Abstract
Human epidermal growth factor receptor type 2 (HER2)-positive breast cancer that is treated with anti-HER2/neu monoclonal antibody (mAb) is not free from late recurrences. Addition of anti-4-1BB mAb to anti-HER2/neu mAb has been demonstrated to strengthen the cytotoxic antitumor response. Our study expands on this by revealing the influence of anti-4-1BB mAb addition on the immune memory of anti-HER2/neu mAb. We designed murine breast cancer models by implanting TUBO and TUBO-P2J cell lines in mice, which were then treated with anti-HER2/neu and/or anti-4-1BB mAb. After complete surgical and/or chemical regression of the tumor, the mice were rechallenged with a second injection of cancer cells. Notably, anti-HER2/neu and anti-4-1BB mAb combination therapy had a synergistic antitumor effect at the initial treatment. However, the combination therapy did not evoke immune memory, allowing the tumors to thrive at rechallenge with reduced CD44+ expression in CD8+ T cells. Immune memory was also impaired when anti-4-1BB mAb was administered to naive CD8+ T cells but was sustained when this was administered to activated CD8+ T cells. In an attempt to resist the loss of immune memory, we controlled the dose of anti-4-1BB mAb to optimize the stimulation of activated CD8+ T cells. Immune memory was achieved with the dose regulation of anti-4-1BB mAb to 1 mg/kg in our model. Our study demonstrates the importance in understanding the adaptive immune mechanism of anti-HER2/neu and anti-4-1BB mAb combination therapy and suggests a dose optimization strategy is necessary to ensure development of successful immune memory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human epidermal growth factor receptor type 2 (HER2) overexpression, observed in 20–30% of invasive breast carcinomas, is associated with decreased overall survival [1]. Fortunately, the impact of trastuzumab, an anti-HER2/neu monoclonal antibody (mAb), on HER2 positive breast cancer treatment has been profound. The mechanism of trastuzumab depends on both antibody-dependent cellular cytotoxicity (ADCC) and the adaptive immune system [2, 3], and adding trastuzumab to adjuvant therapy has increased disease-free survival by 51% and has decreased the risk of death by 41% [4]. However, even with the help of prolonged adjuvant anti-HER2/neu mAb treatment, approximately 20–30% of HER2 positive breast cancers still undergo late recurrences [5]. Currently, clinicians are aiming to boost the action of anti-HER2/neu antibody treatment to overcome the recurrence of cancer.
4-1BB, a member of the TNF receptor family co-stimulatory receptor, is expressed on a wide spectrum of immune cells, including B cells, activated T cells, natural killer (NK) cells, dendritic cells, monocytes, and neutrophils [6]. The interaction between 4-1BB and its ligand can trigger an activation signal in all cell types. Thereafter, agonistic monoclonal antibodies targeting 4-1BB have been developed to harness 4-1BB signaling for cancer immunotherapy. Although the anti-cancer effect of anti-4-1BB antibodies might differ in different cell types, current data show that this effect is mediated by increasing the proliferation, differentiation, and survival of CD8+ T cells together with their cytolytic properties [7, 8].
A previous study verified that the addition of anti-4-1BB mAb promoted the ADCC of anti-HER2/neu mAb by relying on CD8+ T cells in a mouse breast cancer tumor model [9]. However, the impact on adaptive memory has not been well discussed. If anti-4-1BB mAb is able to heighten an enduring immunological response of anti-HER2/neu mAb, this might protect breast cancer patients from recurrence. Therefore, we investigated the immune memory function of anti-4-1BB and anti-HER2/neu mAbs in a mouse breast cancer model. Unexpectedly, immune memory was not incorporated with simple combination therapy. Therefore, we aimed to explore the mechanism of the absence of immune memory in the combination of anti-4-1BB and anti-HER2/neu mAbs. Furthermore, our study proposes a strategy to achieve immune memory in combined anti-HER2/neu and anti-4-1BB mAb therapy.
