Abstract
Purpose
To provide an anatomical basis for intrusive treatment using an approach through the lateral zones of the lumbar intervertebral foramina (LIF), especially for acupotomology lysis, percutaneous transforaminal endoscopy, and lumbar nerve root block.
Methods
Blood vessels, ligaments, nerves, and adjacent structures of ten cadavers were exposed through the L1–2 to L5–S1 intervertebral foramina and examined.
Results
The lateral zones of the LIF were almost filled by ligaments, nerves, and blood vessels, which were separated into compartments by superior/inferior transforaminal ligaments and corporotransverse superior/inferior ligaments. Two zones relatively lacking in blood vessels and nerves (triangular working zones) were found beside the lamina of the vertebral arch and on the root of the transverse processus. Both the ascending lumbar vein and branches of the intervetebral vein were observed in 12 Kambin’s triangles, and in only seven Kambin’s triangles were without any veins.
Conclusions
Nerves and blood vessels are fixed and protected by transforaminal ligaments and/or corporotransverse ligaments. It is necessary to distinguish the ligaments from nerves using transforaminal endoscopy so that the ligaments can be cut without damaging nerves. Care needs to be taken in intrusive operations because of the veins running through Kambin’s triangle. We recommend injecting into the lamina of the vertebral arch and the midpoint between the adjacent roots of the transverse processus when administering nerve root block. Blind percutaneous incision and acupotomology lysis is dangerous in the lateral zones of the LIF, as they are filled with nerves and blood vessels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lateral zones of the lumbar intervertebral foramina (LIF) are often used as a surgical region for acupotomology lysis [1, 2] (Fig. 1), transforaminal injection or nerve root block [3–5], and transforaminal endoscopy [6–9]. Although usually care is taken with nerves, the blood vessels and ligaments in the LIF have often been ignored by surgeons, and the dangers or complications of these procedures have also been neglected. Acupotomology (acupotomy) is a type of surgical treatment using a fine scalpel (acupuncture knife or needle knife), which was pioneered by Han-zhang Zhu in the 1970s [10, 11] and combines traditional Chinese medicine with modern Western medicine. It has since become widely used in traditional Chinese medicine hospitals and ‘barefoot doctor’ clinics in China (Fig. 1). Blind incision and acupotomology lysis in the LIF has become very popular for treatment of lumbar disc herniation and other conditions affecting this area [2, 12] (Fig. 2). However, it is unclear how lumbar disc herniation can be treated using this method. Approaches via Kambin’s triangle have been considered safe for surgery [13–16] because, according to Kambin [13, 15], there was generally ample room for the introduction of coaxial instruments. Is it correct, however, that this area is really lacking in vessels and nerves? There is also no consensus as to the ligaments present in the LIF [17–21]. However, operations or intrusive treatment here can cause injury to nerves and blood vessels, leading to serious sequelae and iatrogenic injury due to the complexity of this zone [22, 23]. Therefore, research into the anatomy of the LIF is important; thus we carried out a study to try to reconcile the conflicting data that currently exist.
Sketch of percutaneous blind incision and debonding with acupuncture-knife. AK acupuncture-knife, CIL corporotransverse inferior ligament, CSL corporotransverse superior ligament, ID intervertebral disc, ITL inferior transforaminal ligament, SP spinous process, STL superior transforaminal ligament, TA tendinous arcus of intertransverse ligament
Materials and methods
In total, ten cadavers (five adults and five children; provided by the Teaching and Researching Office of Anatomy, Southern Medical University), giving a total of 100 LIFs, were examined. Because of the small number, there was no grouping of the cadavers on the basis of demographic characteristics such as age, sex, ethnicity, height, or weight.
The skin, muscle, and fascia of the posterior and bilateral side of the lumbar spine were removed, exposing the LIF and the adjacent vessels and nerves. The fibers and adipose tissue around the LIF, and the lamina were removed, where necessary, to clearly observe the ligaments, nerves, blood vessels, and their adjacent relation in and around the LIF.
Results
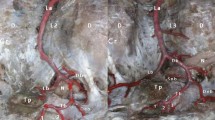
We found that the lateral zones of the LIF were filled with nerves and blood vessels (Fig. 3), and were split into compartments by ligaments (Figs. 4, 5, 6 and 7).
