Abstract
Purpose
In order to diminish total hip arthroplasty (THA) dislocation rate, surgeons strive to achieve adequate component orientation, offset and limb length. In addition, dislocation rate can theoretically be reduced by increasing head diameter and by choosing implants with favorable head-to-neck and cup-to head ratios. We assessed nine radiographic and implant-related parameters associated with an increased risk of dislocation in patients who sustained a dislocation and in those with a stable arthroplasty.
Methods
A total of 1,487 consecutive elective primary THAs performed by a single surgeon, using a posterolateral approach were reviewed at an average follow-up of 18 months (range, 1–112). Fixation was hybrid in 85 % of hips and non-cemented in 15 %. Thirty-eight patients (38 hips, 2.5 %) sustained at least one dislocation. Thirty-seven patients with good quality, standardized anteroposterior radiographs were selected as a “study group”. The study group was matched-paired (1:3) with patients who had a stable arthroplasty based on gender, age, BMI, diagnosis and follow-up. Variables compared between the groups included: head size, cup size, head-to-neck ratio, cup-to-head ratio, leg-length discrepancy, offset, cup inclination, cup version and cup orientation based on the safe zone defined by Lewinnek et al.
Results
None of the nine parameters showed a statistically significant difference between the groups.
Discussion
In this study, 90 % of patients who developed a dislocation had properly positioned acetabular components. In addition, the vast majority of patients in the study group had adequate restoration of limb length and offset. The results of our study may be useful for the orthopedic surgeons who discuss instability following THA surgery, particularly in patients with radiographically sound reconstructions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dislocation is one of the most frequent early complications of total hip arthroplasty (THA) [1, 2]. It is the second leading cause for revision after aseptic loosening [3]. Malkani et al. [4] in an analysis of Medicare claims from 1998 to 2007 determined that dislocation is the most frequent cause of early revision (36 %) within the first two years following surgery.
The rate of dislocation varies widely between 0.5 and 10 % [5–9]. The dislocation rate during the first post-operative year in 14,314 THAs performed between 1996 and 2004 and included in the Scottish National Arthroplasty Project was 1.9 % [10]. These rates should be interpreted with caution as the risk of dislocation increases with follow-up [11].
The risks of dislocation and dislocation-related re-operation are often discussed before surgery based on the patient’s pre-operative risk factors. Patient-related factors include but are not limited to: age greater than 70 years, female gender, diagnosis of hip fracture or avascular necrosis, medical comorbidities, alcoholism, soft tissue laxity, and patient’s non-compliance with post-operative dislocation precautions [12]. A high body mass index (BMI) has also been linked to dislocation after THA revision surgery [13].
Other factors unrelated to the patient have been linked to a high dislocation rate: a low surgical volume [14, 15] and the use of a posterior approach [16, 17], particularly when a soft tissue repair is not performed [16].
During the planning and execution of surgery, a number of mathematic and mechanical “intra-operative” factors are carefully considered by surgeons including the reconstitution of normal hip biomechanics (offset and leg length), adequate positioning and orientation of the components, and a number of implant related factors including head and cup diameter, head-to-neck ratio, cup-to-head ratio and offset. Lewinnek et al. [18] described in 1978 a so-called “safe-zone” of 5–25° of anteversion and 30–50° of inclination, which has become a recognized standard of adequate cup position. These “intra-operative” factors are also scrutinized by physicians while assessing patients who developed post-operative instability.
Surgeons specializing in THA surgery strive to control the majority of previously mentioned factors in order to achieve low dislocation rates. It has been the impression of the senior author, as well as others [19], that even when taking all previously mentioned factors into account, dislocations can still occur in seemingly compliant patients with no major radiographic abnormalities.
In order to assess the role of the previously mentioned variables, we compared head diameter, cup diameter, head-to-neck ratio, cup-to-head ratio, leg-length discrepancy, offset, cup inclination, cup anteversion, and “safe” cup positioning [18] in patients who developed a dislocation following THA and in those of patients with stable THAs. The comparison was made while trying to control for the majority of additional predisposing factors.
Material and methods
In this retrospective, single-centre, single-surgeon study, we included 1,334 consecutive patients who underwent 1,474 elective, primary THAs (140 bilateral). Patients undergoing THA for a hip fracture were excluded. All patients were operated on by a specialized hip surgeon (A.G.D.V.) between 2005 and 2014.
We reviewed all patient charts, operative records and radiographs obtained using a standardized technique [20]. As this investigation focused on THA dislocation, the hip and not the patient was considered the unit of the study.
