Abstract
Purpose
Treatment of tibial plateau fractures is discussed. A retrospective comparative study of fractures treated with an anatomical locking plate of 4.5 mm or 3.5 mm. Our hypothesis is that the 3.5 mm plates give an equivalent hold of fractures with comparable results and better clinical tolerance.
Methods
From May 2010 to October 2011, 18 patients were operated on using a 4.5-mm LCP™ anatomical plate (group A) and 20 patients received a3.5-mm LCP™ anatomical plate (group B). Groups were comparable. One fracture was open.
Results
For the Group A, 14 patients had a follow up of 35.3 months and for the Group B, 16 patients had a follow up of 27 months. Mobility was comparable in both groups. The Hospital for Special Surgery (HSS) score was 86.4 versus 80.6, the Lysholm score was 83.6 versus 77 for groups A and B respectively. Consolidation was 3.25 months versus 3.35 months and mean axis was 183.1° versus 181.6° for groups A and B. Mechanical axes during revision were statistically different to the controlateral axes. One secondary displacement was noted in group A and one secondary displacement in group B. Group A had eight patients reporting discomfort with the material versus three in group B (p < 0.05).
Conclusion
The hypothesis is proven. In regards to the results, there is no significant difference between the two groups but the clinical tolerance was better in group B. More time is needed in the long term to better evaluate these severe fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibial plateau fractures are rare, with a frequency of 1.2 % [1]. There is no consensus in the surgical management of simple fractures, whereas the “gold standard” treatment for complex fractures is plate osteosynthesis [2–10]. Nonetheless, there is no consensus on the type of assembling to be carried out for complex fractures: medial plate, double plate, standard or locking plate, 4.5-mm plates or 3.5-mm plates. Some authors recommend the use of a medial plate once the medial tibial plateau is affected [2–4], guaranteeing better axial resistance. Yoo et al. [5] and Jiang et al. [6] demonstrated that a standard double plate had a better mechanical resistance to that obtained by an unique locking plate, while Mueller et al. [7], Gosling et al. [8, 9] and Higgins et al. [10] proved experimentally and clinically the reliability of a unique lateral locking plate.
Pre-shaped plates theoretically facilitate reduction and improve clinical tolerance, but 4.5 mm plates are often voluminous and cumbersome. Recently Hasan et al. [11] compared the mechanical properties of 3.5-mm and 4.5-mm locking plates with a bicondylar tibial plateau model. No difference was noticed in cyclic loading or for elastic and plastic deformation, nevertheless, 4.5-mm plates are significantly more resistant in terms of axial loading but only for Schatzker V fractures [12]. The authors concluded in favour of 3.5-mm plates due to their comparable mechanical resistance and their clinical lower-profile. To our knowledge, no study has compared the results of tibial plateau fracture synthesis using a 3.5-mm locking pre-shaped anatomical plate or a 4.5-mm locking pre-shaped anatomical plate. The objective of this study was to demonstrate the radio-clinical results in the medium term of these two therapeutic modalities by specifically analyzing the solidness of the assembly and the clinical tolerance. Our hypothesis was based on data from literature that radioclinical results were comparable between 3.5-mm and 4.5-mm plates concerning post-reduction stability with time, but a better clinical tolerance for 3.5-mm plates.
Materials and methods
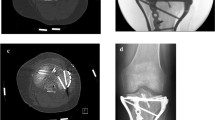
Fractures in this continuous retrospective series (from May 2010 to October 2011) were of traumatic cause. Fractures of open growth plates and pathologic fractures were excluded. Thirty-eight patients were included and distributed in two groups: group A (4.5-mm plates) (Fig. 1) and group B (3.5-mm plates) (Fig. 2). Both groups were comparable in terms of number of cases, age, sex and type of Schatzker fracture [12]. Both groups were consecutive. There were more road accidents in group B (13 versus 5). Fifteen patients were retired (group A = 6, group B = 9) and 23 were still in active service (group A = 12, group B = 11). None of the fractures presented initially with vasculo-neurological complications and one fracture in group A was open stage II according to Gustilo [13] (Table 1).
