Abstract
Purpose
In Norway, 19 % of revisions of non-resurfaced total knee arthroplasties done for knee pain between 1994 and 2011 were Secondary Patella Resurfacing (SPR). It is, however, unclear whether SPR actually resolves the pain. The aim was to investigate prostheses survival and clinical outcomes following SPR.
Method
A total of 308 knees (301 patients) with SPR were used to assess implant survival, and a sub-cohort (n = 114 out of 301 patients) with Patient Reported Outcome Measures (PROMs) data were used to assess the clinical outcomes. The EuroQol (EQ-5D), the Knee Injury and Osteoarthritis Outcome Score, and Visual Analogue Scales on satisfaction and pain were used to collect PROM data. Outcomes were analysed by Kaplan-Meier, Cox regression, and multiple linear regression.
Results
The five- and ten-year Kaplan-Meier survival percentages were 91 % and 87 %, respectively. Overall, 35 knees were re-revised at a median follow-up of eight years and pain alone (10 knees) was the main cause of re-revision. Younger patients (<60 years) had nearly nine times higher risk of re-revision compared to older patients (>70 years) (RR = 8.6; p < 0.001). Mean EQ-5D index score had improved from 0.41 (SD 0.21) preoperative to 0.56 (SD 0.25) postoperative following SPR. A total of 63 % of patients with PROM data were satisfied with the outcomes of SPR.
Conclusion
The long-term prostheses survival following SPR was satisfactory, although not as good as for primary knee replacement. Patients’ health related quality of life improved significantly following SPR. Still, more than a third of patients with PROMs data were dissatisfied with the outcomes of the SPR procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to some authors the risk of anterior knee pain and the need for secondary patella resurfacing (SPR) after primary total knee arthroplasties (TKAs) is higher after patella non-resurfaced primary prostheses than after a patella-resurfaced primary TKAs [1–3]. In Norway, between 1994 and 2011, 19 % of revisions of patella non-resurfaced primary TKAs were SPR due to pain [4]. However, it is not clear whether the pain is resolved with SPR.
Several clinical studies have been published addressing the results of SPR, but the reported series are small and none of these studies have reported implant survival and clinical outcomes as a combined outcome measure [5–10]. Moreover, as far as we know, only two register studies have reported the survival rate [1] and patient’s satisfaction [11] following SPR, but they did not assess other clinical outcomes, namely, the functional outcome, level of pain relief, and/or changes in health-related quality of life (HRQoL) following SPR.
The aim of our study was to assess prostheses survival and clinical outcomes as well as to assess factors that predict outcomes of the SPR procedure done to painful non-resurfaced TKAs.
Materials and methods
Study population and source of data
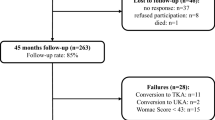
This study was based on surgical procedure data from the Norwegian Arthroplasty Register (NAR) and additional information on Patients Reported Outcome Measures (PROMs). Only patients who underwent SPR after non-resurfaced primary TKAs due to pain alone (i.e. anterior knee pain and/ or global knee pain) and reported to the NAR between 1994 and 2011 were eligible for this study. In this study, pain was considered as a primary reason for failure of TKA if not combined with other causes of failure. Overall, 308 knees (301 patients) were included in this study, and a sub-cohort of 114 of these patients had PROM data based on which the clinical outcomes of SPR were assessed (Fig. 1).
The NAR is a nationwide register initiated as a hip arthroplasty register in 1987 and later extended to also include arthroplasties of all other joints from January 1994. The NAR does not record any prospective PROMs related to any knee arthroplasty operations to date. Thus, we used unpublished PROMs data collected in 2006 as a part of an earlier PhD study project from the NAR [12]. The PROM data was collected using a self-administered postal-questionnaire sent to all patients with revision knee arthroplasties reported to the NAR between 1st January 1994 and 5th September 2005. Only patients who had a minimum of one-year follow-up after SPR were included in the postal-questionnaire survey.
