Abstract
Purpose
This study compares the radiographic and functional outcomes of uncemented and cemented humeral fixation in reverse total shoulder arthroplasty (RTSA).
Methods
A prospective research database was reviewed for RTSA patients from 2007 to 2010. Inclusion criteria were primary RTSA from one manufacturer (Exactech Equinoxe®) with a grit-blasted metaphyseal humeral stem and two year minimum follow-up. Exclusion criteria included shoulder arthroplasty for fractures, fracture sequelae or inflammatory arthropathy. Radiographic and functional outcomes were compared between the uncemented and cemented groups.
Results
A total of 97 patients (58 women, 39 men) with 100 RTSAs met the inclusion criteria. Radiographic and clinical two year follow-up was available in 80 % (51 RTSAs) of the uncemented group and 89 % (32 RTSAs) of the cemented group (mean follow-up 3.5 years). Average age at surgery was 72 years. Both groups showed significant improvements in the 12-item Simple Shoulder Test (SST-12), 12-item Short Form (SF-12), Shoulder Pain and Disability Index 130 (SPADI-130), American Society of Shoulder and Elbow Surgeons (ASES) score and normalised Constant scores. One humeral loosening was seen in each group (2 % uncemented, 3 % cemented). Both groups’ overall component revision rate was 6 % (one in each group relating to humeral component failure). There were no significant differences in complication rates, change in functional scores and range of motion improvement.
Conclusions
Humeral component press-fitting in RTSA provides similar outcomes as cementation at a minimum two year follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Reverse total shoulder arthroplasty (RTSA) is used to treat rotator cuff arthropathy, glenohumeral arthritis with rotator cuff deficiency, massive rotator cuff tears with pseudoparalysis, symptomatic irreparable rotator cuff tears, inflammatory arthritis, complex proximal humerus fractures in the elderly and the sequelae of proximal humeral fractures [1]. Since its 2003 US Food and Drug Administration (FDA) approval, its use has been increasing in the USA. While many designs exist, the overall principle is similar. The deltoid acts as the lever arm, allowing shoulder flexion and providing glenohumeral stability through compression.
Functional outcomes of RTSA have been promising, but long-term studies with greater than ten year follow-up are lacking [1, 2]. Although glenoid fixation without cement has generally proven viable in RTSA, no study has specifically focused on uncemented humeral fixation. Several studies have included uncemented humeral components in the study population [3–10], but none were designed to directly compare the functional and radiographic outcomes of cemented and uncemented humeral fixation.
Studies on uncemented humeral fixation in total shoulder arthroplasty have shown high rates of lucencies as well as a high percentage of stems that are at risk for loosening [11, 12]. One randomised controlled trial of uncemented and cemented stems in total shoulder arthroplasty showed better functional scores and forward elevation with cemented stems [13]. The different biomechanics of the reverse shoulder replacement may alter the load on the humeral stems compared to total shoulder arthroplasty. The effect on clinical outcomes of this different loading of the proximal humerus is unknown in RTSA. The theoretical advantages of uncemented humeral fixation are decreased operative time, biological ingrowth potential and easier revision of the humeral component if necessary.
The purpose of this study is to compare the functional and radiographic outcomes of cemented and uncemented humeral components in RTSA. We hypothesise that patients with press-fit humeral components have the same functional outcomes, similar complication rates and similar loosening rates compared to patients with cemented humeral components in RTSA.
Patients and methods
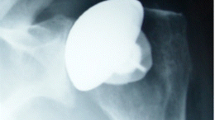
A review of a consecutive series of patients treated with a primary RTSA for cuff tear arthropathy at the University of Florida between June 2007 and December 2010 was performed. Medical records and a prospective research database were reviewed for demographic, operative and clinical information. Inclusion criteria were primary RTSA with the Exactech Equinoxe® system (Gainesville, FL, USA) using a metaphyseal grit-blasted humeral stem (Fig. 1) and a minimum follow-up of two years. Exclusion criteria included shoulder arthroplasty for fractures or fracture sequelae, chronic shoulder dislocations, inflammatory arthropathy or a prior arthroplasty procedure.
The standard deltopectoral approach was used in all cases. The glenoid baseplate was placed with the inferior edge of the baseplate lining up with the inferior aspect of the glenoid. The baseplate uses a cage for bone ingrowth. Humeral head autograft was routinely used in the cage to aid in bone ingrowth. At least four baseplate compression screws were placed with the goal of three screws with good fixation. Each compression screw was converted to a locking screw using locking caps.
