusion is established via the femoral catheter post-operatively while the sciatic catheter is used on demand only (in case of pain in the posterior part of the knee in spite of a sufficient effect of the femoral nerve block). However, in a retrospective study including 208 patients treated with this regimen, a relatively high percentage of patients required one or more injections into the sciatic catheter: 43 % on post-operative day one and 21 % on day two, respectively [10]
The aim of the present investigation was, therefore, to assess if the intermittent concept performed in our department is able to provide an analgesic effect which is equivalent to a continuous infusion. The primary endpoint was the difference between groups with regard to pain at rest in the dorsal part of the knee during the post-operative time course. Secondary endpoints were pain at rest in the ventral part of the knee, pain during mobilisation, opioid consumption, frequency of injections into the sciatic catheter and functional outcome (degree of flexion/extension of the knee).
Methods
Patients and methods
The study design was randomised, unblinded, prospective and monocentre (ClinicalTrials.gov Identifier: NCT01843153). After obtaining approval from the local ethics committee (Ethikkommission der Ärztekammer Nordrhein, Düsseldorf, Germany, April 19th 2013, No. 2012049, chairman F. Pluisch) and patients’ written informed consent, we included 140 patients, American Society of Anesthesiologists Physical Status I-III, undergoing elective total knee arthroplasty (TKA) in general anaesthesia combined with an FNB and SNB, from April 2013 to October 2014.
Patients were excluded from the study if one or both of the blocks were not feasible or did not provide sufficient analgesia in the post–anaesthesia care unit (PACU). In case of accidental removal of one of the catheters, removal because of catheter-related complications or re-operation during the post-operative time course, a direct comparison of pain scores, opioid requirements or functional outcome of these patients with the other cases was not possible any longer. Therefore, data of these patients could be analysed only before the incident during the time period with catheters providing adequate analgesia. However, after the loss of one of the catheters or after a re-operation, the measurements had to be stopped.
Nerve blocks
Patients were premedicated orally with midazolam 7.5 mg and ibuprofen 800 mg one hour before surgery. Standard monitoring (electrocardiogram, pulse oximeter, blood pressure cuff) and intravenous access were established and patients were placed in the supine position. The puncture sites were identified as described below, disinfected and draped sterilely. In all cases, nerve blocks were performed using a nerve stimulator (Stimuplex HNS 11; B. Braun, Melsungen, Germany) together with 60-mm (FNB) and 150-mm (SNB) needles (Plexolong/Meier Nanoline Sprotte Spezial; Pajunk, Geisingen, Germany), respectively.
The FNB was performed 1–2 cm below the inguinal ligament and 1–2 cm lateral to the femoral artery. Muscle twitches of the quadriceps femoris muscle with a current of less than 0.6 mA were considered as indicative of adequate needle placement. After 30 ml of prilocaine 1 % had been injected, the catheter was placed 5–8 cm deeper than the distance from skin to the tip of the needle. Prilocaine was used in order to achieve a fast onset of the FNB, thereby reducing the discomfort during SNB puncture.
For the SNB, the anterior approach was used in order to keep the patient in the supine position for patient comfort and efficiency reasons. The puncture site was 5 cm below of the FNB (Fig. 1). A line was drawn from the anterior superior iliac spine to the pubic tubercle and divided into thirds. A second line was drawn, parallel to the first, medial from the cephalad aspect of the greater trochanter. Then, a third line was drawn perpendicular from the medial third of the first line to intersect the second line. The intersection usually was located over the lesser trochanter of the femur, representing the point of initial needle insertion. Initially, the current was set to 3–5 mA and was reduced gradually until muscle twitches could be observed with values less than 1.0 mA. After injection of 20 ml ropivacaine 0.75 %, the catheter was placed 5–8 cm deeper than the distance from skin to the tip of the needle.
Identification of the puncture site for the sciatic block. Yellow line sciatic nerve. Upper red line connection between superior anterior iliac spine and pubic tubercle. Lower red line parallel to the upper red line, beginning medial from the cephalad aspect of the greater trochanter. Green line perpendicular line from the medial third of the upper red line to intersect the lower red line. White arrow puncture site. Details are explained in the text
Femoral or sciatic blocks were regarded as not feasible, if the nerve could not be identified with the nerve stimulator using the technique mentioned above.