The PROMs data used in the study were quality of life according to the EQ-5D [13, 14], functional outcome using Knee Injury and Osteoarthritis Outcomes Score (KOOS) [15], Visual Analogue Scale (VAS) for satisfaction and pain [16, 17], and questions related to musculoskeletal comorbidity (Charnley category) [18]. The EQ-5D index scores range from 0 (indicating a health status close to death) to 1 (indicating best possible health status). The KOOS subscale scores and the VAS scores range from 0 to 100 with “0” indicating worst possible state and “100” indicating the best possible state. Calculation of the KOOS subscale scores and missing items was done in accordance with the KOOS scoring 2012 guidelines (http://www.koos.nu/index.html). A validated Norwegian version of KOOS (http://koos.nu) and EQ-5D (http://www.euroqol.org) were used.
Statistics
The Kaplan-Meier and Cox regression analyses with any causes for re-revision as the end point were used to calculate implant survival probabilities and risk of re-revision, respectively. In the present study, the survival times of implants were censored at the date of emigration or death or at the end of the study on December 31, 2011. The graphical examination (log minus log plot) was used to assess the proportional hazard assumption of the Cox-regression model and the assumption was fulfilled.
A paired-samples t-test was conducted to evaluate the impact of the revision operation on patients’ HRQoL. Multiple linear regression was used to assess differences in mean scores in the PROMs. In all analyses, p-values ≤ 0.05 were considered statistically significant and the statistical analyses were performed using the statistical software IBM-SPSS version 22.
Ethical clearance
The NAR has a license from the Norwegian Data Inspectorate (reference number: 03/00058-15/JTA and last issued 19th April 2012), and The Regional Committee for Research Ethics in Western Norway approved the survey (date of issue: 02/23/2006, registration number: 046:06), with extended permission (latest date of issue 07/11/2012, registration number: 2012/1692/REK Vest).
Results
Demographic characteristics
The demographic characteristics for the included cases are summarized in Table 1. Of them, 73 % were women, 76 % were 60 years or older at revision, 80 % had osteoarthritis as primary diagnosis and 66 % were Charnley category ‘C’ patients. For the PROM data, 114 out of the 121 patients to whom the postal-questionnaire were sent had responded to the questionnaire yielding a response rate of 94.2 % (Fig. 1).
Survival of implants
The crude re-revision percentage was 11 % (35 of 308 knees) at a median follow-up of eight years (range 0–17 years). Pain alone (ten knees), loose femoral component (five knees), deep infection (four knees), loose tibia component (four knees), and instability (four knees) were the main causes of re-revision following SPR. The Kaplan-Meier survival percentage was 91 % (95 %CI 87–94 %) at five years and 87 % (95 %CI 82–91 %) at ten years (Fig. 2a). The relative risk (RR) of re-revisions was higher in patients aged < 60 years (RR = 8.6; 95%CI 3.2–23.1; p < 0.001) compared to patients aged >70 years (Table 2). We observed no statistically significant differences in risk of re-revision following SPR between patients with and without PROM data (Fig. 2b).
EQ-5D index score and change in pain severity level
The mean EQ-5D index score significantly increased from 0.41 (SD 0.21) to 0.56 (SD 0.25) after SPR (Table 1). The paired–samples t-test showed that each of the five EQ-5D domains improved in mean scores after SPR but were statistically significant only for mobility (Δ mean =0.16 (SD 0.46), p < 0.001), usual activities (Δ mean =0.16 (SD 0.57), p = 0.003), and pain/discomfort (Δ mean =0.51 (SD 0.73), p < 0.001). Overall, patients with the most severe pre-operative pain/discomfort in the EQ-5D domain gained most (69 % of 71 patients) from the SPR procedure (Fig. 3). Female sex was a risk factor for poorer outcome in the mean ΔEQ-5D index score (p < 0.05) (Table 3).
KOOS subscales
The mean scores in KOOS subscales were KOOS-pain, 55 (SD 25); KOOS-symptoms, 64 (SD 20); KOOS-ADL, 52 (SD 24); KOOS-sport/rec., 17 (SD 22); and KOOS-QoL, 38 (SD 26). Older age (>70 years) had a positive effect on all the KOOS subscales compared to younger age (<60 years), but the observed difference was statistically significant only for the subscale KOOS-symptoms (p < 0.05). Patients in the Charnley category ‘A’ had better outcome in the KOOS subscales scores compared to Charnley categories ‘B’ and ‘C’ (Table 3).
