Abstract
Purpose
Our study aimed at evaluating age- and gender-specific references describing lower-limb alignment in a large population of children using an accurate and reliable method (EOS 2D/3D).
Methods
From our database, we selected 523 EOS records suitable for 3D modelling representing age groups between two and 16 years in which no relevant deviation influencing lower-limb biomechanics could be observed (the majority of the examined population had mild scoliosis). We performed reconstruction of both lower limbs, thus obtaining the value of the mechanical tibiofemoral angle (mTFA) and the femoral mechanical axis–femoral shaft angle (FM-FS) and calculated the anatomical tibiofemoral angle (aTFA) from previous parameters. Statistical analysis was carried out using the Kolmogorov–Smirnov test, Spearman correlation, regression analysis and Welch test.
Results
The aTFA reaches its maximum by the age of three years: 13.07° in boys and 10.73° in girls; it then varies ∼4.44° in both genders. By the age of three years, the mTFA reaches 8.04° in boys and 4.85° in girls; it starts to decrease to −1.47° in boys and 0.13° in girls. By the age of three years, FM-FS increases to 5.02° in boys, then fluctuates at ∼4.08°, while in girls, it increases to 5.87°, then fluctuates at ∼4.24°.
Conclusions
The pattern found in this study confirms the results of previous publications investigating Caucasian populations; however, absolute values differ significantly in several cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Axis deviation of the lower limb frequently occurs in clinical practice. Although changes in anatomical and biomechanical parameters during childhood are well known, these conditions may be a reason of concern for parents and relatives, who usually seek medical advice [1–3]. Based on a consensus, normal ranges of axis deviation are given in ±2 standard deviations (SD) for age- and ethnic-specific values. This comprises a broad spectrum covering almost all parameters, but a more precise definition of these ranges is needed, since deviations may indicate numerous pathological processes (e.g. rickets, phosphate diabetes, renal osteodystrophy, Marfan syndrome). On the other hand, changes in the sensitive biomechanical balance may lead to numerous orthopaedic disorders (e.g. axis deviation of the lower limb in childhood is an independent risk factor of knee osteoarthritis). Consequently, specifying values requiring surgical or conservative correction is useful. Considering the outstanding clinical importance of this topic, its widespread appearance in the literature is not surprising. Nevertheless, these studies are not uniform regarding either nomenclature or methods. Moreover, the number of patients is usually low in such studies; therefore, comparing results between studies is difficult.
To evaluate lower-limb alignment, both physical examination and imaging techniques are used in clinical practice. Some physical methods can be appropriate for estimating lower-limb alignment, but limitations in their accuracy should be taken into consideration [4]. In regards to imaging techniques, only full-length standing anteroposterior (AP) lower-limb radiographs provide precise evaluation, since the mechanical axis cannot be evaluated on short knee AP radiographs; additionally, deviations (e.g. proximal coxa vara or distal tibia vara) may remain hidden [5]. Patient positioning is also crucial in full lower-limb radiography, as inaccurate positioning may lead to measurement differences, as published by Thelen et al. [6]. Patella-ahead and posterior condyle alignments, which are widespread in clinical practice, can lead to misinterpretation, since patellar malalignment and condylar asymmetry are common deviations [5]. Difficulties in measuring mechanical parameters have led to a limited number of appropriate studies in childhood. Sabharwal and Zhao evaluated their records by using patella-ahead alignment without describing gender-specific differences [7].
The multiwire chamber, which earned Georges Charpak the 1992 Nobel Prize in Physics, has led to a revolutionary new imaging technique called EOS 2D/3D imaging system (EOS Imaging, Paris, France) [8]. The device produces weight-bearing, whole-body simultaneous AP and lateral imaging with the help of co-linked pairs of X-ray tubes and detectors moving together vertically. The use of ultra-low-dose radiation is a prominent advantage of this technique, since bidirectional, full-body imaging of an adult results in <0.30 mGy radiation dose [9–11]. This advantage is especially important in paediatric orthopaedic patients. Another significant advantage of this technology is that during examination, the patient is in a standing, weight-bearing position, which enables the examination of mechanical parameters. The system’s sterEOS 3D software makes possible preparation of 3D models from the records (by fitting a general model). In the beginning, it was only available when imaging the spine, but software development made it possible to reconstruct the lower limb and pelvis or to model hip arthroplasty [6, 9, 12–15]. Several articles dealt with the authenticity and applicability of 3D modelling in the recent past, but among these, only Gheno et al., Assy et al. and our department have investigated children and adolescents [13, 16–18]. All publications stated that EOS technology is suitable and reliable for measuring biomechanical parameters of the lower limb [15–19]. Limitation of the method is that it is based on a general model and is not suitable for 3D reconstruction of severe deformities, e.g. fractures or tumours.