Surgical procedure
Surgical delay was comparable in the two groups. In all cases, the surgeon was a senior physician, there were five different surgeons. The patients were always made to lie in the supine position on a standard table with a tourniquet in almost every case (group A = 18/18, group B = 19/20). When a lateral plate was placed, the surgical approach was a classic lateral one with submeniscal athrotomy, and when a medial plate was placed, the surgical approach was a medial retro-ligamentary. The choice of the surgical approach and the kind of surgery was left to the preference of the operator on the basis of a systematic pre-operative CT scan. The plates used were anatomical locking plates LCP® (Depuy-Synthes, Etupes, France). For the 3.5-mm plates there was a lateral (ref. 02.124.20/21) or a medial (ref. 239.95/96) anatomic model, and for 4.5-mm plates (ref. 222.22) there was only a lateral anatomic one. Plates were always in titanium. In comparison with standard stainless plates, we choose anatomical locking plates because the screws had a better bony fixation, independent of bone quality, and because titanium gives elasticity to the assemblage that benefits consolidation. The choice of the plate (3.5 or 4.5 mm) was according to the surgeon’s preference and independent of the type of fracture. In group A, the plates were always unique: 16 times in lateral and twice in medial. In group B, a unique lateral plate was used ten times, a unique medial plate four times and a double plate six times. In order to overcome the impossibility of compression by the locking screws, an additional initial screwing was done 14 times (seven times in each group). A graft was used 12 times (group A = six times with a bone substitute) (group B = 6: three times with a substitute and three times with a lyophilized bone). The average operating time was comparable for each group, 89.5 minutes in group A and 107 minutes in group B. A minimal postsurgical non-weight-bearing period of six weeks and immediate mobilization on an athromotor in a sector of 0–90° were prescribed in the immediate follow-up. Free mobilisation was allowed beyond six weeks. Total weight-bearing permission depended on radiologic imaging. It was 8.6 weeks (six to 16, med eight) in group A, and nine weeks (eight to 12, med eight) in group B (Table 2).
Evaluation
Evaluation was retrospective. We compared the immediate postoperative X-rays with those obtained at the consolidation time. An initial articular reduction default was considered as pathologic if it was greater than 2 mm [2–10]. Consolidation was considered as achieved when the whole fracture line had disappeared anteroposteriorly and laterally. Follow-up study was completed with a pangonometry. Deficiency in axis was considered as pathologic when pangonometry showed a global deformation superior to 5° compared to 180°. Signs of osteoarthritis were looked for over a long period of time. On review, clinical evaluation included a measure of mobility and functional evaluation using scores like Lysholm [15] and Hospital for Special Surgery (HSS) [16]. Patients were asked a satisfaction index ranging from (very good, good, worse). Observed complications were compiled.
Statistical analysis
For statistical results, a Student t-test was used with a positivity threshold of p < 0.05 to compare for continuous variables (quantitative variables). A chi-squared test was used for categorical variables between the two groups with a positivity threshold of p < 0.05.
Results
At the follow-up, one patient was lost in each group before estimating consolidation. In group A, 14 patients were reviewed (22 % were lost to follow-up) at a mean of 35.3 months (26–43, med 24), and 16 were reviewed in group B (20 % were lost to follow-up) at a mean of 27 months (19.5–38, med 27.5). The bigger mean of group A was due to the recent use of 3.5-mm plates in our usual practice.
Clinical results were presented in Table 3. Concerning group A, seven patients returned to the same level of their usual activity in an average time of four months (3–8) and two underwent professional rehabilitation. In group B, five returned to their same level of activity in an average time of 3.8 months (three to six) and three underwent rehabilitation. The remaining patients of the two groups were retired. No statistical difference was observed.
Radiologic results were presented in Table 4. In group A, a case of nonunion was reoperated at 5.5 months using an autologous decortications graft with a favorable outcome at three months post graft. During review, mechanical axis of lower limb in group A was 183.1° on average, for a contralateral mechanical axis of 179.5° (p < 0.02). Four axial valgus deformity were greater than 5° (6°, 6.8°, and 14°) were observed. Four times more major modification of mechanical axis (>5°) were observed compared to the healthy side (8°, 8°, 9°, 11°), without evolving into osteoarthritis. During review, mechanical axis of lower limb in group B was 181.6° on average for a contralateral mechanical axis of 178° (p < 0.002), with an additional case of more than 5° valgus at 12°. Three times more major modification of mechanical axis (>5°) were observed compared with the healthy side with a difference of 10°, 12° and 12° respectively. Once, this led to an early case of osteoarthritis and twice the clinical results were disappointing with a HSS score of 58 and 45 respectively and a Lysholm score of 50 and 47 respectively. No statistical difference was noted between the two groups.
Several complications were noted. In group A, four complications were observed in three patients: one deep venous thrombosis, one spontaneous resolving algodystrophy, one immediate postoperative compartment syndrome requiring emergent fasciotomy with a favorable outcome in the end, and a spontaneous and complete regression of paraesthesia involving the common fibular nerve. In group B, three complications were observed in three patients: one algodystrophy, one non-infectious dissension of scar tissue was treated locally with a satisfactory evolution and one Enterobacter cloacae arthritis developed on the 7th postoperative day and was treated in another establishment with no further information on its outcome.
