Abstract
Introduction
A novel hand-held navigation combines gyroscopes, accelerometers and a secure local wireless channel to guide the distal femoral and proximal tibial cutting positions by displaying to the surgeon directly on the pods within the surgical field. No previous study has reported on its accuracy.
Materials and methods
A prospective randomized controlled trial was performed to compare radiographic outcomes in minimally invasive surgery total knee arthroplasty (MIS-TKA) with (40 patients, 40 knees) and without (40 patients, 40 knees) the novel hand-held navigation.
Results
The use of hand-held navigation resulted in fewer outliers (> ± 3° malalignment) in all frontal alignment: the hip-knee-ankle, the femoral component, and the tibial component. Tibial slope was also better achieved with the navigation. Femoral component flexion was not significantly different. Operation time and bone cutting time with the navigation were not longer than those without. Blood loss from drainage was not significantly different.
Conclusion
The hand-held navigation improves accuracy for mechanical alignment and positioning of the prosthesis without additional surgical time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Restoration of the mechanical alignment is an important consideration during total knee arthroplasty (TKA). Many studies confirm that postoperative mechanical axis within 3° of varus or valgus is crucial to achieve the best long-term survival [1–3]. In the last few years, a number of technologies have therefore been developed to aid the surgeon in achieving a better alignment in knee arthroplasty, including computer-assisted surgery (CAS) based on line-of-sight navigation, patient-matched guides based on pre-operative imaging, and most recently, the new system of CAS: the hand-held navigation. Although several meta-analyses demonstrate that the former CAS-TKA provides a significant improvement in prosthesis alignment and component position, it is perceived to be complex and requires more surgical time with a learning curve, and there is also the possibility of complications such as fracture from the guidance pins [4, 5]. With these potential pitfalls, a new hand-held computer assisted stereotaxic surgical instrument system called iAssist navigation was developed to assist the surgeon in the positioning of prosthetic components intra-operatively. It employs surgical instruments and position sensors to determine alignment axes in relation to anatomical landmarks and to precisely position alignment instruments and implant components relative to these axes. This study conducted a prospective, randomized, controlled trial to compare accuracy of knee alignment and component positioning of MIS-TKA performed with and without the hand-held navigation.
Materials and methods
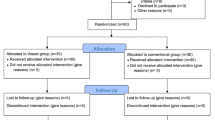
This prospective, randomized controlled study was approved by the ethical committee of our institution (COA57/2557). All patients with knee osteoarthritis whose symptoms could not be treated with conservative measure were admitted under the care of one surgeon for a primary minimally invasive total knee arthroplasty (MIS-TKA). Both varus and valgus deformity cases were included in this trial. Patients were excluded from the trial if they had deformity from a previous fracture and/or osteotomy, less than 90° of range of motion (ROM), or more than 30° of flexion contracture. Patients were randomly assigned to each of the two arms with random permuted blocks of four. The patients flow chart is summarized in Fig. 1. Both the patients and the investigators measuring the final outcomes were blinded with regard to the trial arm to which the patient had been assigned.
A total of 80 patients (80 knees) who underwent MIS-TKA were randomized into two groups. Group I (iAssist-MIS-TKA group; 40 patients, 40 knees) was operated using the iAssist navigation (iAssist Knee System, Zimmer, US) (Fig. 2). Group II (MIS-TKA group; 40 patients, 40 knees) was operated using the same minimally invasive technique but without the hand-held navigation (Fig. 3). Pre-operative clinical variables such as age, sex, body mass index, number of co-morbidities, side, range of motion, and Knee Society scores (KSS) [6] were recorded. All surgery was performed by one experienced surgeon (ST) who had experience with the use of computer navigation and the standard instruments. In addition, to ensure that the surgeon has excelled in the surgical technique before the start of this study, he had performed more than 30 operations with iAssist-MIS-TKA.