The aim of our study was to determine age- and gender-specific reference intervals of lower-limb alignment in a large paediatric population with the help of a precise, distortion-free method (EOS 2D/3D).
Materials and methods
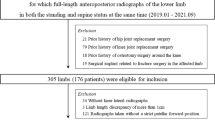
In this study, we evaluated the results of EOS 2D/3D radiographs obtained at the Department of Orthopaedics, University of Pécs, between 2007 and 2012. Of the 7108 records, we selected 2360 cases representing the two to 16-year-old age group. All radiographs were taken for orthopaedic indications. We selected 727 cases in which there were no previous surgical interventions or deviations influencing biomechanics of the lower limbs. Cases in which anamnesis revealed any disorders that may influence growth were excluded. 3D modelling was unsuccessful in 204 cases (28 % of all samples) because reliable identification of femoral trochanters and condyli was impossible due to incorrect positioning. Distribution of the remaining 523 cases and their proven diagnosis is summarised in Table 1.
For this type of retrospective study, formal patient consent was not required; however, before radiological examinations, written informed consent was obtained from all individuals’ parents or guardians, including permission to use images for research purposes.
Radiographs were taken in a standardised step-forward position (right leg forward 8–10 cm). EOS 3D v1.4.4.5297 software was used for data processing. 3D modelling of both lower limbs was performed in the four to 16-year-old age group, resulting in 1022 models. In the two to three year-old age group, total 3D modelling was not possible due to the uncertainty of epiphyseal cartilages; in these cases, we used the software’s lower-limb alignment mode, performing this measurement on 24 limbs.
All models were prepared by the same specially trained doctor having 2.5 years’ experience in lower-limb 3D modelling, thus excluding interobserver error. Intraobserver reliability was evaluated in 30 randomly chosen cases (including 28 full 3D and two lower-limb alignment modelling) on three different days. Criteria determined by Winer were used for the evaluation [20].
The measured parameters were the following:
-
(1)
Mechanical tibiofemoral angle (mTFA) or hip-knee-ankle angle represents the angle between the mechanical axis of the femur and the mechanical axis of the tibia in the frontal plane of the knee (varus position negative, valgus positive) (Fig. 1a); this value is automatically calculated by the EOS 3D software.
Fig. 1 Mechanical tibiofemoral angle: a Represented in 3D EOS reconstructions of pathological lower limbs from our database. FMA femoral mechanical axis, mTFA mechanical tibiofemoral angle, LBA load-bearing axis, TMA tibial mechanical axis. b Mean values ±2 standard deviations (SD) of the mTFA. c Scatterplot and linear regression of mTFA with age. Dashed lines represent the 95 % confidence interval (CI) upper/lower limits of the linear regression coefficient
-
(2)
FM-FS or HKS angle represents the angle between the femoral mechanical and anatomical axes in the frontal plane of the knee (Fig. 2a); this value is also automatically calculated by the EOS 3D software.
Fig. 2 Femoral mechanical axis–femoral shaft angle (FM-FS): a FM-FS angle represented in 3D EOS reconstructions of pathological lower limbs from our database. FMA femoral mechanical axis, FSA femoral-shaft axis). b Mean values ±2 standard deviations (SD) of the FM-FS. c Scatterplot and linear regression of the FM-FS with age. Dashed lines represent 95 % confidence interval (CI) upper/lower limits of the linear regression coefficient
-
(3)
The aTFA or knee angle represents the angle between the anatomical femoral and tibial axes (varus position negative, valgus positive); this value was calculated from the difference between mTFA and FM-FS (Fig. 3a).