Materials and methods
Cell lines
The HER2/neu positive mouse breast cancer cell line TUBO and its variant TUBO-P2J cell line reported previously [10] were cultured in Dulbecco’s modified Eagle’s medium supplemented with 10% heat-inactivated fetal bovine serum (FBS; HyClone, Logan, UT, USA), 10% NCTC-109 medium, 2 mM L-glutamine, 0.1 mM minimal essential medium non-essential amino acids, 100 U/mL penicillin, and 100 mg/mL streptomycin. The cells were maintained in a humidified incubator at 37 °C and 5% CO2 and passaged every 3 days.
In vivo study
Female BALB/c or C57BL/6 mice (5 to 6-weeks-old) were purchased from Orient Bio (Daejeon, Korea) and used for experiments when they reached a body weight of 17–20 g (6 to 8-weeks-old). The mice were allowed to acclimatize before the experiments under specific pathogen-free conditions at the animal care facility of the College of Medicine (Inje University). The experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee of Inje University (2019-002).
TUBO cells (1 × 106 cells/mouse) or a mix of TUBO and TUBO-P2J cells (1 × 106 TUBO cells containing 1% TUBO-P2J cells) were subcutaneously (s.c.) injected into the backs of mice anesthetized with a mixture of ketamine (90 mg/kg) and xylazine (10 mg/kg). For tumor rechallenge experiments, mice that were tumor-free for at least 1 month after complete rejection of the treatment or surgical tumor removal were rechallenged by separate s.c. injections of 5 × 106 TUBO cells (left upper back) and 1 × 105 TUBO-P2J cells (right upper back) at sites differing from those of the primary tumor. Tumor volume was calculated as (a × b × c)/2, where a–c are the measurements along three orthogonal axes. When the tumor volume reached approximately 150 mm3, the mice were treated with a vehicle control antibody (mIgG), anti-HER2/neu (clone 7.16.4) antibody, and 4-1BB antibody colne 3H3 (kindly provided by Byungsuk Kwon) [11]. An anti-HER2/neu antibody was intraperitoneally (i.p.) administered at doses of 10 mg/kg and 5 mg/kg on three injections every 4 days. The 4-1BB antibody (5 mg/kg) was administered i.p. on days 14 and 18 after tumor implantation.
SIINFEKL (a peptide of amino acids 257–264 of ovalbumin)-specific CD8+ T cells were isolated from the lymphoid of OT-1 mice using anti-thy1.1 and CD8 magnetic beads and magnetic-activated cell sorting (MACS). SIMFEKL-specific CD8+ T cells (2 × 106 cells/mice) were intravenously (i.v.) transferred and then immunized s.c. with 20 µg of ovalbumin (OVA) emulsified in incomplete Freund’s adjuvant (IFA) into C57BL/6 mice.
Flow cytometry
The immune cell population and activation status were evaluated using flow cytometry. Briefly, single-cell suspensions were obtained by collagenase digestion of resected tumors and were then incubated with fluorochrome-conjugated monoclonal antibodies against surface markers after incubation with the Fc blocker 2.4G2. Antibodies against mouse CD45 (clone 30-F11), CD3 (clone 145-2C11), CD8a (clone 53–6.7), CD4 (clone GK1.5), CD107a (clone 1D4B), CD44 (clone IM7), CD62L (clone MEL-14), Thy1.1 (clone HIS51), CD279 (PD1) (clone RMP1-30) conjugated to fluorescein isothiocyanate (FITC), phycoerythrin (PE), allophycocyanin (APC), or phycoerythrin cyanine7 (PE-Cy7) were purchased from eBioscience (San Diego, CA, USA). Intracellular labeling was performed using the BD Cytofix/CytopermTM kit (BD Biosciences) according to the manufacturer’s instructions. A cell suspension at 1.5 × 106 cells/mL was stimulated with phorbol myristate acetate (50 ng/mL) plus ionomycin (750 ng/mL) in Golgi PlugTM-containing medium for 5 h at 37℃ and was then labeled with surface molecules. After washing, the cells were fixed with Cytofix/Cytoperm solution and Perm/WashTM buffer and then labeled with anti-mouse IFN-g-PE (clone XMG1.2) antibodies (all from eBioscience) and analyzed by flow cytometry. For T cell activation experiment, inguinal lymph nodes from control and treated mouse were teased using fine forceps and mechanically disrupted. LN cells were digested for 25 min at 37 °C in RPMI with 500 μg/ml Collagenase IV (Sigma) and 25 μg/ml DNase I (Sigma).