Blood vessels and tendinous arcuss of intertransverse ligament through the lateral zone of L4-5 LIF. ALV ascending lumbar vein, ID intervertebral disc, LN lumbospinal nerve, MNTT triangular working zone of midpoint of neighboring two transverse process root clinging tightly to lamina, SN sympathetic nerve, TA tendinous arcus of intertransverse ligament, TP transverse process
Ligaments
Ligaments in the LIF were classified as follows: obliquely placed bands were considered corporotransverse superior and inferior ligaments, while bands running tranversely were referred to as superior and inferior transforaminal ligaments [19–21].
Transforaminal ligaments
There were two groups of ligaments in the lateral zones of the LIF: the superior and the inferior transforaminal ligaments.
The superior transforaminal ligament is located below the inferior vertebral notch in the lateral zones, which starts from the isthmus periphery and stops at the inferolateral vertebral body on the same vertebral body and outside the posterior longitudinal ligament (Fig. 4). Among the 100 LIFs, 36 superior transforaminal ligaments were found: 9 in L1–2, 12 in L2–3, 11 in L3–4, 5 in L4–5, and none in L5–S1.
The inferior transforaminal ligaments were thick in L1–2 to L3–4, and slender or absent in L4–5 to L5–S1. In some cases, there were two inferior transforaminal ligaments, which started from the junction of the transverse process root and superior articular process, and stopped at the next vertebral body or at the lateral annulus fibrosus and lateral posterior longitudinal ligament (Figs. 5 and 6). Among the 100 LIFs, 45 inferior transforaminal ligaments were found: 16 in L1–2, 11 in L2–3, 14 in L3–4, and 2 in L4–5.
The lateral zones were divided into three compartments: the middle one was the largest, and the superior and inferior compartments were smaller. The upper compartment had superior branches of the intervertebral vein going through it (Figs. 3, 4, 5 and 6); the middle compartment contained a spinal nerve and the spinal nerve branch of the segmental artery; the inferior compartment had inferior branches of the intervertebral vein running through it (Fig. 5).
Corporotransverse ligaments
Almost all the corporotransverse ligaments, which were divided into superior and inferior corporotransverse ligaments, were distributed in the L5–S1L5/–S1 LIF. Parts of these ligaments were combined with the tendinous arches of the intertransverse ligaments at the starting point. The corporotransverse superior ligament ran from the lower transverse process to the inferolateral vertebrae of the same segment, or to the lateral annulus fibrosus or the superolateral part of the lower vertebrae (Fig. 7). The corporotransverse inferior ligament ran from the upper transverse process to the superior outside of the vertebrae of the same segment, and to the lateral annulus fibrosus or superolateral part of the upper vertebrae (Fig. 7).
The lateral zone of the LIF was divided into three compartments: anterosuperior, posterior, and inferior. There were communicating branches of the lumbar sympathetic and anterosuperior branches of the intervertebral vein in the smaller anterosuperior compartment; a posterior branch of the intervertebral vein and a lumbar branch of iliolumbar vessels in the larger posterior compartment; and the L5 nerve and sometimes the inferior intervertebral vein in the smaller anteroinferior compartment (Fig. 7). There were 12 corporotransverse superior ligaments and seven corporotransverse inferior ligaments visible in 20 of the L5–S1L5/–S1 intervetebral foramina.
Tendinous arch of the intertransverse ligament
The tendinous arch of the intertransverse ligament started broadly from the inferior vertebral notch, the inferomedial accessory process, or even the superolateral isthmus, ran downwards to the anterosuperior root of the transverse process and superior articular process, dorsolaterally, tilted from the anteromedial side towards the posterolateral side, along with the posterior branches of the spinal nerve, and was vertical to the branches (Fig. 3). The tendinous arch of the intertransverse ligament was frequently found in the L1–2 to L4–5 LIF lateral zones; the anteroposterior branches of the spinal nerve lay close to this ligament, but none of these branches was seen in the L5/–S1 foramen. The anterior and posterior parts of the tendinous arch were both next to the neurovascular bundle, the anterior part being next to the thick ascending lumbar vein.
Nerves through the lateral zones of LIF
The lumbospinal nerves ran under the superior transforaminal ligaments (Fig. 4) and above the inferior transforaminal ligaments (Figs. 5 and 6). After leaving the LIF, the bifurcation of the anterior and posterior branches lay close to the tendinous arch of the intertransverse ligament, and the spinal nerve rode off on both sides of the tendinous arch of the intertransverse ligament in a “Y” shape (Fig. 3). The sympathetic nerves linked with the spinal nerve anterior branch at the lateral zone (Figs. 3, 4, 5 and 8).