Fig. 3 Anatomical tibiofemoral angle (aTFA). a The aTFA represented in 3D EOS reconstructions of pathological lower limbs from our database. FSA Femoral shaft axis, TSA tibial shaft axis. b Mean values and ±2 standard deviations (SD) of the aTFA. c Scatterplot and linear regression of the aTFA with age. Dashed lines represent upper/lower 95 % confidence interval limits for the linear regression coefficient
Statistical analysis of data was carried out using SPSS v22 (IBM Corp., Armonk, NY, USA) and Microsoft Office Professional Plus v14.0.6112.5000 (Microsoft Corp., Redmond, WA, USA) software applications. Intraobserver reliability was investigated using the intraclass correlation coefficient (ICC). The investigated parameter and laterality were evaluated by paired samples t test. Normality of data was checked using the Kolmogorov–Smirnov test. Relationship between measured data and age was evaluated using Spearman correlation and regression analysis, while differences between genders were analysed using the Welch test; p < 0.05 was accepted as significant.
Results
Operator intra-observer reliability was excellent (ICC in full 3D modelling mode: mTFA, 0.95; FM-FS, 0.98; and lower-limb alignment mode: mTFA, 0.99; FM-FS, 0.99). No parameter studied showed correlation with laterality; therefore, average values of the two sides were used in further calculations. Considering the entire sample, the Kolmogorov–Smirnov test was significant in all examined parameters. The year-wise distribution of samples showed they did not differ significantly from normal distribution (Table 2).
In boys, the mTFA increased from 5.5° to 8.0° between the ages of 2 and 3, decreased to -0.9° by the age of 8 years, fluctuated at ∼0.3° and finally decreased to −1.8° at the age of 15–16 years. In girls, it increased from 2.5° to 4.9° between the ages of two and three, decreased to 0.9° then showed a slight increase until finally fluctuating at ∼0.5° (Table 3, Fig. 1).
FM-FS was similar to tibiofemoral angle, but its changing amplitude was much smaller. In boys, it increased from 3.9° to 5.0°, then after a slight decrease, it fluctuated at ∼4.1° until the age of 16 years. In girls, it increased from 4.1° to 5.9°, then after a slight decrease, it fluctuated at ∼4.2° (Table 3, Fig. 2). The aTFA was 9.4° in two year-old boys and 6.6° in two year-old girls; then it increased and reached its maximum by the age of three years, with 13.1° in boys and 10.7° in girls. After this, it decreased to 3.0° at the age of eight then fluctuated at ∼4.4° until the age of 14 and finally decreased to 2.7° at the age of 15–16 years in boys. In girls, it decreased to 4.6° at the age of six, then after a slight increase, fluctuated at ∼4.6° (Table 3, Fig. 3). All three examined parameters showed linear correlation with age. The aTFA and mTFA were also gender-related, and there was a strong correlation between aTFA and mTFA (p < 0.00; correlation coefficient = 0.882) (Table 2).
Discussion
To the best of our knowledge, this is the first time that normal ranges of anatomical and biomechanical parameters influencing lower-limb alignment have been reported in the two to 16-year-old age group with the help of an equipment enabling precise and accurate radiological analysis; additionally, parameters were analysed according to gender and age groups in this large population.
Similarly to Assi et al. and Gheno et al., we found the EOS 3D technology to be a reliable method for evaluating biomechanical parameters of the lower limb both in children and adolescents, even though the presence of epiphyseal cartilage may cause some uncertainty and may prolong 3D reconstruction time in children <ten years [13, 16–18].
In the case of mTFA, we observed valgus position at the age of two years, which corresponds to results of Sabharwal and Zhao [7]; however they measured a smaller deviation from neutral. In our study, the mechanical valgus position reached its maximum by the age of three years, as opposed to the maximum by the age of two years as reported Sabharwal and Zhao. After this, neutralisation can be observed in both sexes; maximal mechanical axis deviation from neutral was 2.2°. In boys, deviation was much greater, and the varus position can also be observed several times; it was most prominent by the age of 15 years, with a value of 2.2°. This deviation was much smaller in girls, and an important difference in girls is that a definitive varus position did not appear. This changing pattern corresponds to the results of Sabharwal and Zhao except that their results showed <0.6° fluctuation after the age of seven; however, they also found a slight varisation tendency after the age of 15 years, which is similar to our finding [7].