Use of hand-held navigation (iAssist) in minimally invasive total knee arthroplasty to guide to resect distal femur and proximal tibia. After femoral registration (a, b), femoral landmarking and varus/valgus and flexion/extension adjustments were performed (c) to allow accurate resection (d). The tibial landmarking (e) and registration (f) were performed before varus/valgus and anterior/posterior slope angles were set, and the bone was resected (g)
Minimally invasive total knee arthroplasty (MIS-TKA) using an intramedullary cutting guide to resect distal femur (a, b) and extramedullary cutting guide to resect proximal tibia (c). The size of distal femur was determined (d). The femoral anteroposterior cut was made following the selection of femoral sizing and rotation (e).The tibial and femoral trial components were inserted (f). The tibial and femoral components were inserted with cement (g)
All procedures were performed using the same fixed-bearing posterior stabilized implant (NexGen HiFlex, Zimmer, US) without patellar resurfacing and using a minimally invasive technique. Patients had a regional anaesthetic unless contraindicated by a medical issue. The tourniquet pressure was at 280 mmHg in all cases. The incision was typically less than 9 cm long, which represented no more than twice the length of the patella. A mini-midvastus approach was made, which allowed for exposure of the knee without everting the patella. The iAssist-MIS-TKA was performed using the iAssist navigation system. Briefly, iAssist Knee pods were calibrated, and each pod was installed on its respective instrument. After femoral registration, femoral landmarking and varus/valgus and flexion/extension adjustments were performed. Then, the femur was resected, and the cut was validated. Next, the tibial landmarking and registration were performed before varus/valgus and anterior/posterior slope angles were set, and the bone was resected and validated. The hand-held navigation system was used to guide the two main bone cuts in both coronal and sagittal plane as well as to validate the final bone cut. For the MIS-TKA group, the distal femoral resection was performed using the intramedullary technique and the proximal tibial resection was performed by extramedullary technique. Femoral and tibial components were cemented in all cases.
Both groups had the same postoperative pain control and rehabilitation consisting of a multimodal approach, which aims to avoid parenteral narcotics and provide early postoperative mobilization.
Perioperative parameters (operative time, bone cutting time and blood loss) and radiographic alignment at six weeks postoperation were evaluated by two independent investigators who were blinded to the trial interventions. The average of the two results was used in the analysis. For anteroposterior and lateral weight-bearing hip-to-ankle standing radiographs, the feet were placed apart with the knees in maximum extension and the toes pointing straight. The radiographs were evaluated (Fig. 4) by measuring five component angles: (1) hip-knee-ankle (HKA) angle, which is an angle formed between the mechanical axis of the femur and the mechanical axis of the tibia as measured on the lateral side of the midline (the mechanical axis of the femur is defined as the line connecting the centre of the femoral head with the center of the knee, and the mechanical axis of the tibia is defined as the line connecting the centre of the ankle mortise with the centre of the knee, with 180° as the target angle, (2) coronal femoral angle, which is an angle formed between the mechanical axis of femur and the transcondylar line of the femoral component as measured on the lateral side, with 90° as the target angle, (3) coronal tibial angle, which is an angle formed between the mechanical axis of the tibia and the tibial base plate as measured on the lateral side, with 90° as the target angle, (4) sagittal femoral angle, which is an angle of femoral component flexion as measured between the frontal femoral cortex and the inner frontal part of the femoral component; a large angle indicates high degree of femoral component flexion, with a 3° flexion as the target angle, and (5) sagittal tibial angle, which is an angle of posterior slope of the tibial component as measured posteroinferiorly from the line perpendicular to the midline of tibia, with a 7° posterior slope as the target angle.
Statistical analysis of measurements of malalignment was performed. Up to 3° of deviation from the target angle was considered acceptable, whereas values outside of this range were classified as outliers.
The bone cutting time was defined as the time elapsed between impacting the femoral spike into the distal femur in group I or the insertion of the intramedullary femoral guided rod in group II and when the trial components placement were completed. Skin-to-skin operative time was recorded. Any complications during the study and amount of blood loss from drainage were also recorded.
Statistical analysis
From our preliminary study, a mean difference in the HKA angle deviation between the two groups was 1.5° with a standard deviation (SD) of 1.9° and 2.4° for the groups with and without navigation, respectively. The sample size was therefore estimated to be 33 knees per group to ensure sufficient power of 80 with a significant difference (α = 0.05, two-sided significance level). In order to compensate for 10 % of patients who were lost to follow-up, we recruited at least 37 knees per group to ensure sufficient sample size to reach the significant level.
Demographic and preoperative data of both groups were compared with independent t-test (Student t-test) and chi-square. The clinical and radiographic outcomes of both groups were compared with an independent t-test and chi-square. The p-value < 0.05 indicates a statistically significant difference (SPSS version 21, SPSS Inc, Chicago, IL).
Results
The iAssist-MIS-TKA group (group I) consisted of 32 females and eight males who had an average age of 68.0 ± 8.0 years (range 51–85 years). The MIS-TKA group (group II) consisted of 34 females and six males who had an average age of 65.9 ± 6.3 years (range 54–78 years). Others demographic variables such as pre-operative deformity, body mass index (BMI) and KSS were similar between the two groups (Table 1).