Arteries through the lateral zones of the LIF
The L1–2 to L4–5 lumbar arteries were divided into three groups of terminal branches at the lateral zone of the LIF: the anterior, spinal, and dorsal branch groups (Fig. 8). The iliolumbar artery lumbar branch or L4 artery inferior branch entered the L5/–S1 foramina in some cases (Fig. 7). The anterior branch groups were mainly transverse process anterior branches (anterior branch, transverse process anterior artery). The transverse process anterior branch was the abdominal branch, which was thick and formed many muscle branches along the transverse process anterior part, with the communicating branches and neighboring transverse process anterior branches anastomosing. The extra-spinal arterial nets were comprised of the dorsal branch of the interarticular artery and the upper and lower articular arteries. The upper and lower articular arteries crossed ahead of the tendinous arch of the intertransverse ligament and ran alongside the accompanying vein.
Veins through the lateral zones of LIF
Branching off from the intravertebral vein, the intervertebral vein joined the ascending lumbar vein or the lumbar vein after leaving the foramen. In addition, the root vein joined the ascending lumbar vein or the lumbar vein at the lateral zone with the root artery (Figs. 3, 4, 5 and 7). Meanwhile, the ascending lumbar vein or the lumbar vein accepted the transverse process anterior vein and the subordinate branches of the vertebral lateral vein posterior plexus at the lateral zone of the LIF.
Running from the anteromedial vertebral vein or the anterolateral vein in the lateral recess, the intervertebral vein was divided into a superior branch and an inferior branch, which respectively ran upwards from the superior transforaminal ligament and downwards from the inferior transforaminal ligament. The L5/–S1 foramina tended to lack the inferior branch of the intervertebral artery. The ascending lumbar vein was located on the dorsal side of the anterior branch of the spinal nerve, and adhered to the transverse process root and tendinous arch of the intertransverse ligaments, which collected the superior and inferior branches of the intervertebral veins, the dorsal superior and inferior articular veins, and the transverse process anterior veins at the lateral zones of the LIF. The ascending lumbar vein was constant, although the types and size of the vessels varied greatly.
The triangular working zones
Two zones relatively lacking in blood vessel and nerve (triangular working zones) ran beside the lamina of the vertebral arch and on the root of the transverse processus in the lateral zones of the LIF. One was Kambin’s triangle (Fig. 3) and the other was the midpoint of two neighboring transverse process roots clinging tightly to the lamina (Fig. 3). Kambin’s triangle is often regarded as a suitable approach for numerous lumbar operations because it is thought to have a relative lack of blood vessels and nerves. In this study, we found the ascending lumbar vein and branches of the intervetebral vein in 12 Kambin’s triangles; only seven Kambin’s triangles lacked any veins. These veins had a thin wall and large diameter. The midpoint of the two neighboring transverse process roots clung tightly to the lamina. The base line was composed of the lateral border of the lamina and zygapophyseal joints, while the upper and lower lines respectively comprised the upper and lower articular arteries and veins (Fig. 3).
Discussion
The lower back pain caused by lumbar disc herniation and other cause is a common clinical condition [24–26]. Many surgical treatments focus on the lateral zones of LIF. The anatomical structures of LIF and its lateral zones are complex. Therefore, familiarity with the structure is vital to the safety and efficacy of the treatment. We hope our findings will be of use to pain specialists and spine surgeons who routinely use fluoroscopy and other techniques to access LIF, either percutaneously or by an open method.
The ligaments of the lateral zone of LIF
Golub et al. [21] suggested that the ligaments mentioned above were abnormal tissues and were closely associated with lower back pain, a view that was generally accepted and propagated [18, 20, 27]. Nevertheless, some researches considered them to be normal tissues, functioning as fixation and protection for nerves and vessels, or as mechanical stabilization for the lumbosacral segments [19]. There has therefore been controversy over the issue, although some anatomical and biomechanics experiments have been carried out [17–20, 27]. In the opinion of the acupotomology community, the, ligaments in the lateral zones are important factors in causing lower back pain, and therefore blind incision and acupotomology lysis have formed the basis of treatment for lumbar disc herniation [2, 12]. Based on our findings in the current study, we concluded that these ligaments have the following functions.