Measurement of IFN-g secretion by T cells by enzyme-linked immunospot (ELISPOT) assay
The ELISPOT assay was performed using the Mouse IFN-γ ELISPOT kit (BD Biosciences) according to the manufacturer’s instructions. The ELISPOT 96-well plates were coated overnight at 4 °C with a capture antibody and then blocked with 10% FBS in RPMI 1640 medium. Spleens from control and treated mice were passed through a 100-μm nylon cell strainer. After the first centrifugation (5 min 400 × g), tissue supernatant was collected. Splenocytes were then resuspended in RPMI 1640 medium (Gibco, ThermoFisher). Splenocytes (4 × 105) were co-cultured at a 10:1 ratio with tumor antigen-pulsed bone marrow-derived dendritic cells (BMDCs) that had been pulsed overnight with triplicates of freeze-thawed lysed TUBO or TUBO-P2J cells. Concanavalin A (5 mg/mL) was used as a positive control to confirm the IFN-γ responsiveness of cells cultured with tumor antigen-pulsed BMDCs. After a 24-h incubation, cells were removed from the wells by washing, and a biotinylated anti-IFN-γ antibody (clone XMG1.2) was added to the wells. Spots were developed using streptavidin-conjugated horseradish peroxidase and a 3-amino-9-ethyl-carbazole substrate. IFN-γ spots were counted using an ELISPOT plate reader (AID Autoimmun Diagnostika, Strassberg, Germany).
Results
The combination therapy of anti-HER2/neu mAb and agonistic anti-4-1BB mAb enhanced their antitumor effect but was inadequate in suppressing lethal rechallenge
To test whether the combination therapy of anti-HER2/neu mAb and agonistic anti-4-1BB mAb could reduce tumor burden additively and synergistically, we established a treatment model for TUBO and/or TUBO-P2J cells. BALB/c mice bearing tumors derived from either TUBO cells or a mixture of TUBO and TUBO-P2J cells were treated with antibodies. Tumor-bearing mice were treated with anti-HER2/neu mAb and/or anti-4-1BB mAb (Fig. 1a, e). Most of the treatments had significant treatment effects on both tumors. For TUBO tumors, all regimens significantly reduced tumor size after administration (Fig. 1b) (anti-HER2/neu mA and anti-4-1BB mAb: p < 0.05, combination therapy: p < 0.01, compared with control group). In particular, the combination of anti-HER2/neu and anti-4-1BB mAbs resulted in improved antitumor efficacy compared with that of anti-HER2/neu or anti-4-1BB alone (p < 0.05). In TUBO and TUBO-P2J cell mixed tumors, anti-HER2/neu mAb did not significantly decrease tumor size. In contrast, anti-4-1BB mAb and its combination with anti-HER2/neu mAb induced effective tumor regression (p < 0.001 and p < 0.001, respectively) (Fig. 1f). In addition, in concordance with TUBO tumors, the combination therapy improved the anticancer effect in TUBO and TUBO-P2J cell mixture tumors (p < 0.001). These data support the previous model that anti-4-1BB mAb effectively enhanced the anti-HER2/neu mAb treatment against cancer cells [9, 12].