Although the maximum at the age of three years was noticeable for FM-FS, after a moderate decrease, this value fluctuated at ∼4.2°. Compared with the other two parameters, this change was not so large, since there were barely more than 2° between end values. Unlike in our study, Sabharwal and Zhao found no peak at two to three years of age in aTFA and mTFA; however, fluctuation measured by those authors was also within 2°, although they reported an average of 6.6° [7].
The changing pattern of aTFA correlates with results of previous publications. Our results confirm former data reporting that varus position present at birth changes to valgus by the age of two years. Valgus value of 9.1° measured by Sabharwal and Zhao [7] is very similar to our data measured at the age of two; other authors found smaller values. In our study, valgus position reached its maximum at the age of three, similar to results of most previous publications. According to Sabharwal and Zhao, valgus value reached maximum at the age of two; however, it changed only slightly until the age of five. In the study of Yoo et al., maximal valgus position was found by the age of four, while Saini et al. found it in six-year-old children only. In children older than eight years, our data fluctuated at ∼4.5° and decreases to 3.76° by the age of 16. This corresponds to reports from most of other authors—except for Cheng et al., who found fluctuation at ∼0.5°. Conversely, other authors found no gender specificity, although Cahuzac et al. found a difference in the 13- to 16-year age group. In comparison, our results showed significant differences in the entire population. (Fig. 4). We assume, that this may be explained by differences in the dynamics of sexual maturity, since by the age of seven or eight, girls have already begun their rapid-height-growth phase, while this occurs by the age of nine to ten in boys. This shift may also explain the differences found in the 15- to 16-year-old age group, because girls’ growth rate decreases significantly compared with boys at this age [1–3, 7, 21–25].
We also found strong correlation between aTFA and mTFA, indicating that the FM-FS has no compensatory role, since an mTFA strongly deviating from the average is always accompanied by a similarly strongly deviating aTFA [7].
Our study is limited by the fact that most optimal study group would be a completely healthy group of individuals without any orthopaedic complaints, but the use of ionising radiation in their case (especially in childhood) is ethically unacceptable. Accordingly, we processed pictures of such children who attended our outpatient clinic. The possible distortion effect of the examined population’s orthopaedic pathologies (mainly mild scoliosis) must also be noted. Another limitation of our retrospective study is the fact that the examined population did not show a normal distribution regarding gender and age. The low number of two to three year-olds can also influence results. After discussion with a biostatistical specialist, we concluded that the distorting effect of the low number of study participants is of little significance compared with the importance of the valgisation tendency to end at the age of three years. Another deficiency of our study is that no children younger than two years were examined. This is because EOS examination requires that the patient should stand alone safely and motionless, which cannot be carried out in the under-two age group.
References
Engel GM, Staheli LT (1974) The natural history of torsion and other factors influencing gait in childhood. A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop Relat Res 99:12–17
Heath CH, Staheli LT (1993) Normal limits of knee angle in white children--genu varum and genu valgum. J Pediatr Orthop 13:259–262
Salenius P, Vankka E (1975) The development of the tibiofemoral angle in children. J Bone Joint Surg Am 57:259–261
Kraus VB, Vail TP, Worrell T et al (2005) A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum 52:1730–1735. doi:10.1002/art.21100
Cooke TD, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34:1796–1801
Thelen P, Delin C, Folinais D et al (2012) Evaluation of a new low-dose biplanar system to assess lower-limb alignment in 3D: a phantom study. Skeletal Radiol 41:1287–1293. doi:10.1007/s00256-012-1438-x