Induction and maintenance of anaesthesia
General anaesthesia was induced with propofol 2 mg kg−1, fentanyl 0.1 mg and rocuronium 0.3 mg kg−1. Following intubation of the trachea, patients’ lungs were mechanically ventilated with an oxygen/air mixture. Anaesthesia was maintained with remifentanil, 0.1 μg kg min−1 and sevoflurane 0.7-2 vol. %, according to the patients’ needs.
Post-operative analgesia and study groups
For post-operative analgesia, a multimodal approach was used. In the post–anaesthesia care unit (PACU), 20 ml of ropivacaine 0.375 % were injected into the femoral catheter in order to provide long-lasting analgesia. In case of a pain score of more than 3 on a numerical rating scale (NRS) from 0 to 10 (0, no pain; 10, worst pain imaginable), patients received piritramide intravenously, titrated until a pain score of <4 was reached. At the general ward, all patients received sustained-release ibuprofen 2 × 800 mg orally, or in case of contraindications, metamizole 4 × 1,000 mg orally. Additionally, ropivacaine 0.2 % was continuously infused with 8 ml/h via the femoral catheter until the 2nd postoperative day. All patients were visited by the acute pain service 2 times per day (08:00 and 15:00) and on demand, if necessary. Patients with preoperative opioid requirement received their medication in addition to the study medication.
After arrival in the operation theatre, patients were randomised into two groups. In the continuous group (CON group), they received a continuous infusion of ropivacaine 0.2 % at 6 ml/h via the sciatic catheter in addition to the femoral catheter. In the intermittent group (INT group), only the femoral catheter was used continuously.
In case of an NRS above 3 at rest or 4 during mobilisation, ropivacaine 0.2 % (10 ml) was injected into one or both of the catheters, depending on the localisation of the pain. If the patient could localise the pain (anterior or posterior part of the knee), the respective catheter was chosen. If the patient was not able to localise the pain, ropivacaine 0.2 % was injected into both catheters. In case of insufficient pain relief, another bolus of ropivacaine 0.2 % (10 ml) was administered. In case of inadequate pain relief afterwards, oxycodone 10 mg orally, 2 times daily was administered orally in addition to the regional analgesia. On the second post-operative day, the continuous infusions of the catheters were stopped if NRS was below 4 at rest and below 5 during mobilisation. Simultaneously, an oral analgesic regimen consisting of oxycodone 2 × 10 mg and ibuprofen 2 × 800 mg daily was started. In case of higher NRSs, the catheters were used until the third post-operative day.
Patients were mobilised by standing before the bed on the day of surgery. On the first post-operative day, patients were additionally mobilised by movements on a motor-operated continuous passive motion device (Artromot® K1 classic; Ormed, Freiburg, Germany) with a degree of 30° flexion. Walking was performed on the second post-operative day.
Measurements
Measurements of both catheters included NRS at rest and during mobilisation during all visitations, additional injections into the SNB, additional opioid consumption, number of blocks providing insufficient analgesia, number of complications such as infection, nerve injury, haematoma, or accidental removal, functional outcome defined as degree of flexion/extension of the knee at the fifth post-operative day.
Statistical analysis
Data were analysed using the software package Sigma Plot 12.3 for Windows (Systat Software, Chicago, IL). The primary endpoint was the pain at rest.
Normally distributed data were analysed with the t-test (height, weight). Not normally distributed data (NRS scores, functional outcome, and age) were compared by the Mann–Whitney rank sum test or with the Fisher exact test (number of injections, gender). All tests were performed two-tailed with a significance level of α = 0.05.
We calculated the sample size prospectively based on the results of our previous study (Soltesz et al. [10]): aiming at a power of 90 % to detect a difference of NRS ≥2 (mean 3, standard deviation 3) at the 5 % level, 46 patients per group were required. In order to compensate for possible dropouts caused by accidental removal, technical problems or insufficient effect of one of the blocks, 70 patients per group were randomised.
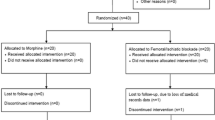
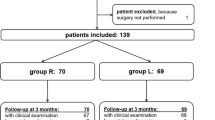
Results
One hundred and forty patients were randomised. Seven patients out of the CON group and five patients out of the INT group had to be excluded from the study because one or both of the nerve blocks could not be performed. Additionally, during the post-operative time course, the absolute numbers of patients with catheters decreased to 108 until the second post-operative day because of the following reasons: in six patients out of the CON group measurements had to be stopped prematurely because of accidental disconnection and subsequent removal of one of the catheters, and in one case because the patient requested removal before the second post-operative day. In the INT group, one patient was excluded because of surgical bleeding that needed revision, one sciatic catheter was removed because of suspected nerve injury, two patients requested removal, and in nine cases one of the catheters disconnected prematurely. The suspected nerve injury was not confirmed and all patients recovered completely without long term sequelae.