Surgeries were performed utilizing a standardized protocol that included intention to use regional, hypotensive anesthesia, lateral decubitus, and posterolateral approach. Enhanced posterior soft tissue repair was routinely used [21, 22]. Cementless acetabular fixation was used in all 1,474 THAs. Cemented femoral fixation was used in 1,257 THAs and cementless fixation with a proximally coated stem in the remaining 217. Metal on polyethylene articulation was used in 1,459 of 1,474 hips (98.9 %). Before surgery, a validated pre-operative planning was performed [20] aiming at restoring hip biomechanics. Patients were mobilized the day after surgery and observed posterior dislocation precautions for six weeks. They were encouraged to bear weight as tolerated. They were mobilized with a walker and progressed to a cane. They followed posterior dislocation precautions for the first six weeks including the use of a cane, high chair and high toilet seat. They were instructed to sleep with a pillow between the legs for six weeks. After that, they were instructed to avoid high hip flexion, adduction and internal rotation for life by means of post-operative patient verbal and written education.
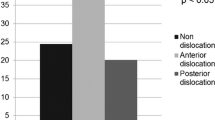
There were 38 patients with 38 hips (2.6 %) who presented with one or more dislocations occurring at an average follow-up of 18 months (range, 0–80 months). The direction of dislocation was posterior in 36 hips and anterior in two. One patient with an anterior dislocation had poor quality radiographs for evaluation and was excluded from the analysis, leaving 37 patients (37 hips) in the study group.
The mechanism of dislocation was hyperflexion and internal rotation in 18, hyperflexion in ten, trauma in three, and unknown in three. The three remaining patients dislocated while performing regular daily activities and observing posterior dislocation precautions.
The 37 patients (37 hips) in the study group were matched 1:3 with 111 patients (111 hips) with a stable THA (control group). Matching was performed based on age (±7 years), gender, BMI (±6), follow-up (±6 months) and diagnosis (Table 1). All study and control patients had a metal-on-polyethylene articulation. All patients in the control group were personally interviewed by the senior author at last follow-up to confirm that they had a stable arthroplasty with no dislocations.
For all study and control patients, we recorded implant characteristics (cup diameter, head diameter and neck length). We used manufacturer’s data to calculate head-to-neck ratio and cup-to-head ratio. Standardized radiographs taken by a single group of radiology technicians were blindly measured by a single observer who was not involved in patient care (A.G.D.V.) to calculate the following additional outcome variables: leg length discrepancy, offset difference with the contralateral hip, cup inclination, cup anteversion and cup position based on Lewinnek’s safe zone [18].
Measurements were done in Sectra IDS7 PACS station (Sectra, Linkoeping, Sweden) and calibrated for magnification. Leg length discrepancy was determined as the perpendicular distance between the proximal corner of the lesser trochanter and a horizontal reference line drawn through the base of the teardrops (Fig. 1). Offset was calculated as the percentage difference between the offset of the THA and that of the opposite hip (Fig. 1). Cup inclination was measured as the angle between the cup’s superior and inferior edges and the previously mentioned reference line (Fig. 1). Cup anteversion was calculated based on the algorithm proposed by Lewinnek et al. in the anteroposterior radiographs. Cup inclination and anteversion was used to determine adequacy of cup orientation within Lewinnek et al.’s safe zone [18].
An anteroposterior view of the pelvis demonstrates a horizontal reference line through the base of the teardrops (a-a’). The limb-length discrepancy was determined by measuring the perpendicular distance from the reference line to the proximal corner of the lesser trochanters (b and b’). The femoral offset of both hips (c and c’) was used to calculate the offset differential. Cup inclination (α) was measured as the angle between the cup’s superior and inferior edges and the reference line (a-a’)
Statistical analysis
For the a priori power analysis, we used the estimates of the effect of head diameter on the dislocation rate reported by Amlie et al. [23] and assumed a correlation coefficient between matched case and control patients to be 0.25 in a matched case–control study. A sample size of 30 cases and a matched sample of 90 control patients achieved 90 % power to detect an odds ratio of 6.06 versus the alternative of equal odds using a chi-square test with a 0.05 significance level.
Descriptive statistics were presented for matching variables and other prognostic factors of interests. Continuous variables were summarized using means and standard deviations; a paired t-test was used for comparisons between matched study and control cases. Categorical variables were reported using frequencies and proportions, and were compared using chi-square or Fisher exact tests. Conditional logistic regression was applied to examine the relationship between dislocation and a set of prognostic factors that were found to be significant or borderline significant in the univariate analysis. SAS Proc PHREG was used and adjusted for the matched pair nature of the data. Adjusted odds ratios and 95 % confidence limits were calculated and presented.
