Abstract
Purpose
The purpose of this study is predicting the clinical and radiological long-term outcome and identifying prognostic factors of Legg-Calvé-Perthes disease (LCPD) in Catterall 2 and 3 hips.
Methods
Sixty hips (59 patients) were diagnosed with LCPD between 1959 to 1974 and were followed prospectively. Forty-two of these 60 hips were classified as Catterall 2 or 3. In 2002, 33 hips (32 patients) with Catterall type 2 or 3 were evaluated clinically and radiographically. In 2010, 27 hips (26 patients) were re-evaluated.
Results
In 2002, 15 hips had Catterall 2 type LCPD and 18 hips Catterall 3. Twelve of the 33 hips (36 %) had signs of osteoarthritis. In 2010, 14 hips were classified as Catterall 2 and 13 hips as Catterall 3. Catterall 2 hips had a significantly better Harris Hip Score (HHS) (p = 0.001). There were 15 hips (55 %) with signs of osteoarthritis.
Conclusion
The long-term prognosis of LCPD Catterall type 2 and 3 is relatively benign. However, more than 50 % of the patients will develop signs of osteoarthritis between the 4th and 5th decades. At the latest follow-up a strong increase in the number of cases with osteoarthritis was seen. Sphericity of the femoral head is an important predicting factor in the development of osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Legg-Calvé-Perthes disease (LCPD) of the hip is still one of the most poorly understood orthopaedic diseases. However, up to now prognoses of the outcome of LCPD and treatment strategies remain controversial. The first classification system representing a milestone in the diagnoses and treatment of LCPD was introduced in 1971 by Catterall [1]. In this classification system, the extent of femoral head involvement was used and related to the expected long-term prognosis. There is no discussion about the prognosis of Catterall type 1 or 4. The prognosis of Catterall type 1 is very benign, while patients with Catterall 4 have a poor outcome with early development of osteoarthritis. However, the long-term outcome of patients categorised as Catterall 2 and 3 is less clear [1–3]. Certainly, long-term studies are available, but the long-term prognosis of Catterall type 2 or 3 is not clear as the available long-term studies did not use this classification, because it was not available yet at time of publication or there were no historical lateral X-rays available during follow-up to perform an accurate classification [4].
The extent of femoral head involvement and age at time of onset are described and generally accepted as the most important factors in predicting the outcome of LCPD [5–8]. However, Weinstein suggested in 1997 that age at healing of LCPD is a more important prognostic factor than age at onset [8, 9].
The purpose of this study was to predict the clinical and radiological long-term outcome of patients that had been diagnosed for Catterall type 2 or 3 at childhood age, with a focus on the development of osteoarthritis. In addition, we tried to identify the influence of other prognostic factors of LCPD in the long-term, such as the age at onset, age at healing and radiographic signs.
Material and methods
Sixty hips (59 patients) were diagnosed with LCPD at the Orthopaedic Department of the Radboud University Medical Centre in Nijmegen between 1959 and 1974. In this period, one of the senior authors (R.F.) followed these patients prospectively. All patients were retrospectively staged in 1974 according to the Catterall classification based on AP and lateral X-rays. All patients were followed until radiological healing. As the long-term prognosis of Catterall 1 and 4 is clear, we decided to focus on 42 of the 60 hips (41 patients) classified as Catterall 2 or 3.
After healing, patients were not followed on a regular basis. In 2002, one of the authors (R.v.K.) traced 35 of these 41 patients with Catterall 2 and 3. Three of the 35 patients refused to cooperate for different reasons. In total 32 patients (33 hips) were investigated in 2002.
At that time the group consisted of 27 men and five women. One patient suffered bilateral LCPD. Fifteen hips were classified as Catterall 2 and 18 hips as Catterall 3. The median age at time of follow-up was 42.7 years (range, 30.7–49.6 years). The median time to follow-up was 35.5 years (range, 25–42 years) (Table 1).
At childhood age, all these patients were first treated in a conservative way according to the protocol at that time, which consisted of bed rest with or without a period of traction or a spica cast followed by a period of an ischial weight-bearing calliper. In the Catterall 2 group, one patient underwent a decompression of the femoral head. In the Catterall 3 group, two patients underwent decompression of the femoral head. Nine hips in the Catterall 3 group underwent surgical interventions, mainly for (sub)luxation of the femoral head. Treatment consisted of a femoral varus derotational osteotomy in most of the cases. In this study the outcome of the different surgical interventions were not analysed and compared in predicting the clinical and radiological outcome.