Discomfort of osteosynthesis material was significantly (p < 0.05) more common in group A (n = 8/14, 57 %) with four hardware removals (28.6 %) on average at 19.5 months without any complication. In group B, material discomfort was observed three times (3/16, 18.7 %), leading to two removals (12.5 %). A third one was carried out in view of a programmed prosthetic knee replacement without any clinically reported discomfort.
Discussion
The most important finding of the present study was the comparable radio-clinical results between 3.5-mm and 4.5-mm locking pre-shaped anatomical plates and the better clinical tolerance of 3.5-mm plates.
Range of motion recuperation and functional recuperation were similar, responding more to the severity of the lesions rather than the type of material used. Radiologic results were equally comparable in terms of rate and time of consolidation but also of quality of articular reduction, which highlights the stability of the reduction for the two types of implants, thus confirming biomechanical data [11].
Our hypothesis was confirmed. Thus we are convinced of the benefits of the use of a 3.5-mm locking pre-shaped plate on functional recovery and stability of fracture.
There is no consensus in the literature concerning the strategy for surgical management of proximal tibial fractures: one or two plates? Standard or locking? Experimental data in literature are divergent. Based on an experimental point of view for medial fractures, the plate has to be medial with a console effect [2–4]. For more complex fractures, Yoo et al. [5] recommended the use of a double plate. They compared experimentally on synthetic bones: 3.5-mm lateral plates, medial double-plate LC-DCP, double plate with a third medial tube plate and a lateral LC-DCP, a lateral locking plate and a LISS plate. They concluded on the superiority of the association between 3.5-mm lateral plate and the 3.5-mm medial third tube plate when the assembly was exposed to axial stress. Jiang et al. [6] showed similar experimental results. Nonetheless, in other biomechanical studies, no difference was observed in resistance during compression when a unique lateral locking plate was used comparatively to an assembly with two plates [7, 8, 10].
Recent experimental studies have shown precisely the utilization of locking plates in these indications. For Estes et al. [19], there is no difference axially between the assembly “fully locked” and the “mixed type of assembly”. For Cullen et al. [20], the use of poly-axial locking screws offered better rigidity and better resistance to rupture. Finally, Lindeque and Baldini [21] compared different locking systems, and concluded that the Synthes® and DePuy® systems had better resistance to wear in contrast to the Zimmer® system, but that the DePuy® system had a resistance to rupture better than the other two. Our radiologic results confirm these experimental data, even though a secondary displacement occurred in each group. Fracture stability was achieved irrespective of the type of plate, thus validating our hypothesis. Analysis of mechanical axes of lower limbs during review revealed metaphyseal abnormality, evaluation of the articular area was judged to be good. There is no particular type of fracture at risk with three type II, one type III, two type V and one type VI. The most important point during review was the significant difference in mechanical axis between the fractured side and the contralateral side for both implants, highlighting a lack of attention to detail during the restitution of the mechanical axis. The anatomic characteristics of the plates should reduce this risk, provided that they are used as a reduction mold with articular epiphyseal screw parallelism associated with cortical tibial plate parallelism.
Concerning radiologic and clinical results, Barei et al. [22] concluded that conventional osteosynthesis with two plates was a sure technique with satisfying results with no more complications. However, the use of two plates can expose difficulties when implanting a total knee arthroplasty, with the obligation to remove the plates through two incisions and a longer surgery time. Some authors proposed a multi-plate reconstruction for severe bicondylar tibial plateau fracture, especially for young adults, with three to five plates [23]. In order to reduce cutaneous and septic complications a double mini-invasive surgical access was proposed. Oh et al. [24] reported 21 excellent clinical results out of 23 cases but 9.35 % of global malunion. These authors insisted on the absence of iatrogenia in this mini-invasive surgical technique. We do not have any experience in mini-invasive surgery for articular fractures, of which we remain convinced in the interest of direct control reduction. Despite this precaution, we observed defects in the mechanical axis during review, even though the articular area remained unaffected. To our knowledge only one clinical study (84 cases) compared standard double-plate osteosynthesis to lateral locking plate [18]. The results are statistically comparable in terms of reduction loss, material rupture, rate of infection, rate of consolidation and HSS functional score. Radiologic results were not in favor of the LISS locking system with an explanation for statistical difference for defects being due to the mini-invasive characteristics of the surgery. According to our experience, one lateral 4.5-mm locking plate is useful and gives very good radiological and clinical results, especially if there is a medial tibial plateau component [25]. In this series, the choice of plate was not done according to fracture type but to the surgeon’s philosophy, and in case of two plates it was easier with 3.5-mm rather 4.5-mm plates. But we think that using locking plates changes our point of view about single or double plates. Publications showed satisfying radio-clinical results for the treatment of articular proximal tibial using locking plates [14, 17, 26–30], but to our knowledge none show comparative results for 3.5-mm plates. The rate of malunion ranged from 0 to 23 % and the rate of correction loss from 0 to 14 %. In our series, the observed rates were comparable. Clinical results seen in the literature are comparable to ours, emphasizing the severity of these lesions and the absolute necessity of a quality reduction [31, 32]. Mobility and functional scores that we reported were satisfying and identical irrespective of the type of plate. Thus, according to our experience, in the short term there were few repercussions on the existence of malunions.