Results
The direct comparison of outcome variables between cases and controls revealed that study patients (dislocators) and controls (non-dislocators) had no significant differences in any of the outcome variables studied. The following variables were found to be marginally significant: head-to-neck ratio (p = 0.09), leg length discrepancy (p = 0.07), cup diameter (p = 0.07), and cup anteversion (p = 0.06) (Table 2).
After including all variables with a marginally significant difference in a regression analysis, none was found to be significantly different between cases and controls (Table 3).
Discussion
Dislocation after THA affects patients and physicians, and increases the cost of care. When assessing a patient with a dislocated THA, the surgeons utilize plain radiographs and other studies to assess the factors analyzed in our study, and determine the cause of instability. This assessment has substantial treatment implications, as surgery for recurrent hip instability often focuses on revising malpositioned components, correcting offset and, when possible increase the diameter of the femoral head. In addition, the detection of suboptimal biomechanical conditions in a patient with THA instability has legal implications.
However, it has been the impression of the senior author (A.G.D.V.) that dislocations frequently occurred in patients with biomechanically sound reconstructions. This “counterintuitive” observation prompted us to perform the current study. In order to focus on intraoperative variables that may be associated with a higher risk of dislocation, we controlled for a number of well-recognized pre-operative factors predisposing to post-operative instability using a strict matched-pair methodology.
We were unable to find any intra-operative factor related to the implant choice, technique of implantation, and positioning that could explain the occurrence of a dislocation. Our analysis shows that despite achieving radiographically sound reconstructions and paying careful attention to choosing implants with desirable characteristics, dislocations still occur.
There are limitations to our analysis. The first is the retrospective nature of the study and selection bias: the senior author has always strived to use implants with favorable head-to-neck and cup-to-head ratios. He used a validated pre-operative planning protocol aimed at minimizing error in implant positioning and in restoring hip biomechanics [20], and, when possible, avoided the use of femoral heads with a skirt. He has routinely used enhanced posterior soft tissue repair [21]. As the intra-operative variables controlled by the senior author are routinely considered by the majority of surgeons, an analysis of cases in which these details are not controlled is unfeasible. The second limitation is the lack of a complete range of femoral head diameters. The senior author has used 28 and 32 mm diameter heads. The effect of smaller and larger diameter heads on the results of this study cannot be assessed. A third limitation is the sample size. It can be argued that the lack of statistical significance observed in the variables analyzed in our study can be the result of a beta-type error (underpowered study). In order to overcome this limitation, a pre-study power analysis was performed. For power analysis, we selected the diameter of the femoral head, which has been widely recognized as being associated with dislocation. Our power analysis demonstrated that our sample size may be sufficient to detect an effect of femoral head on dislocation rates. The fourth limitation is the lack of control over post-operative variables. It can be speculated that those patients who dislocate are less likely to have followed dislocation precautions than those who did not dislocate. On the other hand, it is well recognized that a substantial proportion of patients with stable THAs do not follow dislocation precautions. In the present study, all patients were educated after surgery with a standardized protocol and education material and asked to follow posterior dislocation precautions for life. The last limitation is the lack of generalisation. It is likely that devoted arthroplasty surgeons are able to execute a more precise surgery than low volume ones, thus, the results of our study cannot be extrapolated to surgeons with different level of training and utilizing different surgical approaches. Based on the previously discussed limitations, we believe that we can safely answer our research questions.
Femoral offset contributes to hip stability [22, 24, 25]. Fackler and Poss [1] studied 1443 THA patients. Those who dislocated (2.4 %) had a mean loss of offset of 5.2 mm compared to patients with a stable THAs. In our series, attention was paid to restoring offset by means of pre-operative planning. The THAs in the study group and in the control group had similar offset compared to the contralateral hip (p = 0.94).
Equalization of leg length allows a natural gait, improves stability by maintaining muscle tension and increases patient’s satisfaction [25]. In our analysis, the average leg length discrepancy was only 0.9 mm (study group, 0.62 mm; control group, 0.27 mm [p = 0.22]).