Pain-VAS and satisfaction-VAS
The mean pain-VAS and satisfaction-VAS scores were 55 (SD 25) and 51 (SD 27), respectively. Of the 114 patients with PROM, 63 % reported medium to complete satisfaction (satisfaction-VAS ≥40 points) with the results of the SPR procedure, but 26 % reported severe to extreme/intolerable pain (pain-VAS <40 points) after SPR.
Discussion
We assessed prostheses survival rate and clinical outcomes after SPR of painful non-resurfaced TKAs. The survival rate was 87 % at ten years and 35 knees were re-revised at a median follow-up of eight years. Pain alone was the main cause of re-revision and younger age (<60 years) was a risk factor for re-revision. For the clinical outcomes, the mean EQ-5D index score improved by 0.15 points and 63 % of the patients with PROM were satisfied with the results of SPR. Male patients had a better post-revision improvement in mean EQ-5D index score, and patients in Charnley category ‘A’ had significantly better mean score in KOOS subscales than the other categories.
The incidences of anterior knee pain following patella non-resurfaced TKA vary between 4 % and 21.4 %; and up to 30 % of these knees were revised with SPR in some studies [1, 7, 8]. Existing studies on revision TKA with SPR, except two register studies [1, 11], are based on a relatively small number of cases (7 to 58 cases) and mainly reflect rather poor outcomes of the SPR procedure in resolving anterior knee pain [5–9, 19]. Some of these studies reported that 45–66 % of patients improved following SPR and 14–30 % deteriorated or experienced some complications from the revision [5, 7, 8].
In the present study, 11 % of patients were re-revised at a median follow-up of eight years. Most re-revisions were done for pain alone or for loosening. The high number of pain alone, reported as a reason for re-revision, indicates that the procedure does not resolve the pain in a large proportion of patients. Possible explanations might be the presence of occult low grade infection and unrecognised aseptic loosening that were not detected pre-operatively by the available detection modalities. Other authors found worse results, namely, 11–18 % of re-revisions at an average follow-up of three to five years after SPR [1, 8, 10, 19]. The present study was based on a large number of cases from a national register involving a large number of surgeons and hospitals with different case volumes as well as several prostheses, which could explain this difference in re-revision rate.
The significant improvements in mean EQ-5D index score in the present study showed that SPR can be effective for relieving persisting severe anterior knee pain following primary TKAs. Such improvement in the mean EQ-5D index score following patella resurfacing was also reported by earlier studies on primary TKAs [20]. We found that only a few patients (5 %) had worse pain after the SPR procedure and this finding is in accordance with the worse pain symptoms (2.2–7 %) reported by some earlier studies [19, 21]. However, 22 of the 71 patients with severe pain problems pre-operatively had not improved in their pain post-operatively (Fig. 3). The possible explanation for this could be that knee pain following TKA is not entirely related to the patellofemoral joint; rather it is multifactorially related either to the implants design, the surgical technique, malpositioning of implants and flexion/ extension gap imbalance that the surgeon did not detect, pain from hip and spine and central pain. Compared to our findings, a recent clinical study by Scheurer et al. reported a relatively higher mean score in KOOS-pain (66), KOOS-symptoms (68), KOOS-ADL (62), and KOOS-QoL (42) [9]. Possible explanations for this difference could be that the Scheurer et al. study findings were based on relatively few cases (58 knees), used one single prosthetic design and it was a single-centre clinical study [9].
Overall, 63 % of our patients with PROM were satisfied with the results of SPR, which is exactly the same as reported by Munoz-Mahamud et al. [6]. However, this percentage was somewhat higher than that reported by some earlier studies (50–53.3 %) [11, 19] but lower than what was reported by Scheurer et al. (75 %) [9] and Parvizi et al. (80 %) [8]. The most probable cause for these differences is the fact that most earlier studies are based on relatively small sample size and are single-centre series. Other possible explanations could be the differences in patients’ profile, length of follow-up, instrument and methods used to assess patients’ satisfaction, and implants used.