Sabharwal S, Zhao C (2009) The hip-knee-ankle angle in children: reference values based on a full-length standing radiograph. J Bone Joint Surg Am 91:2461–2468. doi:10.2106/JBJS.I.00015
Charpak G (1996) Prospects for the use in medicine of new detectors of ionizing radiation. Bull Acad Natl Med 180:161–168, discussion 168-169
Illés T, Somoskeöy S (2012) The EOS™ imaging system and its uses in daily orthopaedic practice. Int Orthop 36:1325–1331. doi:10.1007/s00264-012-1512-y
Deschênes S, Charron G, Beaudoin G et al (2010) Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976) 35:989–994. doi:10.1097/BRS.0b013e3181bdcaa4
Dietrich TJ, Pfirrmann CW, Schwab A et al (2013) Comparison of radiation dose, workflow, patient comfort and financial break-even of standard digital radiography and a novel biplanar low-dose X-ray system for upright full-length lower limb and whole spine radiography. Skeletal Radiol 42:959–967. doi:10.1007/s00256-013-1600-0
Chaibi Y, Cresson T, Aubert B et al (2012) Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Engin 15:457–466. doi:10.1080/10255842.2010.540758
Assi A, Chaibi Y, Presedo A et al (2013) Three-dimensional reconstructions for asymptomatic and cerebral palsy children’s lower limbs using a biplanar X-ray system: a feasibility study. Eur J Radiol 82:2359–2364. doi:10.1016/j.ejrad.2013.07.006
Lazennec JY, Brusson A, Dominique F et al (2014) Offset and anteversion reconstruction after cemented and uncemented total hip arthroplasty: an evaluation with the low-dose EOS system comparing two- and three-dimensional imaging. Int Orthop. doi:10.1007/s00264-014-2616-3
Journé A, Sadaka J, Bélicourt C et al (2012) New method for measuring acetabular component positioning with EOS imaging: feasibility study on dry bone. Int Orthop 36:2205–2209. doi:10.1007/s00264-012-1650-2
Gheno R, Nectoux E, Herbaux B et al (2012) Three-dimensional measurements of the lower extremity in children and adolescents using a low-dose biplanar X-ray device. Eur Radiol 22:765–771. doi:10.1007/s00330-011-2308-y
Schlégl AT, Szuper K, Somoskeöy S et al (2014) Evaluation of the usefulness of the EOS 2D/3D system for the measurement of lower limbs anatomical and biomechanical parameters in children. Orv Hetil 155:1701–1712. doi:10.1556/OH.2014.30009
Szuper K, Schlégl Á, Leidecker E et al (2015) Three-dimensional quantitative analysis of the proximal femur and the pelvis in children and adolescents using an upright biplanar slot-scanning X-ray system. Pediatr Radiol 45:411–421. doi:10.1007/s00247-014-3146-2
Folinais D, Thelen P, Delin C et al (2013) Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop Traumatol Surg Res 99:509–516. doi:10.1016/j.otsr.2012.12.023
Winer BJ (1971) Statistical principles in experimental design. McGraw Hill, New York, pp 283–293
Saini UC, Bali K, Sheth B et al (2010) Normal development of the knee angle in healthy Indian children: a clinical study of 215 children. J Child Orthop 4:579–586. doi:10.1007/s11832-010-0297-z
Cheng JC, Chan PS, Chiang SC et al (1991) Angular and rotational profile of the lower limb in 2,630 Chinese children. J Pediatr Orthop 11:154–161
Cahuzac JP, Vardon D, Sales de Gauzy J (1995) Development of the clinical tibiofemoral angle in normal adolescents. A study of 427 normal subjects from 10 to 16 years of age. J Bone Joint Surg Br 77:729–732
Yoo JH, Choi IH, Cho TJ et al (2008) Development of tibiofemoral angle in Korean children. J Korean Med Sci 23:714–717. doi:10.3346/jkms.2008.23.4.714
Joubert K, Mag K, van’t Hof M et al (2006) The growth rate of height between the ages of 3 and 18 around the millennium in Hungary (on the basis of the Hungarian Nation-wide Representative Longitudinal Growth Study. Gyermekgyógy 5:517–527
Acknowledgments
No benefits in any form have been received or will be received from a commercial party related, directly or indirectly. The authors declare that there are no potential conflicts of interest in connection with this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schlégl, Á.T., Szuper, K., Somoskeöy, S. et al. Three dimensional radiological imaging of normal lower-limb alignment in children. International Orthopaedics (SICOT) 39, 2073–2080 (2015). https://doi.org/10.1007/s00264-015-2851-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2851-2