Combined treatment of anti-HER2/neu antibody 7.16.4 and agonistic anti-4-1BB antibody 3H3 produced synergistic treatment of in HER2-susceptible and HER2-resistant tumors; however, mice who received combined treatment showed less immune memory for protection from lethal rechallenge. a Experimental scheme. b BALB/C mice (n = 3–4) were injected s.c. with 1 × 106 TUBO cells and treated with 200, 100, or 100 µg anti-HER2/neu antibody by i.p. injection on days 14, 28, and 22 after tumor inoculation. Anti-4-1BB antibody (3H3, 100 µg) was administered by i.p. injection on days 14 and 18 after tumor inoculation. The tumor growth was measured. c, d Tumor free, anti-HER2/neu antibody and/or anti-4-1BB antibody-treated BALB/c mice were rechallenged s.c. with 5 × 106 TUBO cells on different sites from those of the primary tumor after complete rejection of primary tumors by surgery. c Individual growth curves of TUBO tumor. d Percent tumor-free mice. e Experimental scheme. f BALB/C mice (n = 5 to 6 per group) were inoculated s.c. with a mixture of 1 × 106 TUBO and 1 × 104 TUBO-P2J cells. TUBO and TUBO-P2J mixed-tumor bearing mice were treated with the anti-HER2/neu antibody and anti-4-1BB antibody, as described in b. The tumor growth was measured. g, h Tumor free, anti-HER2/neu antibody and/or anti-4-1BB antibody-treated BALB/c mice were rechallenged s.c. with 5 × 106 TUBO cells (on left upper back) and 1 × 104 TUBO-P2J (on right upper back) separately after complete rejection of primary tumors by surgery. g Individual growth curves of TUBO and TUBO-P2J tumors. h Individual tumor volume of TUBO and TUBO-P2J on day 35 after rechallenging tumors. The data are expressed as the mean ± SEM of each treatment group. Statistical analysis was performed with an unpaired Student’s t test using GraphPad Prism 5 software to compare differences between the vehicle-control group and other groups (*p < 0.05; **p < 0.01; ***p < 0.001) or between the anti-HER2/neu antibody-treated group and the other groups (#p < 0.05; ##p < 0.01; ###p < 0.001)
Having confirmed that anti-HER2/neu mAb and/or anti-4-1BB mAb were effective antitumor agents, we sought to investigate the adaptive immune function of the antibody therapies. Therefore, the rechallenge models were built by surgically resecting all residual tumors, thereby creating a clinical remission state, and re-injecting a mixture of TUBO cells and/or TUBO-P2J cells separately (n = 4 per group).
In the first TUBO cell rechallenge model, 5 × 106 TUBO cells were re-injected at different sites from the primary tumor (Fig. 1a, c). Notably, tumors demonstrated a distinct response to the re-injected agents. The mice previously treated with anti-HER2/neu or anti-4-1BB mAb alone significantly inhibited tumor growth from rechallenge, whereas mice treated with anti-HER2/neu mAb and anti-4-1BB mAb combination therapy showed conflicting results, permitting tumor growth after rechallenge. As a consequence, the group initially treated with anti-HER2/neu mAb and anti-4-1BB mAb combination had fewer mice reaching complete remission against tumor rechallenge (Fig. 1d).
In the second rechallenge model, 5 × 106 TUBO cells and 1 × 105 TUBO-P2J cells were re-injected at separate sites on BALB/c mice (on left upper back and right upper back, respectively) that had been cured of tumors based on a mix of TUBO and TUBO-P2J cells by anti-HER2/neu and/or anti-4-1BB mAb treatment (Fig. 1e, g). As TUBO and TUBO-P2J tumors of combination therapy-treated mice grew, the anti-4-1BB mAb single agent significantly inhibited the growth of both rechallenged tumors. In particular, the volume of combination therapy-treated rechallenged TUBO tumors increased more aggressively, considering the volume of TUBO-P2J (Fig. 1h). In summary, these results verified that the combination of anti-HER2/neu and anti-4-1BB mAbs therapy enhanced the antitumor effect against TUBO and TUBO/TUBO-P2J mixed tumors; however, combined therapy was incapable of inhibiting tumor growth after rechallenge, which was in opposition to the effect seen with anti-HER2/neu and anti-4-1BB mAb single therapies.