Perioperative and radiographic results at six weeks
Between the two groups, the perioperative results were not significantly different (p > 0.05) (Table 2). Although the amount of blood loss was higher in the MIS-TKA group, the difference was not significant (p > 0.05). Operation time and bone cutting time of the hand-held navigation group were not significantly longer than the group without the navigation (p > 0.05).
To assess the accuracy of the operations in the two groups at the six-week follow-up, angle deviation and percentage of knees with the implant aligned out of ±3 degrees from the target angle were used as indicators by considering five angles (HKA angle, coronal femoral angle, coronal tibial angle, sagittal femoral angle, and sagittal tibial angle) (Table 3).
Discussion
Many advances in technology have been implemented to improve implant alignment in TKA. For instance, meta-analysis of imageless CAS for TKA significantly reduces the number of outliers in the limb mechanical axis, coronal position of the femoral component, and coronal position of the tibial components by rates of approximately 80 %, 87 %, and 80 %, respectively [4]. Nevertheless, CAS still has some drawbacks such as the increased operative time of 20 minutes on average, increased extra costs for hardware and software, and long learning curve for surgeons [4, 7–10].
In the last few years, the pinless navigation was introduced to check coronal and sagittal alignment without the need for intracortical pin fixation. This technique reduces number of steps of the registration procedure normally required in the conventional navigation technique. It was found that the pinless navigation was more effective than the conventional alignment jigs in TKA as it reduced HKA outliers > ± 3° (5 % vs 25 %). However, the duration of surgery in the pinless group was significantly longer than in the conventional group [11].
Recently, patient-specific guides (PSGs) have been introduced as the new instrument to improve alignment and reduce operative time because it utilizes MRI or CT to tailor a patient-specific instrument before the operation. This pre-operative planning of PSGs has an advantage over the computer navigation which requires intra-operative bone registration. However, PSGs also have several disadvantages such as increased costs for imaging and instrument fabrication as well as increased pre-operative time required for surgical planning. PSGs also do not seem to be able to result in the same degree of accuracy as the CAS system [12–14].
Evidently, while these technologies have distinct advantages, there is room for improvement such as time efficiency, cost effectiveness, complication rate, and reproducibility with minimal learning curve [15]. Therefore, a new hand-held navigation system called iAssist navigation was developed in 2012 by employing inertial electronic components or gyroscopes to pass the information through a secure local wireless channel [16–19]. The system can be used to position the distal femoral and proximal tibial cutting guides in a real-time manner. Therefore, the system considerably reduces the complexity of the previous imageless computer navigation systems.
Previously, Scuderi et al. [19] conducted a study that compared accuracy between the imageless navigation system and the iAssist hand-held navigation system. The study found that the initial clinical values measured on CT showed a good correlation to actual validation measurements from the hand-held system. The femoral mechanical axis showed an average accuracy of 0.4 ± 0.95° between the validated bone surface and the postoperative CT. Tibial measurements of the mechanical axis were also proven to be accurate, with an average error of 0.70 ± 1.07°. Tibial slope results were reproducible, with errors of −0.05° ±0.78°.
Unlike the study of Scuderi et al., our study aimed to compare the accuracy between the standard instrument and the iAssist hand-held system. From our result, the use of the hand-held navigation resulted in fewer outliers in frontal alignment, all for the entire TKA, the femoral component separately, and for the tibial component separately. Tibial slope was also achieved better with hand-held navigation. The femoral component flexion was not significantly different by the hand-held navigation.
In addition, our study considered other important outcomes such as operative time and blood loss. Previously, one of the major drawbacks for the imageless CAS-TKA is the longer bone cutting time; however, such drawback does not seem to be the limitation of the hand-held navigation because this study found that the bone cutting time of the iAssist-MIS-TKA group was only marginally longer than and not significantly different from the MIS-TKA group. For the iAssist-MIS-TKA group, blood loss was found to be reduced but not significantly.
However, the limitation in this study is that we did not use CT scans to determine alignment. To reduce the error of alignment evaluation, we therefore performed strictly controlled radiographic positioning.
In conclusion, the initial experience with the hand-held navigation has been positive. The use of this new navigation system for total knee arthroplasty is less complex and less time consuming than the former navigation system. Most importantly, the use of this new technology also provides better accurate alignment than the conventional MIS-TKA.