With regard to demographic data, differences between groups were not observed. Details of the selection process and patient characteristics are presented in Fig. 2 and Table 1, respectively
The absolute numbers of patients with catheters during the complete postoperative time course are displayed in Table 2 and Fig. 3. In the majority of the cases, the pain therapy via catheters could be terminated as scheduled on the second post-operative day. The frequency of termination was similar in both groups. Thirty-seven patients in each group required regional analgesia until the third post-operative day.
Pain scores
With regard to the primary endpoint, median NRS scores in the dorsal part of the knee at rest were 0–1 (0–3.5) in the CON group and 0–1 (0–4) in the INT group (median (25th/75th percentile; Table 2). Ventral median NRS scores in the knee at rest as well as dorsal and ventral NRS scores during mobilisation were below 3 at rest and below 5 during mobilisation over the complete period of assessment in both groups (Table 2). With regard to all NRS scores differences between the groups could not be observed.
In the INT group, the number of supplemental injections into the sciatic catheter was higher compared to the CON group from the day of surgery until the morning of the second post-operative day and at the morning of the third post-operative day. Conversely, at the afternoon of the second post-operative day, the number of additional injections was higher in the CON group (4 vs. 2; p < 0.05; Fig. 3). The cumulative number of injections was 24 in the CON group versus 52 in the INT group, respectively. In both groups, the number of injections initially increased during the time period of observation with its peak at the first post-operative day.
Functional outcome
Pre-operatively, a deficit of extension of 5° (0/10) was observed in both groups. The values for flexion were 100° (90/110) for the CON group, and 100° (90/120) for the INT group (median [25th/75th percentile]; not significant). On the fifth post-operative day, extension was 0° (0/0) in both groups. Flexion was 80° (70/90) in the CON group and 80° (65/90) in the INT group (median [25th/75th percentile]; not significant).
Opioid consumption
Thirty-one patients (49 %) in the CON group and 28 patients (47 %) in the INT group required supplemental analgesia with oxycodone 10 mg at least once. Differences with regard to cumulative dose, frequency or duration of opioid administration were not observed between the groups (Table 3).
Discussion
The results of this study suggest that analgesic regimens for TKA consisting of a continuous femoral nerve block combined with either a continuous sciatic nerve block or an intermittent sciatic injection on demand are able to provide sufficient and equipotent analgesia at rest and during mobilisation. With regard to the intensity of pain as the main outcome parameter, no differences were observed. Moreover, functional outcome measured as degree of flexion/extension was similar in both groups.
A methodological strength of the study is the separate assessment of pain in the ventral and the dorsal part of the knee. Thus, the effect of the sciatic block and the femoral block could be evaluated isolated from each other. To our knowledge, all other studies dealing with this topic did not perform this separation and are therefore not able to discriminate between pain resulting from insufficient femoral or sciatic block, thereby possibly influencing their results [1, 4, 7–9, 11–14].
Another advantage of our concept is the placement of catheters allowing repeated injections instead of a single-shot sciatic block. By this approach, we were able to modify the treatment according to the patients’ individual needs and could simultaneously evaluate the intensity of pain in the time course by comparing the number of necessary injections into the catheters. Thus, we could demonstrate an increased demand of additional injections in both groups from the morning of the first until the morning of the second post-operative day. Additionally, the total number of supplemental injections was significantly higher in the INT group.
Probably, the increasing demand in both groups as well as the higher rate of injections in the INT group were caused by the fading effect of the initial nerve block. Therefore, a continuous concept seems to be of advantage, since the number of additional injections increased in the post-operative course in spite of the fact that a long-acting local anaesthetic was used in both groups. A reduction was observed not before 48 hours post-operatively. Both findings suggest a benefit of a catheter based analgesic regimen.