The combination of anti-HER2/neu mAb and anti-4-1BB mAb therapy strengthened the initial anti-cancer immune response but contrarily deteriorated the immune memory response
To explore the mechanism underlying the previous results, ELISPOT assays were performed on anti-HER2/neu and/or anti-4-1BB mAb-treated TUBO mouse splenocytes. The mice were sacrificed on day 10 after the first anti-HER2/neu mAb administration. Splenocytes were isolated and ELISPOT assays were performed. The ELISPOT assay revealed a marked increase in IFN-γ expression in splenocytes from TUBO mice treated with a combination of anti-HER2/neu and anti-4-1BB mAbs with that resulting in splenocytes from mice treated with single therapy of anti-HER2/neu or anti-4-1BB mAb (p < 0.01) (Fig. 2a). The upregulated expression of IFN-γ implies that the anti-HER2/neu and anti-4-1BB mAb combination treatment induced an immune response against cancer cells.
Combined treatment of anti-HER2/neu antibody and anti-4-1BB antibody enhanced the induction of antitumor immunity but impaired memory response. a TUBO-tumor bearing mice were treated with anti-HER2/neu antibody and anti-4-1BB antibody, as described in Fig. 1a. The mice were euthanized on day 10 after the first anti-HER2/neu antibody treatment. Splenocytes were isolated and then ELISPOT assays were performed as described in the Materials and Methods section. a Representative ELISPOT assay results. Results are expressed as the mean ± SEM of each group. Statistical analysis was conducted using an unpaired Student’s t test. *p < 0.05; **p < 0.01; ***p < 0.001, as compared with the vehicle-control group. #p < 0.05; ##p < 0.01; ###p < 0.001, as compared with the anti-HER2/neu antibody-treated group. b On day 10 after the first anti-HER2/neu antibody treatment, the tumors were removed to obtain cell suspensions for surface or intracellular staining. Flow cytometric analysis of CD8+ or CD4+ cells, gated on CD45+ cells in tumors. Flow cytometric analysis of CD107a or IFNγ+ cells, gated on CD8+ cells in tumors. c Flow cytometric analysis of CD44+ or CD44+CD62L− cells, gated on CD8+ cells in tumors. The left panels are representative flow cytometry analysis, and the right panels show the data expressed as the mean ± SEM of each treatment group. Statistical analysis was performed with an unpaired Student’s t test using GraphPad Prism 5 software to compare differences between the vehicle-control group and each antibody-treated group (*p < 0.05; **p < 0.01; ***p < 0.001) or between the anti-HER2/neu antibody-treated group and the other antibody-treated groups (#p < 0.05; ##p < 0.01; ###p < 0.001)
To define the immune cells associated with anti-HER2/neu mAb and/or anti-4-1BB mAb treatment, flow cytometric analysis of immune cells was performed. On day 10 after the first treatment, the tumors of TUBO-bearing mice were resected to prepare single cell suspensions, and surface or intracellular staining was performed. Flow cytometric analysis revealed a global increase in CD8+ and CD4+ T cells after mAb treatment (Fig. 2b). In terms of anti-HER2/neu mAb or anti-4-1BB mAb single therapies, the CD8+ T cell population was increased with anti-4-1BB mAb therapy (p < 0.01), and the CD4+ T cell population was increased with anti-HER2/neu mAb therapy (p < 0.01). When treated with the anti-HER2/neu mAb and anti-4-1BB mAb combination, the frequency of both CD8+ and CD4+ T cells was significantly increased (p < 0.001 and p < 0.05, respectively). The proportion of CD107a+CD8+ T cells, which were not influenced by the administration of either anti-HER2/neu or anti-4-1BB mAb, were significantly increased by the combination of anti-HER2/neu and anti-4-1BB mAbs (p < 0.001). Expression of IFN-γ in CD8+ T cells was increased in single anti-HER2/neu mAb and in combination with anti-4-1BB mAb (p < 0.05 and p < 0.05, respectively). These data suggest that the combined application of anti-HER2/neu mAb and anti-4-1BB mAb amplified the immune response.