We observed that male patients had significantly higher mean ΔEQ-5D index score compared to female patients. The variation seen with sex may be due to the fact that musculoskeletal pain in the general population is less common in men than women [22] and that perception of pain is higher in women than men [23]. Patients with Charnley category ‘A’ had better scores on KOOS subscales, as did older-aged patients. Such effect of age and Charnley category on KOOS subscale outcomes were also reported by earlier studies on primary TKAs [20]. The possible explanation could be greater expectations in younger patients [20].
Our study has strengths and limitations. The strength of this study is that we included a relatively large sample size and used data from a national register with high registration completeness [24]. This gave us the opportunity to include several prostheses designs (n = 13) and to involve large numbers of surgeons and hospitals (n = 51) with differing case volumes. Thus, the results may have a better external validity than results from randomized controlled trials or single-surgeon series. However, our study also has some limitations. First, the pre-operative EQ-5D was assessed retrospectively at a minimum of one-year post-operatively. The patients may have had difficulty in recalling the exact level of pre-operative symptoms. Thus, the answer of EQ-5D may be biased. Howell et al., however, found moderate to good correlation between prospective data and recall data concerning pre-operative status [25]. Second, we had no information on pre-operative KOOS and VAS scores meaning that we could not evaluate the effect of the SPR procedure using these instruments. Finally, we did not have access to X-rays or CT-scans before and after the revision procedure and could thus not evaluate the degree of osteoarthritis or malposition of the patella or the component.
The present study was based on retrospectively collected PROM data. Further clinical outcome studies with prospective pre-operative and post-operative PROM data are warranted. In the present study, over one-third of patients with PROMs were dissatisfied and the outcomes of SPR were inferior compared to that of primary patellar resurfacing. It seems that the problem of knee pain following non-resurfaced TKAs can be due to multifactorial aetiology. Studies on the clinical outcomes of SPR in relation to surgical technique and implants component designs are also needed.
In conclusion, the long-term survival percentage of non-resurfaced TKAs revised with SPR due to pain alone was satisfactory. Revision of painful non-resurfaced TKAs with isolated SPR can provide a solution to patients with severe pre-operative pain. Still, more than one-third of all patients with PROM were dissatisfied with the outcomes of the SPR procedure.
References
Clements WJ, Miller L, Whitehouse SL, Graves SE, Ryan P, Crawford RW (2010) Early outcomes of patella resurfacing in total knee arthroplasty. Acta Orthop 81:108–13. doi:10.3109/17453670903413145
Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA (2005) Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res 438:191–6
Waters TS, Bentley G (2003) Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am 85-A:212–7
NAR (2013) The Norwegian arthroplasty register (annual report). http://nrlweb.ihelse.net/Rapporter/Rapport2013.pdf. Accessed 20 Sept 2013
Karnezis IA, Vossinakis IC, Rex C, Fragkiadakis EG, Newman JH (2003) Secondary patellar resurfacing in total knee arthroplasty: results of multivariate analysis in two case-matched groups. J Arthroplasty 18:993–8
Munoz-Mahamud E, Popescu D, Nunez E, Lozano LM, Nunez M, Sastre S, Torner P, Segur JM, Macule F (2011) Secondary patellar resurfacing in the treatment of patellofemoral pain after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1467–72. doi:10.1007/s00167-011-1402-7
Muoneke HE, Khan AM, Giannikas KA, Hagglund E, Dunningham TH (2003) Secondary resurfacing of the patella for persistent anterior knee pain after primary knee arthroplasty. J Bone Joint Surg (Br) 85:675–8