We observed that the use of a 28-mm head was not associated with a significantly higher risk of dislocation compared to 32-mm ones (p = 1). However, other investigators reported a reduction in dislocation rates with larger diameter heads [23, 26]. It is possible that the effect of femoral head size in the dislocation rate cannot be fully appreciated when 28- and 32-mm heads are compared, and that a reduction be seen with larger diameter heads. However, large-diameter heads cannot always be used, particularly in patients with small diameter sockets, as the consequently thin polyethylene liners can suffer from runaway wear or fracture [27].
Likewise, we were unable to demonstrate a relationship between the dislocation rate and cup diameter, as suggested by other investigators [28, 29]; head-to-neck ratio (p = 0.22); or cup-to-head ratio (p = 0.71).
The role of cup inclination and anteversion on the dislocation rate has been extensively studied, both independently [30–32] and combined [18]. Acceptable ranges for inclination and anteversion range from 30 to 50° [18, 33] and from 0 to 30° [34] respectively. When cups are positioned within an adequate range, it is believed that a number of unwanted complications are minimized, including increased wear [27], polyethylene fracture, impingement and instability. In our study, we observed that an inclination difference of only 2° (dislocation group more vertical than non-dislocation group) was statistically significant between cases and controls in the univariate analysis. Paradoxically, a difference of 2° in anteversion was also significantly different between cases and controls, with cases having more anteversion than controls. There was no difference in the number of patients with cups falling within the accepted ranges proposed by Lewinnek et al. [18]. Other authors have observed similar findings [19] and have questioned the validity of Lewinnek et al.’s safe zones in modern THA.
In summary, in our study, which spans for a decade of a single specialized orthopedic surgeon, we were unable to find a relationship between ten intra-operative and implant related variables, and the dislocation rate. In the surgeon’s experience, dislocation in patients who undergo elective surgery through a posterolateral approach is 2.6 % at 18 months of average follow-up. It is likely that the experience of the senior author is similar to other specialized surgeons: most THA dislocations will occur in patients with no major radiographic abnormalities. Our findings may aid clinicians while discussing post-operative instability in patients who have radiographically sound reconstructions. In addition, our findings have legal implications indicating that a large number of THA dislocations occur in biomechanically sound reconstructions with no implant malpositioning.
References
Fackler CD, Poss R (1980) Dislocation in total hip arthroplasties. Clin Orthop Relat Res 151:169–178
Macaulay W, Saleh K, Parvizi J (2006) Total hip arthroplasty dislocation: prevention and management: editorial comment. Clin Orthop Relat Res 447:2–3. doi:10.1097/01.blo.0000218741.54000.68
Puolakka TJ, Pajamäki KJ, Halonen PJ, Pulkkinen PO, Paavolainen P, Nevalainen JK (2001) The finnish arthroplasty register: report of the hip register. Acta Orthop Scand 72:433–441. doi:10.1080/000164701753532745
Malkani AL, Ong KL, Lau E, Kurtz SM, Justice BJ, Manley MT (2010) Early- and late-term dislocation risk after primary hip arthroplasty in the medicare population. J Arthroplasty 25:21–25. doi:10.1016/j.arth.2010.04.014
Woo RY, Morrey BF (1982) Dislocations after total hip arthroplasty. J Bone Joint Surg Am 164:1295–1306
Van Sikes C, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM (2008) Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty 23:59–63. doi:10.1016/j.arth.2008.06.032
Mahoney CR, Pellicci PM (2003) Complications in primary total hip arthroplasty: avoidance and management of dislocations. Instr Course Lect 52:247–255
Fricka KB, Marshall A, Paprosky WG (2006) Constrained liners in revision total hip arthroplasty: an overuse syndrome. In the affirmative. J Arthroplasty 21:121–125. doi:10.1016/j.arth.2006.02.100
Allami MK, Fender D, Khaw FM, Sandher DR, Esler C, Harper WM et al (2006) Outcome of Charnley total hip replacement across a single health region in England. The results at ten years from a regional arthroplasty register. J Bone Joint Surg (Br) 88:1293–1298. doi:10.1302/0301-620X.88B10.17933
Meek RMD, Allan DB, McPhillips G, Kerr L, Howie CR (2006) Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res 447:9–18. doi:10.1097/01.blo.0000218754.12311.4a