At time of follow-up in 2002, all 32 patients were evaluated clinically and radiographically. Clinical evaluation consisted of the Harris Hip Score (HHS). Radiographic examination consisted of standard AP and lateral views. These radiographs were classified according to the Mose classification system for head irregularities [10]. According to Mose, a spherical head was classified as good, an elliptical head with <2-mm loss of sphericity was rated fair and an irregular head with >2-mm loss of sphericity was classified as poor [5, 10]. Also, the acetabular congruency was classified as spherically congruent, aspherically congruent and aspherically incongruent [8, 11]. Radiographic osteoarthritis was classified with the Kellgren scoring system [12].
All physical examinations and radiographic evaluation were performed by two of the authors (R.v.K. and B.W.S.). A total hip arthroplasty was considered to be the study endpoint.
Early in 2010 the patient cohort of 2002 was contacted again. Six patients were not re-evaluated in 2010, because two patients were lost to follow-up, one patient died of unknown cause, one patient refused to cooperate and two patients had a total hip replacement before 2002 and were not contacted again because they reached the study endpoint. Thus, 26 patients (27 hips) were re-evaluated with a median time to follow-up of 41.6 years (range, 35.9–48.5 years). This group consisted of 23 men and three women. Fourteen hips were classified as Catterall 2 and 13 hips as Catterall 3 (Tables 2 and 3).
Again, clinical and radiological data were collected (including the same questionnaires and classifications) and compared to the outcome data in 2002. The Mose classification of 2002 was used, because we did not expect changes in the head (ir)regularities over time.
Progression of the osteoarthritis was analysed with the Kellgren score. All physical examinations were done by one author (N.H.) and all radiographic evaluations were performed by two of the authors (N.H. and B.W.S.).
This study was approved by the IRB of our institute.
All statistical analyses were performed by a professional medical statistician (J.H.).
The Mann–Whitney U test was used to test differences in HHS and the Fisher’s exact test to test difference in percentage osteoarthritis (Kellgren score ≥2) between groups for statistical significance. A p value of <0.05 was considered to be statistically significant. The statistical analysis was performed using SAS 9.2 for Windows.
Results
Between 2002 and 2010 there was a strong increase in the number of cases with radiological signs of osteoarthritis. More than 50 % of the patients developed signs of osteoarthritis between the 4th and 5th decades. In 2002, 12 of the 33 available hips (36 %) had signs of osteoarthritis (Table 1).
Of the subsequent cohort available in 2010, we found radiographic signs of osteoarthritis in 15 of 27 hips (56 %) (Table 4). Seven hips were classified as Catterall 2 and eight as Catterall 3 (Kellgren 2, n = 12; Kellgren 3, n = 1; Kellgren 4, n = 2). Three patients in the Catterall 2 and one in the Catterall 3 group had developed signs of osteoarthritis between 2002 and 2010.
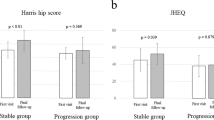
In 2010, patients in the Catterall 3 group had a significantly lower HHS in comparison to patients in the Catterall 2 group (Mann Whitney U test, p = 0.001) (Table 4).
Age at onset was not considered as a prognostic factor in predicting osteoarthritis. Patients with osteoarthritis at time of follow-up, were older at onset of the disease, but this was not statistically significant in comparison with patients without osteoarthritis (p = 0.095).
Also, age at healing was not a prognostic factor in predicting osteoarthritis (p = 0.704).
Sphericity of the femoral head is an important predicting factor in the development of osteoarthritis. Of the total cohort in 2010, there were nine hips (33 %) with a spherical head, seven hips (26 %) with an elliptical head and 11 hips (41 %) with an irregular head according to Mose (Table 4).
Patients with an irregular head according to Mose had a significantly lower HHS compared with patients with a spherical or an elliptical head (91 versus 100) (Mann Whitney U test, p = 0.006). These patients had also significant more osteoarthritis at time of follow-up (Fisher’s exact test, p = 0.047). According to the acetabular congruency, nine of 27 hips were spherically congruent, 12 hips aspherically congruent and 6 hips aspherically incongruent. Patients with an aspherically incongruent hip joint had a lower HHS compared with patients with a (a)spherically congruent hip joint (90 versus 100). This difference nearly reached the level of statistical significance (Mann Whitney U test, p = 0.055). No statistical significance was found regarding the incidence of osteoarthritis in these hips (Fisher’s exact-test, p = 0.182) (Table 4).
Discussion
The purpose of this study was to predict the clinical and radiological long-term outcome of patients with LCPD, classified as Catterall type 2 or 3. Between the 4th and 5th decades of life, more than 50 % of the patients had signs of osteoarthritis. We identified sphericity of the femoral head as a prognostic factor in the development of osteoarthritis. The Catterall type and the sphericity of the femoral head were predictors for the clinical outcome according to the HHS.