A weakness of the investigation is that we did not include a placebo group with femoral block but without sciatic block. Therefore, we are not able to prove a superior analgesic effect of a combined approach compared with a continuous femoral block alone based on our data. We decided not to include a placebo group because we did not want to expose our patients to the risk of a puncture- or catheter-related complication without the possible benefit of the nerve block. Other possibilities would have been a group with single-shot sciatic block or without sciatic block at all. One might pose the question if a sciatic block is necessary at all. The literature assessing this topic is equivocal: some authors could not observe an advantage of a single-shot sciatic block or continuous block in combination with a femoral nerve block [1, 3, 7]. Others found a clear benefit of a single-shot sciatic block [12, 13] or continuous sciatic block [9, 11, 14]. In contrast to our results, Sato et al. [9] were able to demonstrate a clear benefit of a continuous sciatic block with regard to pain scores and morphine consumption in a randomised double-blind clinical trial. Two differences between their design and the approach of our investigation might be responsible for the different results: (1) the comparison with a single shot sciatic block and (2) the injection of a considerably lower dose of ropivacaine (20 ml of a 0.2 % solution) into the SNB.
Ilfeld et al. [15] investigated the effect of a popliteal sciatic block with three different regimens: a high-dose continuous ropivacaine infusion with bolus administration on demand, a low-dose continuous infusion with bolus on demand and a bolus on demand group without continuous infusion. They reported higher pain scores in the latter group, concluding that a continuous regimen might be advantageous compared with a bolus concept.
We observed a relatively high number of catheter failures in our investigation consecutively leading to dropouts. Of note, patients were excluded from further analysis not only if a problem with the sciatic catheter occurred but also if the same situation appeared with the femoral catheter. Thus, the risk of a dropout was doubled by this approach. Nevertheless, an exact assessment of pain in the posterior part of the knee would not have been feasible after oral or intravenous administration of analgesics in order to relieve the pain in the anterior part. Therefore, patients without femoral catheter had to be regarded as dropouts in this setting in spite of a sufficient sciatic catheter.
Other reasons might also have contributed to the reported failure rate: the nerve blocks were performed by all members of our staff, in many cases by residents (under supervision). Additionally, performing the nerve blocks with use of ultrasound might have resulted in a higher initial success rate. However, at the time the study design was developed, only a small proportion of the staff was experienced with ultrasound. The restriction to a small team of regional anaesthesia specialists would probably have increased the quality of the nerve blocks, but would not have reflected a clinical routine situation in a teaching hospital.
Nerve injuries caused by nerve blocks were not observed in our investigation and are a rare event. Additionally, general anaesthesia without performing regional anaesthesia techniques was identified as a risk factor for increased post-operative pain scores in a large retrospective study by Liu et al. [16]. However, nerve blocks are able to produce unwanted muscular weakness and numbness of the extremities, thereby increasing the risk of falling, impairing early mobilisation and worrying patients as well as physicians because of suspected nerve injury [17]. Therefore, many institutions are reluctant to perform these techniques. The use of an intermittent catheter-based regimen might be able to reduce these problems: the initial dose or concentration of the local anaesthetic can be reduced compared with a single-shot concept. Thus, the unwanted side effects mentioned above might occur less frequently and nerve injuries detected or ruled out earlier in the post-operative time course.
Our approach to use an intermittent regimen for the sciatic block intended to minimise effort and costs produced by a second infusion pump. The concept proved to be feasible without disadvantages for the patients; however, repeated injections were necessary over a period of several days. As a consequence of these results, we continue to use catheter-based sciatic blocks in our department. Nevertheless, we were not able to prove a superior effect of one of the two regimens tested. Additionally, the strategies and recommendations in the literature are various: local anaesthesia provided intra-operatively might contribute to improved analgesia: Song et al. [18] observed a benefit of a single-shot intra-operative peri-articular injection of local anaesthesia compared with an intravenous patient-controlled analgesia. Moreover, Broome et al. [19] demonstrated a significant long-lasting analgesic effect of a single-shot intra-articular injection with a new liposomal bupivacaine with lower pain scores than in the control group receiving a femoral block.
Therefore the generality of our results might be limited. Further studies assessing this topic should assess pain in the ventral and the dorsal part of the knee separately from each other in order to distinguish the effect of the sciatic block from the femoral block. Ideally, they should include a placebo group.
In conclusion, a sciatic block, either as a continuous infusion or as intermittent bolus injections on demand, was able to provide adequate analgesia in the dorsal part of the knee. The frequency of additional bolus injections was higher in the intermittent group.