In contrast, flow cytometry analysis showed that the frequency of CD44+CD8+ T cells and CD44+CD62L−CD8+ T cells was decreased by anti-HER2/neu and anti-4-1BB mAb combination therapy (p < 0.05 and p < 0.01, respectively) (Fig. 2c). The expression of adhesion molecules such as CD44 distinguishes memory CD8+ T cells from naive CD8+ T cells [13]. This suggests that the combination therapy might weaken the immunological memory function, unlike a single agent application. Anti-4-1BB addition might provoke a stronger ADCC, whereas it did not entail the immune memory function of CD8+ T cells.
Naive CD8+ T cells and activated CD8+ T cells induce distinct immune memory after anti-4-1BB mAb treatment
The above experiment showed that the impact on CD8+ T cells, especially the decrease in CD44+CD8+ T cells, was the major change in immune cells associated with the anti-HER2/neu and anti-4-BB mAb combination treatment no longer maintaining adaptive immune function. This was in comparison with the single administration of each mAb, which successfully induced immune memory, allowing the mice to continuously resist rechallenge of tumor cells. Therefore, we sought to elucidate the reason for this phenomenon and aimed to clarify whether the addition of anti-4-BB mAb to anti-HER2/neu mAb mainly affected naive T cells or activated T cells. Therefore, experiments on immunized mice with either naive T cells or activated T cells were performed using an anti-4-1BB agent. Naive or activated OT-1 CD8+ T cells were transferred into C57BL/6 mice and then immunized with 20 µg of OVA emulsified in IFA (Fig. 3a). Mice were treated with 100 μg of rat IgG or anti-4-1BB mAb on days 2 and 4. The mice were boosted with 20 μg of OVA emulsified in IFA on day 21. Inguinal LN cells were prepared from each group of mice at 0, 7, 14, 21, or 26 days, stained with anti-CD8 and anti-Thy1.1 mAb, and subsequently analyzed by FACSCanto II. The frequency of both naive CD8+ T cells and activated CD8+ T cells was increased at day 7 after rat IgG and anti-4-1BB mAb treatment (Fig. 3b) and then gradually decreased and diminished by day 21. When rechallenged with 20 μg of OVA emulsified in IFA on day 21, the results of CD8+ T cells were distinct (Fig. 3c). Activated CD8+ T cells of both anti-4-1BB mAb- and rat IgG-treated mice were increased, consistent with the primary injection. However, the naive CD8+ T cells of anti-4-1BB mAb-treated mice were not significantly increased by rechallenge with OVA emulsified in IFA. These results indicated that activation of CD8+ T cells was inevitable in producing immune memory after anti-4-1BB mAb treatment.