-
1.
They act to fix the lumbospinal nerves to the intervetebral foramina and its lateral zone fibers, and protect the nerve from being dragged.
-
2.
They support the lumbospinal nerves. One point often overlooked is that the lateral zones are mostly shaped like a keyhole or a triangle. The inferior transforaminal ligament divides the LIF into a larger upper compartment and a smaller lower compartment. The effective space within these zones would become smaller if the inferior transforaminal ligament were cut, and the nerve would be easily compressed if the nerve root dropped downwards towards the inferior compartment of the intervetebral tubes [28].
-
3.
They protect blood vessels, especially the inferior branch of the intervetebral vein inferior branch, which would be compressed by the spinal nerve without this ligament to protect it.
Blind incision and lysis with acupotomology in lateral zones of the LIF
There have been many reports about blind incision and acupotomology lysis in the lateral zones of LIF. It is considered dangerous and has the potential for injury. In the current study, we found that the transforaminal ligaments occurred mostly in the upper lumbar foramina, but seldom at L4–5 and L5/–S1. However, lumbar intervertebral disc protrusion often involved the L4–5 and L5/–S1 discs. In other words, operations here were meaningless but increased the risk of blood vessels and nerve injuries. The superior transforaminal ligaments clinging to the inferior notch of the pedicle of the vertebral arch could not be cut, but the superior branches of the intervertebral veins were cut according to the operation described in the literature. Blind incision of the inferior transforaminal ligaments was impossible to carry out accurately by acupotomology because of the long distance and the obstruction of the ala of the ilium in the lateral zones of L5/–S1 LIF. In addition, vessels and nerves in the L4-5 or L5/–S1 foramina were vulnerable. As to the corporotranverse ligaments, there was almost complete failure to cut them using acupotomology because of the difficulty in location and abscission by two to three cuts. Therefore, we advise avoiding blind incision in the LIF by acupotomology.
Puncture or nerve root block through the triangular working zones of the LIF
The most common complication of nerve root block via LIF, anesthesia, or injection is injury to blood vessels and nerves. We found that it was better to inject from the midpoint of the two transverse process roots clinging to the lateral border of the vertebral arch and lamina, until a feeling of hollow in operations using nerve blocks in order to reduce injuries to the upper and lower articular arteries and veins. Kambin’s triangle is the approach taken for many lateral lumbar surgeries, and we advised that care should be taken in identifying the veins running through it to avoid injury to the ascending lumbar vein or branches of the intervetebral vein, which were seen in most of the Kambin’s triangles in our study.
References
Guo CQ, Liu NG, Li XH et al (2007) Effect of lysis of acupotomology on plasma vasoactive substance levels in rats with third lumbar vertebra transverse process syndrome. Zhen Ci Yan Jiu 32(5):323–326
Ke Q (2012) Clinical study of needle-knife therapy on treating lumbar disc herniation [EB/OL]. University of Chinese Medicine, Guangzhou
Takeuchi M, Kamiya M, Wakao N et al (2014) A simple, 10-minute procedure for transforaminal injection under ultrasonic guidance to effect cervical selective nerve root block. Neurol Med Chir (Tokyo) 54(9):746–751
Ko SB, Vaccaro AR, Chang HJ et al (2015) An evaluation of the effectiveness of hyaluronidase in the selective nerve root block of radiculopathy: a double blind, controlled clinical trial. Asian Spine J 9(1):83–89. doi:10.4184/asj.2015.9.1.83
Yeom JS, Lee JW, Park KW et al (2008) Value of diagnostic lumbar selective nerve root block: a prospective controlled study. AJNR Am J Neuroradiol 29(5):1017–1023. doi:10.3174/ajnr.A0955
Gu G, Zhang H, Fan G et al (2014) Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop 38(4):817–824. doi:10.1007/s00264-013-2169-x