The proximal humeral shaft was lightly hand-reamed and sequentially broached with the goal of 20° of stem retroversion. For the cemented cases, a cement restrictor and antibiotic-impregnated cement were routinely used. The subscapularis tendon was not routinely repaired unless there was excellent compliance of the tendon. Concerns for a tight subscapularis repair were that the surgeon could create an iatrogenic Hornblower’s sign. Biceps tenodesis was routinely performed to the pectoralis major insertion. Drains were not used.
The decision for cementation versus press-fitting of the humeral component was determined by the surgeon depending on preference, bone quality and available bone stock. The surgeons tended to use cemented humeral fixation early in the study period and changed to predominantly press-fit humeral fixation by the end of the study period.
The rehabilitation protocol was the same for all patients and consisted of a home-based physical therapy programme. Active range of motion was limited for three weeks and external rotation was limited to neutral for weeks weeks. Sling use was discontinued at six weeks and weight restriction limitation was discontinued at three months.
The functional outcomes were compared between the uncemented and cemented humeral stem groups. Range of motion measurements were obtained preoperatively and postoperatively by a research assistant (certified athletic trainer) using a goniometer and placed in a prospective database at annual postoperative visits. Functional scores used were the 12-item Short Form (SF-12), the American Society of Shoulder and Elbow Surgeons (ASES) score, the normalised Constant score, the 12-item Simple Shoulder Test (SST-12) score and the Shoulder Pain and Disability Index 130 (SPADI-130) score and were recorded in a prospective research database. Any missing range of motion data or functional scores were omitted from the individual calculations.
The radiographic outcomes were compared between the uncemented and cemented groups using Grashey and axillary lateral radiographs (Fig. 2a, b). Humeral lucencies were measured using the technique described by Sanchez-Sotelo et al. [12] where eight zones were identified around the proximal humerus. Humeral loosening was defined as progressive radiolucent lines in greater than two zones or with lucent zones and increasing pain with activity. The number of patients with lucent zones was based on their most recent follow-up imaging. Notching was defined on a 0–4 grading scale, as described by Sirveaux et al. [10]. Glenoid loosening was defined as progressive radiolucent lines >2 mm around more than one screw or a shift in baseplate position.
Statistical analysis was performed using Fisher’s exact test to compare dichotomous variables like the complication rates between groups. Functional outcome data between the groups were calculated using the two-tailed Wilcoxon rank sum test. Multivariate analysis was not performed due to the limited number of patients in each group. Post hoc power analysis was performed to see if the numbers had 80 % power to detect a 15 % difference in the change in functional outcome scores and range of motion between the cemented and uncemented groups. Post hoc power analysis showed that this study had enough patients in each group to detect a 15 % difference of the change in SPADI-130 (30 patients) and SF-12 scores (30 patients). This study did not have enough patients in each group to detect a 15 % difference of the change in the normalised Constant score (99 patients), SST-12 (412 patients), ASES score (148 patients), forward elevation (141 patients) or external rotation (798 patients).
Results
A total of 97 patients (58 women, 39 men) with 100 RTSAs met the inclusion criteria from a total of 183 RTSAs performed in the study period. Reasons for exclusion were 34 revisions, 23 with a different implant, 18 fractures or fracture sequelae and eight with inflammatory arthropathy. Of the patients, 64 had an uncemented humeral component and 36 had a cemented humeral stem. Figure 3 shows the trend of humeral fixation over the study time period. The two year follow-up was available for 51 patients with uncemented humeral components (follow-up rate of 80 %) and for 32 patients with cemented humeral components (follow-up rate of 89 %). Eight patients had died (all unrelated to their shoulder surgery) with the prosthesis in place, eight were lost to follow-up before their two year follow-up appointment and one refused participation due to health reasons. These patients were excluded from further analysis. The flow chart of patient selection is presented in Fig. 4. Average follow-up was 3.5 years (3.3 years for the uncemented group and 4.0 years for the cemented group).
The final group included 83 RTSAs in 80 patients including 48 women and 32 men. There were 49 right shoulders and 34 left shoulders. The most common diagnosis was rotator cuff arthropathy in 69 shoulders (83 %). Twelve patients had glenohumeral osteoarthritis with rotator cuff insufficiency, one had avascular necrosis with a torn rotator cuff and one had arthritis from pigmented villonodular synovitis with an insufficient rotator cuff. Average age at surgery was 72 years (range 55–93 years). Forty per cent of the patients had a prior non-arthroplasty surgical procedure on the operative shoulder. More complete demographic data are available in Table 1.