References
Abdallah FW, Brull R (2011) Is sciatic nerve block advantageous when combined with femoral nerve block for postoperative analgesia following total knee arthroplasty? A systematic review. Reg Anesth Pain Med 36:493–498
Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d’Athis F (1999) Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 91:8–15
Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A, Murthy Y (2010) Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology 113:1144–1162
Bauer MC, Pogatzki-Zahn EM, Zahn PK (2014) Regional analgesia techniques for total knee replacement. Curr Opin Anaesthesiol 27:501–506
Chan EY, Fransen M, Parker DA, Assam PN, Chua N (2014) Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev 5:CD009941
Fischer HB, Simanski HJ, Sharp C, Bonnet F, Camu F, Neugebauer EA, Rawal N, Joshi GP, Schug SA, Kehlet H (2008) A procedure-specific systematic review and consensus recommendations for postoperative analgesia following total knee arthroplasty. Anaesthesia 63:1105–1123
Abdallah FE, Brull R (2012) Sciatic nerve block for analgesia after total knee arthroplasty: the jury is still out. Reg Anesth Pain Med 37:122–123
Al-Zahrani T, Doais KS, Aljassir F, Alshaygy I, Albishi W, Terkawi AS (2014) Randomized clinical trial of continuous femoral nerve block combined with sciatic nerve block versus epidural analgesia for unilateral total knee arthroplasty. J Arthroplasty 30(1):149–154
Sato K, Adachi T, Shirai N, Naoi N (2014) Continuous versus single-injection sciatic nerve block added to continuous femoral nerve block for analgesia after total knee arthroplasty: a prospective, randomized, double-blind study. Reg Anesth Pain Med 39:225–229
Soltesz S, Biedler A, Saxler G, Milles-Thieme S, Ziegeler S (2013) Intermittent sciatic block combined with continuous femoral block for patients undergoing knee arthroplasty: a retrospective analysis of 208 patients. Eur J Anaesthesiol 30:187–188
Ben-David B, Schmalenberger K, Chelly JE (2004) Analgesia after total knee arthroplasty: is continuous sciatic blockade needed in addition to continuous femoral blockade? Anesth Analg 98:747–749
Cook P, Stevens J, Gaudron C (2003) Comparing the effects of femoral nerve block versus femoral and sciatic nerve block on pain and opiate consumption after total knee arthroplasty. J Arthroplasty 18:583–586
Hunt KJ, Bourne MH, Mariani EM (2009) Single-injection femoral and sciatic nerve blocks for pain control after total knee arthroplasty. J Arthroplasty 24:533–538
Wegener JT, van Ooij B, van Dijk CN, Hollmann MW, Preckel B, Stevens MF (2011) Value of single-injection or continuous sciatic nerve block in addition to a continuous femoral nerve block in patients undergoing total knee arthroplasty: a prospective, randomized, controlled trial. Reg Anesth Pain Med 36:481–488
Ilfeld BM, Morey TE, Wang RD, Enneking FK (2002) Continuouspopliteal sciatic nerve block for postoperative pain control athome. Anesthesiology 97:959–965
Liu SS, Buvanendran A, Rathmell JP, Sawhney M, Bae JJ, Moric M, Perros S, Pope AJ, Poultsides L, la Valle CJ, Shin NS, McCartney CJ, Ma Y, Shah M, Wood MJ, Manion SC, Sculco TP (2012) Predictors for moderate to severe acute postoperative pain after total hip and knee replacement. Int Orthop 36:2261–2267
Memtsoudis SG, Yoo D, Stundner O, Danninger T, Ma Y, Poultsides L, Kim D, Chisholm M, Jules-Elysee K, Valle AG, Sculco TP (2015) Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop 39:673–680
Song MH, Kim BH, Ahn SJ, Yoo SH, Kang SW, Kim YJ, Kim DH (2015) Peri-articular injections of local anaesthesia can replace patient-controlled analgesia after total knee arthroplasty: a randomised controlled study. Int Orthop. doi:10.1007/s00264-015-2940-2
Broome CB, Burnikel B (2014) Novel strategies to improve early outcomes following total knee arthroplasty: a case control study of intra articular injection versus femoral nerve block. Int Orthop 38:2087–2089
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support and sponsorship
None.
Financial sources that support the work
None
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Soltesz, S., Meiger, D., Milles-Thieme, S. et al. Intermittent versus continuous sciatic block combined with femoral block for patients undergoing knee arthroplasty. A randomized controlled trial. International Orthopaedics (SICOT) 40, 1861–1867 (2016). https://doi.org/10.1007/s00264-016-3117-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3117-3