To our knowledge, the clinical tolerance of locking plates was rarely studied, even though this was discusses by Hasan et al. [11]. The different studies showed at the most the number of material ablations, with different figures ranging from 5 to 11 % [14, 17, 25–36]. Concerning clinical tolerance, our hypothesis was confirmed with a better clinical tolerance for 3.5-mm plates, which has never been discussed in the literature.
Given the articular characteristics of these fractures, we do not recommend nailing in these cases. To our knowledge, there are no studies that compare nailing to locking plates for articular fractures of the tibial plateau. In a radiological and technical comparative study of centro-medullary nailing versus 4.5-mm locking anatomic plates in the treatment of proximal tibial extra-articular fractures, Lindvall et al. [37] demonstrated a higher rate of clinical intolerance for plates with three times more implant removal. The results of this series underline the difficulty in treating proximal tibial fractures with nailing with more malreduction. Indeed, apex anterior malreduction deformity occurred twice in the nailing group and additional surgical techniques were frequently used during reduction within the nailing group.
This study has several limitations. It was a retrospective study. The series was heterogeneous, with different surgeons and a non-standardized surgical procedure. The number of cases is low, but the two groups were comparable and it was a rare fracture. Follow-up time was limited to evaluate osteoarthritis evolution and there was a lot of cases lost to follow-up; but there were some young people in this series who left their first address. Nevertheless, this study allows confirmation of the hypothesis.
Conclusion
The objective of this study was to compare the radio-clinical results, in the medium term, of tibial plateau fractures treated by 3.5-mm or 4.5-mm locking plates, to analyze the solidness of the assembly and the clinical tolerance. Our hypothesis was that radio-clinical results were comparable between the two types of plates concerning post reduction stability with time, but with a better clinical tolerance for 3.5-mm plates. Our hypothesis was confirmed. In conclusion, we can recommend the use of 3.5-locking plates for all tibial plateau fractures. One or two plates were discussed case by case and according the surgeon’s philosophy.
References
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697
Wu CC, Tai CL (2007) Plating treatment for tibial plateau fractures: a biomechanical comparison of buttress and tension band positions. Arch Orthop Trauma Surg 127:19–24
Ratcliff JR, Werner FW, Green JK, Karley BJ (2007) Medial buttress versus lateral locked plating in a cadaver medial tibial plateau fracture model. J Orthop Trauma 21:444–448
Zeng ZM, Luo CF, Putnis S, Zeng BF (2011) Biomechanical analysis of posteromedial tibial plateau split fracture fixation. Knee 18:51–54
Yoo BJ, Beingessner DM, Barei DP (2010) Stabilization of the posteromedial fragment in bicondylar tibial plateau fractures: a mechanical comparison of locking and nonlocking single and dual plating methods. J Trauma 69:148–155
Jiang R, Luo CF, Zeng BF (2008) Biomechanical evaluation of different fixation methods for fracture dislocation involving the proximal tibia. Clin Biomech 23:1059–1064
Mueller KL, Karunakar MA, Frankenburg EP, Scott DS (2003) Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop 412:189–195
Gosling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C (2004) Less invasive stabilization of complexe tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma 18:546–551
Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C (2005) Single lateral locked screw plating of bicondylar tibial plateau. Clin Orthop 439:207–214
Higgins TF, Klatt J, Bachus KN (2007) Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma 21:301–306
Hasan S, Avalon OB, Yoon RS, Sood A, Militano U, Cavanaugh M, Liporace FA (2014) A biomechanical comparison between locked 3.5mm plates and 4.5mm plates for the treatment of simple bicondylar tibial plateau fractures: is bigger necessarily better? J Orthop Trauma 15:123–129
Schaztker J (1974) Compression in the surgical treatment of fractures of the tibia. Clin Orthop 105:220–229
Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 58:453–458