A total of 17 patients were not included in this study, as mentioned previously (four patients in the cemented group and 13 in the uncemented group). No known postoperative complications, humeral loosening or revisions were reported for this group. Average follow-up for this group was nine months with nine patients having at least one year of follow-up. Fourteen of these patients had some functional data prior to loss to follow-up or death. Average active forward elevation was 106°. Average active external rotation was 21°. Average internal rotation was to L3. The average ASES score was 68. Average SPADI-130 was 43.5. Average SST-12 score was 7.6. Average normalised Constant score and SF-12 score were 58.7 and 35.3.
Range of motion significantly increased in active forward elevation and active abduction to 117 and 110° with an average improvement of 41° in both (Table 2). Active external rotation improved an average of 2° to 25°. Internal rotation improved an average of two spinal levels to L2. Both uncemented and cemented groups saw significant increases in forward elevation and abduction, whereas the change in external rotation was not significant in either group (Table 2). Significant improvement in internal rotation was obtained in the uncemented group, but not in the cemented group. Both uncemented and cemented groups had similar improvements in range of motion with no significant difference between groups (Table 2).
Functional outcomes improved significantly in both the cemented and uncemented groups (Table 3). The most dramatic improvement was seen in the SST-12 score with a 6.3 point average increase. In addition, the normalised Constant score increased an average of 41 points, the SPADI-130 score improved an average of 56 points and the ASES score increased an average of 44 points. The improvement in functional scores was not significantly different between groups (all P values >0.05).
Radiographic outcomes were similar between groups (Table 4). Humeral loosening was seen in one patient in each group (2 % rate in the uncemented group and 3 % in the cemented group). Two patients (4 %) had some radiolucent lines in the uncemented group including the one that had a loose stem (Fig. 5a). The patient without loosening had humeral radiolucencies in zones 1 and 7. No patients had additional radiolucent lines in the cemented group except for the one patient with gross loosening (Fig. 5b). Scapular notching was seen in seven patients in the uncemented group (14 %) and all had grade 1 notching. Two patients (6 %) in the cemented group had scapular notching (all grade 1). Only one patient had glenoid loosening (the same patient in the uncemented group that had humeral loosening). These radiographic outcomes were not statistically different between the groups.
Grashey view (a) of a patient with an uncemented humeral stem with subtle lucent lines (blue arrows) and metaphyseal lucency (white arrow), which had definite loosening noted at the time of revision surgery. Grashey view (b) of a patient with a cemented humeral stem with significant lucent lines (arrows)
The most common complication was periprosthetic humeral shaft fracture after falls (six patients, 7 %). This was more common in the uncemented group, but the difference was not significant. Three patients in the uncemented group (6 %) and one in the cemented group (3 %) needed surgical fixation of the periprosthetic humeral fractures. One patient had a dislocation in the cemented group (total dislocation rate of 1 %). Humeral stem revision was performed in two patients in the uncemented group (one for infection and one for loosening) and in two patients in the cemented group (one for humeral loosening and one for an infection after a second procedure for a primary dislocation). Revision of any component was performed in three patients in the uncemented group (6 %) and in two patients in the cemented group (6 %). More complication data are available in Table 5.
Discussion
Based on the data presented, the functional and radiographic outcomes after primary RTSA are similar for cemented and uncemented grit-blasted metaphyseal humeral stems (Exactech Equinoxe® shoulder system) at a minimum follow-up of two years. This is the first study to directly compare the outcomes of uncemented and cemented humeral stems in primary RTSA to our knowledge in the English literature.
The range of motion after RTSA seen in this study is very similar to previous reports. Active forward elevation (117 versus 100–150°) [5, 7, 9, 10, 14–26], active abduction (110 versus 90–133°) [5, 9, 15–18, 22, 24, 25], active external rotation (25 versus 7–51°) [5, 7, 9, 10, 14–18, 20–23, 26] and internal rotation (L3 versus S1-L1) [10, 14, 20–22, 24, 26] were within the ranges reported in the literature. Melis et al. [7] also reported similar range of motion data in combined primary and revision RTSAs between cemented and uncemented humeral stems with the only significant difference being improved internal rotation in the uncemented group.
Similar functional outcomes for RTSA as found in this study have also been reported in the literature. Constant scores consistently improve after RTSA with similar results to those found in this study [7, 9, 10, 14–16, 20, 21, 23, 25–27]. One of these studies, which, unlike our study, included revisions in the analysis, reported similar Constant scores in cemented and uncemented RTSAs [7]. Average ASES scores after RTSA were also similar to those found in the literature (ASES score 77 versus 68–76) with significant improvement in all studies [16–18, 22, 23]. The improvement of 6.3 points seen in this study shows a significant improvement in shoulder function after RTSA. The postoperative SST-12 score of 9 reported in this study is higher than previously reported after RTSA (6.1–8) [16, 22, 27, 28].