4-1BB signaling induces different outcomes in naive and activated T cells. a Experimental scheme. b, c 2 × 106 Thy1.1+ OT-1 CD8+ T cells were injected i.v. into C57BL/6 mice that were immunized s.c. with 20 μg of OVA-emulsified in IFA. As a control, 2 × 106 Thy1.1+ OT-1 CD8+ T cells were injected i.v. into C57BL/6 mice. Rat IgG (100 μg) or anti-4-1BB mAb were administered to the immunized mice at day 2 and 4 via i.p. route. The mice were rechallenged with 20 μg of OVA-emulsified in IFA at day 21. Inguinal LN cells were prepared from each group of mice at day 0, 7, 14, 21 or 26, stained with anti-CD8 and anti-Thy1.1 mAb, and subsequently analyzed by FACS Canto II. Results are mean ± SD (n = 3; *p < 0.05; **p < 0.01)
Dose optimization improves anti-4-1BB response allowing this to attain both an anticancer effect and immune memory
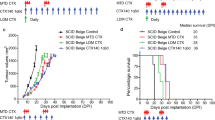
To rescue immune memory after anti-HER2/neu and anti-4-1BB mAb treatment, we hypothesized that dose control of anti-4-1BB mAb would reduce stimulation of naive CD8+ T cells. First, BALB/c mice (n = 3–4 per group) were injected subcutaneously with 1 × 106 TUBO cells and treated with 100 µg of anti-HER2/neu mAb by i.p. injection on days 14, 18, and 22 with or without anti-4-1BB mAb (0.5, 1, or 10 mg/kg) by i.p. injection on days 14 and 18 after tumor inoculation. Tumor growth was also measured (Fig. 4a). When treated with single therapies of either anti-HER2/neu mAb the tumor volume continued to grow, and the treatments did not significantly cure cancer. However, when anti-HER2/neu and anti-4-1BB mAbs were co-administered, all doses combined with anti-4-1BB significantly reduced tumor growth and managed to cure cancer (p < 0.001, p < 0.001, and p < 0.001, respectively). Following the above experiment, the primary tumors were completely resected. At least 1 month after complete remission of the tumor, mAb-treated BALB/c mice were rechallenged with TUBO cells (subcutaneous injection of 5 × 106 cells) at different sites from the primary tumor. Tumor growth was also measured (Fig. 4b). Importantly, mice administered with anti-HER2/neu mAb combined with 10 mg/kg of anti-4-1BB mAb treatment showed tumor regrowth, similar to naive mice. Moreover, mice administered with anti-HER2/neu mAb combined with 0.5 mg/kg of anti-4-1BB mAb eventually presented slight regrowth of tumor as well. This indicates that the optimal therapeutic dose of anti-4-1BB mAb for immunological memory in combination therapy may be 1 mg/kg in our experiments.
Dose optimization of 4-1BB antibody is required in combined therapy with anti-HER2/neu antibody. a BALB/C mice (n = 3 to 4 per group) were injected s.c. with 1 × 106 TUBO cells and treated with 100 μg of anti-HER2/neu antibody by i.p. injection on days 14, 18 and 22, and/or anti-4-1BB antibody (3H3, 0.5, 1, or 10 mg/kg) was administered by i.p. injection on days 14 and 18 after tumor inoculation. The tumor growth was measured. b Tumor-free, antibody-treated BALB/c mice were rechallanged s.c. with 5 × 106 TUBO cells at the different site from the primary tumor at least 1 month after complete rejection of primary tumors. One of two experiments is shown. c Mice were euthanized on -2 days of TUBO tumor rechallenge, and splenocytes were isolated for ELISPOT analysis. ELISPOT assay of IFN-γ+ cells using splenocytes co-cultured with BMDCs pulsed with tumor antigen from TUBO cells lysates. Results were expressed as number of spots per 2 × 105 splenocytes. d On day 1 after the final anti-4-1BB antibody treatment, the tumors were removed to obtain cell suspensions for surface staining. Flow cytometric analysis of PD1+ cells, gated on CD8+ cells in tumors. Data represent mean ± SEM of three independent experiments. p < 0.05, p < 0.01, p < 0.001, each group vs. vehicle control; #p < 0.05, ##p < 0.01, ###p < 0.001, each group vs. anti-HER2/neu antibody and anti-4-1BB antibody (3H3,10 mg/kg) treatment
To clarify the underlying mechanism of the dose dependency of combination therapy, splenocytes were isolated 2 days before the TUBO tumor rechallenge experiment. The IFN-γ ELISPOT analysis for mice treated with anti-HER2/neu mAb combined with either 1 mg/kg or 10 mg/kg of anti-4-1BB mAb was performed (Fig. 4c). The frequency of IFN-γ+ cells was significantly increased in the combination therapy group with 1 mg/kg of anti-4-1BB mAb compared with that in the 10 mg/kg of anti-4-1BB mAb treated group (p < 0.01). In addition, to investigate the association with T cell exhaustion, the expression of PD1 in the tumor tissue was tested one day after the last treatment with anti-4-1BB mAb (Fig. 4a). As a result, the expression of PD1 in CD8 T cells, which was decreased at 1 mg/kg of anti-4-1BB mAb, was restored at 10 mg/kg of anti-4-1BB mAb (Fig. 4d). This implies that anti-HER2/neu mAb combined with a higher dosage of 10 mg/kg of anti-4-1BB mAb leads to immune memory loss, which means that the ability to interfere with T cell exhaustion is lost.