Our study is a historical prospective cohort study, but with no regular follow-up done till 2002. In long-term follow-up studies from the past the Catterall classification was not used, because it was not readily available at time of publication or there were no lateral X-rays available during follow-up [4].
Nowadays this classification is the subject of discussion because of the presumed lack of inter-observer validation [13, 14].
Although many long-term follow-up studies have been published, the number of recent studies with a follow-up longer than 40 years is scarce. Different studies showed different numbers of osteoarthritis [6, 11, 15–17]. Froberg et al. [15] showed in a study with a mean follow-up of 47 years that 13 % of the patients with LCPD in the study group had an arthroplasty, in comparison with none of the patients without LCPD in the control group. McAndrew et al. [6] described an average period of follow-up of 47.7 years. Fifty percent of the patients had osteoarthritis in the 6th decade of life and 40 % had an arthroplasty performed. Lecuire et al. [17] described a follow-up period of over 50 years. Twenty-four of 51 hips had (very) irregular heads; despite that, only 12 of 51 hips were replaced at the time of the latest follow-up.
We reported a rate of osteoarthritis of 56 %. This is in agreement with the results in the literature.
In our study group there were two patients with a total hip arthroplasty after a mean follow-up of 41.6 years. These patients were both in the Catterall 3 group. We have no information as to whether the patients lost to follow-up underwent a total hip arthroplasty after the last evaluation in 2002. Of the patients lost to follow-up, we only know that one of the patients already had radiographic signs of osteoarthritis in 2002.
A generally accepted factor in predicting outcome of LCPD is age at onset [4, 5, 7]. In contrast to the literature, we found in our study that patients with osteoarthritis at time of follow-up were not significantly older at onset of the disease.
Many studies report a better prognosis for patients with healing before the age of eight to nine years, because after that age bone remodelling will decrease [6, 8]. We expected that recovery after the age of 8.5 years was prognostically unfavourable in the long-term because of the greater risk of developing an aspherically incongruent hip joint, but we did not find a significant difference.
An important factor in determining the long-term prognosis according to our study is sphericity of the femoral head. Mose et al. [10] described that sphericity of the femoral head at skeletal maturity is a prognostic factor for osteoarthritis in the long-term. Irregular femoral heads had a greater incidence of osteoarthritis. In our study, we found 11 hips with an irregular head (41 %). Nine of these 11 hips had signs of osteoarthritis at time of follow-up (p = 0.047). This number of osteoarthritis is in comparison with the literature. Perpich et al. [18] described a poor result in 17 of 38 hips (43 %). Fabry et al. [5] found a fair or poor result in 100 % of the cases. Lecuire [17] concluded that the worse the deformation of the femoral head is, the higher the risk of osteoarthritis in the future. Yrjönen [19] showed that in their group of 96 patients (106 hips), 65 hips had a poor outcome in sphericity at skeletal maturity. Of these 65 hips, 15 hips had no signs of osteoarthritis at time of follow-up. Norlin et al. [20] found no spherical head at time of follow-up of patients with an average age of 22.4 years.
According to the congruency of the hip joint, we found six patients with an aspherically incongruent hip joint, five of them had signs of osteoarthritis at time of follow-up (p = 0.182). Stulberg et al. [11] stated that patients with an aspherically congruent hip joint have a greater risk of developing osteoarthritis in adulthood, between the age of 40 and 50 years. In patients with an aspherically incongruent hip joint, the chance of developing a severe early osteoarthritis is great. McAndrew et al. [6] described that the outcome in spherically congruent hips is usually good. Even aspherically congruent hip joints give satisfactory long-term results. Ippolito et al. [4] reported osteoarthritis in 17 of 61 patients. Sixteen patients had an aspherically congruent hip joint and in one patient the hip joint was aspherically incongruent. They concluded that the incidence of osteoarthritis in patients with a spherically congruent hip joint is the same as in the normal healthy population. Developing osteoarthritis in adult life is seen in patients with an aspherically congruent hip joint. Aspherically incongruent hips will give early osteoarthritis.
Patients in the Catterall 3 group had a significantly worse HHS in comparison to patients in the Catterall 2 group. We think this is irrelevant. The first reason is that the lowest HHS in the Catterall 2 group is 91 versus 59 in the Catterall 3 group. This is overall a relatively good outcome. The second reason is that LCPD in both Catterall groups had a relatively mild course of disease with the development of osteoarthritis between the 4th and 5th decades.
A limitation of this study is the small patient group. During follow-up, 13 of 41 patients were lost. Because of the young age of this population at the time of radiological healing, six of the 41 patients were not traceable in 2002 at their known address. In 2010, another two patients were untraceable. We had no influence on a total of 14 patients who refused to cooperate.
We have no information about the condition of the hip of the patients lost to follow-up. Only one of the patients lost to follow-up in 2010 had radiographic signs of osteoarthritis in 2002.