The rate of humeral loosening reported in the literature has been low in RTSA. The two largest studies of RTSA that mentioned humeral loosening reported a 0 and 1.5 % humeral loosening rate in 501 and 337 patients, respectively [8, 20]. Three primary reverse shoulder arthroplasty studies mention the incidence of loosening of cemented and uncemented humeral stems; however, no study directly compares results of cemented versus uncemented humeral stem fixation. Sirveaux et al. [10] reported a 2 % loosening rate in cemented stems versus 0 % in uncemented stems in 80 patients. Sadoghi et al. [9] had a 5 % loosening rate with cemented stems and a 0 % loosening rate in uncemented humeral stems in 68 patients; however, there were only ten patients in the uncemented group. Ek et al. had no loosening in 40 patients followed for a mean of 7.8 years. The study that includes the largest number of uncemented humeral stems including both primary and revision RTSA reports a humeral loosening rate of 0 % in 98 patients with less than two years of follow-up [3].
The infection rate of 1 % in this study is similar to other reported studies in the literature. Infection rates for primary RTSA range from 0 to 18 % with the majority under 4 % [4, 5, 8, 10, 13, 15, 17, 22, 23]. The scapular notching rate of 11 % in this study is lower than most RTSA studies in the literature. Notching rates with a Grammont-style implant vary from 21 to 96 % [2, 5, 15, 18, 21, 29]. The most recent report on the lateral glenoid prosthesis reported a 9 % notching rate [16].
The primary limitation of this study is the non-randomisation of cementation versus press-fitting of the humeral stems which could create a selection bias. The senior surgeon early in the series cemented all the implants and later in the series cemented almost none of the stems. Although this does not represent randomisation, it demonstrates the limited possibility of selection bias. The demographics of both patient groups were similar, again showing limited possibility of selection bias. There were more women in the cemented group; however, presently in our practice all primary reverse shoulder arthroplasties are uncemented. Currently, if there is any question of the quality of metaphyseal bone, then impaction grafting of the metaphysis from the humeral head is performed irrespective of sex. In addition, patients with acute fracture, fracture sequelae and inflammatory arthropathy were excluded from this study in order to remove any bias in this small cohort due to the higher rate of complications reported historically in these patients.
Press-fitting of a metaphyseal grit-blasted humeral stem in primary RTSA provides similar functional outcomes, radiographic outcomes, complication rates and humeral loosening rates when compared to cemented stems at a minimum follow-up of two years. Further studies with a larger number of patients and additional follow-up are needed to see if similar results are obtained in the long term.
References
Sanchez-Sotelo J (2009) Reverse total shoulder arthroplasty. Clin Anat 22:172–182. doi:10.1002/ca.20736
Cheung E, Willis W, Walker M, Clark R, Frankle MA (2011) Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 19:439–449
Bogle A, Budge M, Richman A, Miller RJ, Wiater JM, Voloshin I (2013) Radiographic results of fully uncemented trabecular metal reverse shoulder system at 1 and 2 years’ follow-up. J Shoulder Elbow Surg 22:e20–e25. doi:10.1016/j.jse.2012.08.019
Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G (2009) Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 18:600–606. doi:10.1016/j.jse.2009.03.011
Ek ETH, Neukom L, Catanzaro S, Gerber C (2013) Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg 22:1199–1208. doi:10.1016/j.jse.2012.11.016
Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G (2006) Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am 88:1742–1747
Melis B, DeFranco M, Lädermann A, Molé D, Favard L, Nérot C, Maynou C, Walch G (2011) An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br 93:1240–1246. doi:10.1302/0301-620X.93B9.25926
Nowinski RJ, Gillespie RJ, Shishani Y, Cohen B, Walch G, Gobezie R (2012) Antibiotic-loaded bone cement reduces deep infection rates for primary reverse total shoulder arthroplasty: a retrospective, cohort study of 501 shoulders. J Shoulder Elbow Surg 21:324–328. doi:10.1016/j.jse.2011.08.072
Sadoghi P, Vavken P, Leithner A, Hochreiter J, Weber G, Pietschmann MF, Müller PE (2011) Impact of previous rotator cuff repair on the outcome of reverse shoulder arthroplasty. J Shoulder Elbow Surg 20:1138–1146. doi:10.1016/j.jse.2011.01.013