Parvizi J, Mortazavi SM, Devulapalli C, Hozack WJ, Sharkey PF, Rothman RH (2012) Secondary resurfacing of the patella after primary total knee arthroplasty does the anterior knee pain resolve? J Arthroplasty 27:21–6. doi:10.1016/j.arth.2011.04.027
Scheurer P, Reininga IH, van Jonbergen HP, van Raay JJ (2015) Secondary patellar resurfacing following total knee arthroplasty : a cohort study in fifty eight knees with a mean follow-up of thirty one months. Int Orthop 39(7):1301–1306. doi:10.1007/s00264-015-2684-z
Daniilidis K, Vogt B, Gosheger G, Henrichs M, Dieckmann R, Schulz D, Hoell S (2012) Patellar resurfacing as a second stage procedure for persistent anterior knee pain after primary total knee arthroplasty. Int Orthop 36:1181–3. doi:10.1007/s00264-011-1463-8
Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 71:262–7. doi:10.1080/000164700317411852
Lygre SHL (2010) Pain, function and risk of revision after primary knee arthroplasty. PhD Thesis. Univerity of Bergen
Brooks R (1996) EuroQol: the current state of play. Health Policy 37:53–72
Greiner W, Weijnen T, Nieuwenhuizen M, Oppe S, Badia X, Busschbach J, Buxton M, Dolan P, Kind P, Krabbe P, Ohinmaa A, Parkin D, Roset M, Sintonen H, Tsuchiya A, de Charro F (2003) A single european currency for EQ-5D health states. Results from a six-country study. Eur J Health Econ 4:222–31. doi:10.1007/s10198-003-0182-5
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee injury and osteoarthritis outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96. doi:10.2519/jospt.1998.28.2.88
Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP (2001) Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty 16:740–7. doi:10.1054/arth.2001.23922
Dolan P, Sutton M (1997) Mapping visual analogue scale health state valuations onto standard gamble and time trade-off values. Soc Sci Med 44:1519–30
Charnley J (1972) The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 54:61–76
Correia J, Sieder M, Kendoff D, Citak M, Gehrke T, Klauser W, Haasper C (2012) Secondary patellar resurfacing after primary bicondylar knee arthroplasty did not meet Patients’ expectations. Open Orthop J 6:414–8. doi:10.2174/1874325001206010414
Lygre SH, Espehaug B, Havelin LI, Vollset SE, Furnes O (2010) Does patella resurfacing really matter? Pain and function in 972 patients after primary total knee arthroplasty. Acta Orthop 81:99–107. doi:10.3109/17453671003587069
Spencer SJ, Young D, Blyth MJ (2010) Secondary resurfacing of the patella in total knee arthroplasty. Knee 17:187–90. doi:10.1016/j.knee.2009.08.003
Picavet HS, Schouten JS (2003) Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain 102:167–78
Fillingim RB (2000) Sex, gender, and pain: women and men really are different. Curr Rev Pain 4:24–30
Espehaug B, Furnes O, Havelin LI, Engesaeter LB, Vollset SE, Kindseth O (2006) Registration completeness in the Norwegian arthroplasty register. Acta Orthop 77:49–56. doi:10.1080/17453670610045696
Howell J, Xu M, Duncan CP, Masri BA, Garbuz DS (2008) A comparison between patient recall and concurrent measurement of preoperative quality of life outcome in total hip arthroplasty. J Arthroplasty 23:843–9. doi:10.1016/j.arth.2007.07.020
Acknowledgments
We would like to thank the NAR for allowing us to access the register dataset and all Norwegian orthopaedic surgeons for reporting their surgical cases to the NAR. Many thanks also go to all patients who gave their consent to be entered into the NAR database as well as for their willingness to participate and respond to the survey on which this study was also based.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The NAR is financed by the Western Norway Regional Health Authority (Helse-Vest) and Helse Bergen. During this study, THL received a study grant from the Department of Orthopaedic Surgery and from the Health Research Program at Haukeland University Hospital.
Conflict of interest
No competing interests declared.
Rights and permissions
About this article
Cite this article
Leta, T.H., Lygre, S.H.L., Skredderstuen, A. et al. Secondary patella resurfacing in painful non-resurfaced total knee arthroplasties. International Orthopaedics (SICOT) 40, 715–722 (2016). https://doi.org/10.1007/s00264-015-3017-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3017-y