Padgett DE, Warashina H (2004) The unstable total hip replacement. Clin Orthop Relat Res 420:72–79. doi:10.1097/01.blo.0000122694.84774.b5
Brooks PJ (2013) Dislocation following total hip replacement: causes and cures. Bone Joint J 95:67–69. doi:10.1302/0301-620X.95B11.32645
Kim Y, Morshed S, Joseph T, Bozic K, Ries MD (2006) Clinical impact of obesity on stability following revision total hip arthroplasty. Clin Orthop Relat Res 453:142–146. doi:10.1097/01.blo.0000238874.09390.a1
Hedlundh U, Ahnfelt L, Hybbinette CH, Wallinder L, Weckström J, Fredin H (1996) Dislocations and the femoral head size in primary total hip arthroplasty. Clin Orthop Relat Res 333:226–233
Manley M, Ong K, Lau E, Kurtz SM (2008) Effect of volume on total hip arthroplasty revision rates in the United States Medicare population. J Bone Joint Surg Am 90:2446–2451. doi:10.2106/JBJS.G.01300
Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ (2006) Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res 447:34–38. doi:10.1097/01.blo.0000218746.84494.df
Byström S, Espehaug B, Furnes O, Havelin LI (2003) Femoral head size is a risk factor for total hip luxation. Acte Orthop Scand 74:514–524
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60:217–220
Esposito CI, Gladnick BP, Lee Y, Lyman S, Wright TM, Mayman DJ, Padgett DE (2015) Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty 30:109–113. doi:10.1016/j.arth.2014.07.009
Gonzalez Della Valle A, Padgett DE, Salvati EA (2005) Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg 13:455–462. doi:10.1007/s00264-011-1289-4
Pellicci PM, Bostrom M, Poss R (1998) Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res 355:224–228
Weeden SH, Paprosky WG, Bowling JW (2003) The early dislocation rate in primary total hip arthroplasty following the posterior approach with posterior soft-tissue repair. J Arthroplasty 18:709–713. doi:10.1054/S0883-5403(03)00254-7
Amlie E, Høvik Ø, Reikerås O (2010) Dislocation after total hip arthroplasty with 28 and 32-mm femoral head. J Orthop Traumatol 11:111–115. doi:10.1007/s10195-010-0097-8
Wera GD, Ting NT, Moric M, Paprosky WG, Sporer SM, Della Valle CJ (2012) Classification and management of the unstable total hip arthroplasty. J Arthroplasty 27:710–715. doi:10.1016/j.arth.2011.09.010
Wallner O, Stark A, Muren O, Eisler T, Sköldenberg O (2015) Unstable hip arthroplasties. A prospective cohort study on seventy dislocating hips followed up for four years. Int Orthop 39:1037–1044. doi:10.1007/s00264-014-2583-8
Berry DJ, von Knoch M, Schleck CD, Harmsen WS (2005) Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am 87:2456–2463. doi:10.2106/JBJS.D.02860
González Della Valle A, Su E, Zoppi A, Sculco TP, Salvati EA (2004) Wear and periprosthetic osteolysis in a match-paired study of modular and nonmodular uncemented acetabular cups. J Arthroplasty 19:972–977. doi:10.1016/j.arth.2004.06.001
Peter R, Lübbeke A, Stern R, Hoffmeyer P (2011) Cup size and risk of dislocation after primary total hip arthroplasty. J Arthroplasty 26:1305–1309. doi:10.1016/j.arth.2010.11.015
Kelley SS, Lachiewicz PF, Hickman JM, Paterno SM (1998) Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop 355:163–170
Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA et al (2011) The John Charnley Award: risk factors for cup malpositioning: Quality improvement through a joint registry at a tertiary hospital. Clin Orthop Rel Res 469:319–329. doi:10.1007/s11999-010-1487-1
Ackland MK, Bourne WB, Uhthoff HK (1986) Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J Bone Joint Surg (Br) 68:409–413
Craiovan B, Renkawitz T, Weber M, Grifka J, Nolte L, Zheng G (2014) Is the acetabular cup orientation after total hip arthroplasty on a two dimension or three dimension model accurate? Int Orthop 38:2009–2015. doi:10.1007/s00264-014-2336-8
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815–821. doi:10.1016/j.orthres.2003.11.001
Kummer FJ, Shah S, Iyer S, DiCesare PE (1999) The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty 14:509–513. doi:10.1016/S0883-5403(99)90110-9
Acknowledgements
This study was funded by the generous donation of Mr. GlennBergenfield and the Sidney Milton and Leoma Simon Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Opperer, M., Lee, Yy., Nally, F. et al. A critical analysis of radiographic factors in patients who develop dislocation after elective primary total hip arthroplasty. International Orthopaedics (SICOT) 40, 703–708 (2016). https://doi.org/10.1007/s00264-015-3022-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3022-1