Another limitation of this study is that the outcome of the different surgical interventions was not compared in predicting the clinical and radiological outcome. It is unknown if these procedures have influence on the results in terms of development of osteoarthritis.
A strong point of this study is the long-term follow-up. Another strong point is that this study is only focused on the follow-up of patients classified as Catterall 2 or 3. All patients were followed from onset of disease until healing. In our opinion, the prognosis of patients with Catterall 1 is always good, and most of the patients with Catterall 4 hips will develop early osteoarthritis.
In conclusion, LCPD had a mild course of disease in Catterall 2 and 3 hips. Between the 4th and 5th decades of life, more than 50 % of the patients had signs of osteoarthritis. A strong increase in the number of cases with radiological signs of osteoarthritis was seen between 2002 and 2010. Patients in the Catterall 3 group and patients with an irregular head according to Mose had a significantly lower HHS at time of follow-up. According to the Kellgren score, patients with an irregular femoral head according to Mose had significantly more osteoarthritis.
In our study, age at onset, age at healing and acetabular congruency were not of predictive value in osteoarthritis.
References
Catterall A (1971) The natural history of Perthes’ disease. J Bone Joint Surg (Br) 53:37–53
Fulford GE, Lunn PG, Macnicol MF (1993) A prospective study of nonoperative and operative management for Perthes’ disease. J Pediatr Orthop 13:281–285
Mukherjee A, Fabry G (1990) Evaluation of the prognostic indices in Legg-Calve-Perthes disease: Statistical analysis of 116 hips. J Pediatr Orthop 10:153–158
Ippolito E, Tudisco C, Farsetti P (1987) The long-term prognosis of unilateral Perthes’ disease. Clin Orthop Relat Res 69:243–250
Fabry K, Fabry G, Moens P (2003) Legg-Calve-Perthes disease in patients under 5 years of age does not always result in a good outcome Personal experience and meta-analysis of the literature. J Pediatr Orthop B 12:222–227
McAndrew MP, Weinstein SL (1984) A long-term follow-up of Legg-Calve-Perthes disease. J Bone Joint Surg Am 66:860–869
Wiig O, Terjesen T, Svenningsen S (2008) Prognostic factors and outcome of treatment in Perthes’ disease: A prospective study of 368 patients with five-year follow-up. J Bone Joint Surg (Br) 90:1364–1371
Yrjonen T (1999) Long-term prognosis of Legg-Calve-Perthes disease: A meta-analysis. J Pediatr Orthop B 8:169–172
Weinstein SL (1997) Natural history and treatment outcomes of childhood hip disorders. Clin Orthop Relat Res 344:227–242
Mose K, Hjorth L, Ulfeldt M, Christensen ER, Jensen A (1977) Legg Calve Perthes disease. The late occurence of coxarthrosis. Acta Orthop Scand Suppl 169:1–39
Stulberg SD, Cooperman DR, Wallensten R (1981) The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am 63:1095–1108
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Christensen F, Soballe K, Ejsted R, Luxhoj T (1986) The Catterall classification of Perthes’ disease: An assessment of reliability. J Bone Joint Surg (Br) 68:614–615
Ritterbusch JF, Shantharam SS, Gelinas C (1993) Comparison of lateral pillar classification and Catterall classification of Legg-Calve-Perthes’ disease. J Pediatr Orthop 13:200–202
Froberg L, Christensen F, Pedersen NW, Overgaard S (2011) The need for total hip arthroplasty in Perthes disease: A long-term study. Clin Orthop Relat Res 469:1134–1140
Gower WE, Johnston RC (1971) Legg-Perthes disease. Long-term follow-up of thirty-six patients. J Bone Joint Surg Am 53:759–768
Lecuire F (2002) The long-term outcome of primary osteochondritis of the hip (Legg-Calve-Perthes’ disease). J Bone Joint Surg (Br) 84:636–640
Perpich M, McBeath A, Kruse D (1983) Long-term follow-up of Perthes disease treated with spica casts. J Pediatr Orthop 3:160–165
Yrjonen T (1992) Prognosis in Perthes’ disease after noncontainment treatment. 106 hips followed for 28-47 years. Acta Orthop Scand 63:523–526
Norlin R, Hammerby S, Tkaczuk H (1991) The natural history of Perthes’ disease. Int Orthop 15:13–16
Acknowledgments
We declare that we have no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heesakkers, N., van Kempen, R., Feith, R. et al. The long-term prognosis of Legg-Calvé-Perthes disease: a historical prospective study with a median follow-up of forty one years. International Orthopaedics (SICOT) 39, 859–863 (2015). https://doi.org/10.1007/s00264-014-2589-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2589-2