Biggi F, DiFabio S, D’Antimo C, Trevisani S (2010) Tibial plateau fractures: internal fixation with locking plates and the MIPO techniques. Injury 41:1178–1182
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligaments injuries. Clin Orthop 198:43–49
Ranawat CS, Shine J (1973) Duo condylar total knee arthroplasty. Clin Orthop 94:185–195
Schutz M, Kaab MJ, Haas N (2003) Stabilization of proximal tibia fractures with the LIS-System: early clinical experience in Berlin. Injury 34(suppl 1):A30–A35
Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF (2008) A comparative study of Less Invasive Stabilization System (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. Knee 15:139–143
Estes C, Rhee P, Shrader MW, Csavina K, Jacofsky MC, Jacofsky DJ (2008) Biomechanical strength of the peri-loc proximal tibial plate: a comparison of all-locked versus hybrid locked/nonlocked screw configurations. J Orthop Trauma 22:312–316
Cullen AB, Curtiss S, Lee MA (2009) Biomechanical comparison of polyaxial and uniaxial locking plate fixation in a proximal tibial gap model. J Orthop Trauma 23:507–513
Lindeque B, Baldini T (2010) A biomechanical comparison of three different lateral tibia locking plate. Orthopedics 33:18–21
Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK (2006) Functionnal outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am 88:1713–1721
Zhai Q, Hu C, Luo C (2014) Multi-plate reconstruction for severe bicondylar tibial plateau fractures of young adults. Int Orthop 38:1031–1035
Oh CH, Oh JK, Kyung HS, Jeon IH, Park BC, Min WK, Kim PT (2006) Double plating of unstable proximal tibial fractures using minimally invasive percutaneous osteosynthesis technique. Acta Orthop 77:524–530
Ehlinger M, Rahme M, Moor BK, Di Marco A, Brinkert D, Adam P, Bonnomet F (2012) Reliability of locked plating in tibial plateau fractures with a medial component. Orthop Traumatol Surg Res 98:173–179
Beck M, Gradl G, Gierer P, Rotter R, Witt M, Mittelmeier T (2008) Treatment of complicated proximal segmental tibia fractures with the less invasive stabilization locking plate system. Unfallchirurg 111:493–498
Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ (2004) Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma 57:340–346
Haiduewych G, Sems SA, Huebner D, Horwitz D, Levy B (2008) Results of polyaxial locked-plate fixation of periarticular fractures of the knee. Surgical technique. J Bone Joint Surg Am 90(Suppl 2):117–134
Stannard JP, Wilson TC, Volgas DA, Allonso JE (2003) Fracture stabilization of proximal tibial fractures with the proximal tibial LISS: early experience in Birmingham, Alabama (USA). Injury 34(Suppl 1):A36–A42
Lee JA, Papadakis SA, Moon C, Zalavras CG (2007) Tibial plateau fractures treated with the less invasive stabilization system. Int Orthop 31:415–418
Mattiassich G, Foltin E, Scheurecker G, Schneiderbaueur A, Kropfl A, Fischmeister M (2014) Radiographic and clinical results after surgically treated tibial plateau fractures at three and twenty two years postsurgery. Int Orthop 38:587–594
Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P (2010) Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop 34:565–570
Boldin C, Finkhauser F, Hofer HP, Szyzkowitz R (2006) Three year results of proximal tibia fractures treated with LISS. Clin Orthop 445:222–229
Cole PA, Zlowodzki M, Kregor PJ (2004) Treatment of proximal tibia fractures using the less invasive stabilization system. Surgical experience and early clinical results in 77 fractures. J Orthop Trauma 18:528–535
Phisitkul P, McKinley TO, Nepola JV, Marsh JL (2007) Complications of locking plate fixation in complex proximal tibial injuries. J Orthop Trauma 21:83–91
Ricci WM, Rudzki JR, Borelli J (2004) Treatment of complexe proximal tibia fractures with the less invasive skeletal sabilization system. J Orthop Trauma 18:521–527
Lindvall E, Sanders R, DiPasquale T, Herscovici D, Haidukewych G, Sagi C (2009) Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma 23:485–492
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ehlinger, M., Adamczewski, B., Rahmé, M. et al. Comparison of the pre-shaped anatomical locking plate of 3.5 mm versus 4.5 mm for the treatment of tibial plateau fractures. International Orthopaedics (SICOT) 39, 2465–2471 (2015). https://doi.org/10.1007/s00264-015-2713-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2713-y