Wang K, Hong X, Zhou BY et al (2015) Evaluation of transforaminal endoscopic lumbar discectomy in the treatment of lumbar disc herniation. Int Orthop. doi:10.1007/s00264-015-2747-1
Jacquot F, Gastambide D (2013) Percutaneous endoscopic transforaminal lumbar interbody fusion: is it worth it? Int Orthop 37(8):1507–1510. doi:10.1007/s00264-013-1905-6
Chen Z, Zhao J, Liu A et al (2009) Surgical treatment of recurrent lumbar disc herniation by transforaminal lumbar interbody fusion. Int Orthop 33(1):197–201. doi:10.1007/s00264-008-0531-1
Hanzhang Z (2006) Acupotomolgical theory: formation and perfection. World Sci Technol Modern Trad Chin Med Mater Med 8(4):85–93. doi:10.3969/j.issn.1674-3849.2006.04.021
Hanzhang Z (2006) Summarization of acupotomology system. Eng Sci 8(7):1–15. doi:10.3969/j.issn.1009-1742.2006.07.001
Jinping M, Li L, Wei F et al (2010) Systematic review of needle-knife therapy for lumbar intervertebral disc protrusion. Chin J Inf TCM (07):31-35
Kambin P, O’Brien E, Zhou L et al (1998) Arthroscopic microdiscectomy and selective fragmentectomy. Clin Orthop Relat Res 347:150–167
Park JW, Nam HS, Cho SK et al (2011) Kambin’s triangle approach of lumbar transforaminal epidural injection with spinal stenosis. Ann Rehabil Med 35(6):833–843. doi:10.5535/arm.2011.35.6.833
Kambin P, Sampson S (1986) Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs: report of interim results. Clin Orthop Relat Res 207:37–43
Dalbayrak S, Yaman O, Yilmaz M et al (2015) Transforaminal approach in lumbar disc herniations: transforaminal microdiscectomy (TFMD) technique. Turk Neurosurg 25(1):29–35. doi:10.5137/1019-5149.JTN.8197-13.1
Cramer GD, Skogsbergh DR, Bakkum BW et al (2002) Evaluation of transforaminal ligaments by magnetic resonance imaging. J Manip Physiol Ther 25(4):199–208
Park HK, Rudrappa S, Dujovny M et al (2001) Intervertebral foraminal ligaments of the lumbar spine: anatomy and biomechanics. Childs Nerv Syst 17(4-5):275–282
Amonoo-Kuofi HS, El-Badawi MG, Fatani JA et al (1988) Ligaments associated with lumbar intervertebral foramina. 2. The fifth lumbar level. J Anat 159:1
Transfeldt EE, Robertson D, Bradford DS (1993) Ligaments of the lumbosacral spine and their role in possible extraforaminal spinal nerve entrapment and tethering. J Spinal Disord Tech 6(6):507–512
Golub BS, Silverman B (1969) Transforaminal ligaments of the lumbar spine. J Bone Joint Surg 51(5):947–956
Uei H, Tokuhashi Y, Oshima M et al (2014) Vascular injury following microendoscopic lumbar discectomy treated with stent graft placement: case report. J Neurosurg Spine 20(1):67–70
Uribe JS, Deukmedjian AR (2015) Visceral, vascular, and wound complications following over 13,000 lateral interbody fusions: a survey study and literature review. Eur Spine J 1-11
Wang K, Hong X, Zhou BY et al (2015) Evaluation of transforaminal endoscopic lumbar discectomy in the treatment of lumbar disc herniation. Int Orthop. doi:10.1007/s00264-015-2747-1
Horvath G, Koroknai G, Acs B et al (2010) Prevalence of low back pain and lumbar spine degenerative disorders. Questionnaire survey and clinical-radiological analysis of a representative Hungarian population. Int Orthop 34(8):1245–1249. doi:10.1007/s00264-009-0920-0
Halldin K, Lind B, Ronnberg K et al (2009) Three-dimensional radiological classification of lumbar disc herniation in relation to surgical outcome. Int Orthop 33(3):725–730. doi:10.1007/s00264-008-0519-x
Min J, Kang S, Lee J et al (2005) Anatomic analysis of the transforaminal ligament in the lumbar intervertebral foramen. Neurosurgery 57(1):37–41
Zhengin L, Eryu C (1989) The clinical anatomy series: chest and spinal anthology. People’s Medical Publishing House of China 287–298
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuan, Sg., Wen, Yl., Zhang, P. et al. Ligament, nerve, and blood vessel anatomy of the lateral zone of the lumbar intervertebral foramina. International Orthopaedics (SICOT) 39, 2135–2141 (2015). https://doi.org/10.1007/s00264-015-2831-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2831-6