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 86-B:388–395. doi:10.1302/0301-620X.86B3.14024
Verborgt O, El-Abiad R, Gazielly DF (2007) Long-term results of uncemented humeral components in shoulder arthroplasty. J Shoulder Elbow Surg 16:S13–S18. doi:10.1016/j.jse.2006.02.003
Sanchez-Sotelo J, Wright TW, O’Driscoll SW, Cofield RH, Rowland CM (2001) Radiographic assessment of uncemented humeral components in total shoulder arthroplasty. J Arthroplasty 16:180–187. doi:10.1002/ca.20736
Litchfield RB, McKee MD, Balyk R, Mandel S, Holtby R, Hollinshead R, Drosdowech D, Wambolt SE, Griffin SH, McCormack R (2011) Cemented versus uncemented fixation of humeral components in total shoulder arthroplasty for osteoarthritis of the shoulder: a prospective, randomized, double-blind clinical trial-a JOINTs Canada Project. J Shoulder Elbow Surg 20:529–536. doi:10.1016/j.jse.2011.01.041
Boileau P, Watkinson D, Hatzidakis AM, Hovorka I (2006) Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 15:527–540. doi:10.1016/j.jse.2006.01.003
Castricini R, Gasparini G, Di Luggo F, De Benedetto M, De Gori M, Galasso O (2013) Health-related quality of life and functionality after reverse shoulder arthroplasty. J Shoulder Elbow Surg 22:1639–1649. doi:10.1016/j.jse.2013.01.020
Cuff D, Clark R, Pupello D, Frankle M (2012) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of five years, of a previous report. J Bone Joint Surg Am 94:1996–2000. doi:10.2106/JBJS.K.01206
Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M (2005) The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 87:1697–1705. doi:10.2106/JBJS.D.02813
Ji JH, Jeong JY, Song HS, Ok JH, Yang SJ, Jeon BK, Kim TG, Moon YS, Kim YS (2013) Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg 22:1102–1107. doi:10.1016/j.jse.2012.07.019
Lädermann A, Walch G, Lubbeke A, Drake GN, Melis B, Bacle G, Collin P, Edwards TB, Sirveaux F (2012) Influence of arm lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg 21:336–341. doi:10.1016/j.jse.2011.04.020
Lévigne C, Boileau P, Favard L, Garaud P, Molé D, Sirveaux F, Walch G (2008) Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg 17:925–935. doi:10.1016/j.jse.2008.02.010
Mizuno N, Denard PJ, Raiss P, Walch G (2012) The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop 36:1647–1653. doi:10.1007/s00264-012-1539-0
Mulieri P, Dunning P, Klein S, Pupello D, Frankle M (2010) Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am 92:2544–2556. doi:10.2106/JBJS.I.00912
Nolan BM, Ankerson E, Wiater JM (2011) Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res 469:2476–2482. doi:10.1007/s11999-010-1683-z
Kadum B, Mukka S, Englund E, Sayed-Noor A, Sjödén G (2014) Clinical and radiological outcome of the Total Evolutive Shoulder System (TESS®) reverse shoulder arthroplasty: a prospective comparative non-randomised study. Int Orthop 38:1001–1006. doi:10.1007/s00264-013-2277-7
Atoun E, Van Tongel A, Hous N, Narvani A, Relwani J, Abraham R, Levy O (2014) Reverse shoulder arthroplasty with a short metaphyseal humeral stem. Int Orthop 38:1213–1218. doi:10.1007/s00264-014-2328-8
Mizuno N, Denard PJ, Raiss P, Walch G (2012) The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop 36:1647–1653. doi:10.1007/s00264-012-1539-0
Alta TD, Bergmann JH, Veeger DJ, Janssen TW, Burger BJ, Scholtes VA, Willems WJ (2011) Kinematic and clinical evaluation of shoulder function after primary and revision reverse shoulder prostheses. J Shoulder Elbow Surg 20:564–570. doi:10.1016/j.jse.2010.08.022
Wellman M, Struck M, Pastor MF, Gettmann A, Windhagen H, Smith T (2013) Short and midterm results of reverse shoulder arthroplasty according to the preoperative etiology. Arch Orthop Trauma Surg 133:463–471. doi:10.1007/s00402-013-1688-7
Farshad M, Gerber C (2010) Reverse total shoulder arthroplasty—from the most to the least common complication. Int Orthop 34:1075–1082. doi:10.1007/s00264-010-1125-2
Acknowledgments
This study received no outside funding.
Conflict of interest
One or more of the authors (K.F. and T.W.) has received funding from Exactech. No other author has a potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Level of evidence: level III cohort therapeutic study
Rights and permissions
About this article
Cite this article
King, J.J., Farmer, K.W., Struk, A.M. et al. Uncemented versus cemented humeral stem fixation in reverse shoulder arthroplasty. International Orthopaedics (SICOT) 39, 291–298 (2015). https://doi.org/10.1007/s00264-014-2593-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2593-6