References
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 24(4):570–578. doi:10.1016/j.arth.2008.03.002
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg (Br) 73(5):709–714
Brin YS, Nikolaou VS, Joseph L, Zukor DJ, Antoniou J (2011) Imageless computer assisted versus conventional total knee replacement. A Bayesian meta-analysis of 23 comparative studies. Int Orthop 35(3):331–339. doi:10.1007/s00264-010-1008-6
Jung KA, Lee SC, Ahn NK, Song MB, Nam CH, Shon OJ (2011) Delayed femoral fracture through a tracker pin site after navigated total knee arthroplasty. J Arthroplasty 26(3):505 e509–505 e511. doi:10.1016/j.arth.2010.01.006
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Kim YH, Kim JS, Yoon SH (2007) Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. J Bone Joint Surg (Br) 89(4):471–476. doi:10.1302/0301-620X.89B4.18878
Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D (2007) Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am 89(2):261–269. doi:10.2106/JBJS.F.00601
Manzotti A, Cerveri P, Pullen C, Confalonieri N (2014) Computer-assisted unicompartmental knee arthroplasty using dedicated software versus a conventional technique. Int Orthop 38(2):457–463. doi:10.1007/s00264-013-2215-8
Saragaglia D, Picard F, Refaie R (2012) Navigation of the tibial plateau alone appears to be sufficient in computer-assisted unicompartmental knee arthroplasty. Int Orthop 36(12):2479–2483. doi:10.1007/s00264-012-1679-2
Maderbacher G, Schaumburger J, Keshmiri A, Barthel M, Springorum HR, Craiovan B, Grifka J, Baier C (2015) Pinless navigation in total knee arthroplasty: Navigation reduced by the maximum? Int Orthop 39(3):455–460. doi:10.1007/s00264-014-2529-1
Lachiewicz PF, Henderson RA (2013) Patient-specific instruments for total knee arthroplasty. J Am Acad Orthop Surg 21(9):513–518. doi:10.5435/JAAOS-21-09-513
Russell R, Brown T, Huo M, Jones R (2014) Patient-specific instrumentation does not improve alignment in total knee arthroplasty. J Knee Surg. doi:10.1055/s-0034-1368143
Thienpont E, Schwab PE, Fennema P (2014) A systematic review and meta-analysis of patient-specific instrumentation for improving alignment of the components in total knee replacement. Bone Joint J 96-B(8):1052–1061. doi:10.1302/0301-620X.96B8.33747
Lackey WG, Berend ME (2012) Hand-held navigation in total knee arthroplasty. J Bone Joint Surg (Br) 94(11 Suppl A):151–152. doi:10.1302/0301-620X.94B11.30831
Nam D, Weeks KD, Reinhardt KR, Nawabi DH, Cross MB, Mayman DJ (2013) Accelerometer-based, portable navigation vs imageless, large-console computer-assisted navigation in total knee arthroplasty: a comparison of radiographic results. J Arthroplasty 28(2):255–261. doi:10.1016/j.arth.2012.04.023
Nam D, Cross M, Deshmane P, Jerabek S, Kang M, Mayman DJ (2011) Radiographic results of an accelerometer-based, handheld surgical navigation system for the tibial resection in total knee arthroplasty. Orthopedics 34(10):e615–e621. doi:10.3928/01477447-20110826-12
Khan H, Walker PS, Zuckerman JD, Slover J, Jaffe F, Karia RJ, Kim JH (2013) The potential of accelerometers in the evaluation of stability of total knee arthroplasty. J Arthroplasty 28(3):459–462. doi:10.1016/j.arth.2012.07.025
Scuderi GR, Fallaha M, Masse V, Lavigne P, Amiot LP, Berthiaume MJ (2014) Total knee arthroplasty with a novel navigation system within the surgical field. Orthop Clin North Am 45(2):167–173. doi:10.1016/j.ocl.2013.11.002
Acknowledgments
The patients’ expenses for the TKA were covered by a public healthcare program. NK received a scholarship for her MS study from Thailand Graduate Institute of Science and Technology (TGIST), TG-CPMO 01-56-008.
Conflict of interest
ST is a paid consultant for Zimmer. The remaining authors declare that they have no conflict of interest.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thiengwittayaporn, S., Fusakul, Y., Kangkano, N. et al. Hand-held navigation may improve accuracy in minimally invasive total knee arthroplasty: a prospective randomized controlled trial. International Orthopaedics (SICOT) 40, 51–57 (2016). https://doi.org/10.1007/s00264-015-2848-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2848-x