Discussion
Anti-HER2/neu mAb therapy undoubtably takes precedence among the successful antibody antitumor-based therapies and can efficiently restrain the growth of HER2/neu + tumors in vitro and in vivo [1, 14, 15]. The main mechanism of anti-HER2/neu mAb anticancer therapy is enabled by diminishing cell signaling, enabling G1 cell cycle arrest with increased p27Kip1 expression, reducing cyclin E expression, and damaging DNA repair ability [16,17,18]. These multiple effects occur via the prevention of HER2/neu dimerization, where the effector Fc arm of the mAb binds to the Fc receptor on (FcR)-positive inflammatory cells [19]. An interesting report on anti-HER2/neu mAb noted that the in vivo therapy treatment effect was dependent on the existence of FcR signaling [2]. This demonstrated that the anticancer effect of the anti-HER2/neu mAb was weak in FcR-knockout mice. Moreover, when a mutation was made to inhibit FcR binding, anti-HER2/neu could not induce ADCC by NK effector cells. Subsequently, the importance of FcRs in antibody treatment has been emphasized with evidence of its association with breast cancer prognosis [20]. The above findings led to the concept that ADCC may be an influential component of antibody-mediated antitumor effects, and this has been validated over the last two decades. After the administration of antibody treatment, tumor-infiltrating leukocytes (TILs), especially FcR-positive cells, increase in the tumor microenvironment [21, 22]. In addition, improved clinical response to antibody treatment was seen with tumors that had higher infiltration of TILs with greater capacity to perform in vitro ADCC activity [23].
It is becoming clearer that specific agents of cancer cell death, such as targeted monoclonal antibodies, are possibly immunogenic and able to form adaptive anticancer immunity. In addition to FcR-mediated cytotoxic response, anti-HER2/neu mAb induces adaptive immune responses against HER2/neu positive breast cancer patients [24]. In our previous report, we demonstrated the necessity of T cells and adaptive immunity for tumor reduction by anti-HER2/neu therapy [3]. The significance of adaptive immunity was proven by the observation that Rag1-knockout mice lacking adaptive immunity had diminished efficacy in anti-HER2/neu therapy. In wild-type BALB/c mice depleted of CD8+ T cells, the efficacy of anti-HER2/neu mAb was reduced. The presence of immune memory was suggested, and as a result of adaptive immunity, mice completely cleared of tumor after anti-HER2/neu therapy were constantly resistant to tumor rechallenge afterwards. These observations were further investigated using CD8-and IFN-γ-knockout mice [9]. In this study, we demonstrated that both CD8+ cells and IFN-γ from CD8+ cells were essential for anti-HER2/neu therapy. In addition, our study demonstrated the role of NK cells and type-I IFNs in mediating anti-HER2/neu therapy.
In ADCC, FcγRIII (CD16) ligation activates signals within NK cells. In the tumor microenvironment, tumor-targeted antibodies are sensed by the NK cell FcγRIII [25]. Human NK cells increase 4-1BB expression after FcRIII ligation, and subsequent stimulation with anti-4-1BB mAb enhanced ADCC. This strengthened ADCC-mediated tumor regression encourages the use of anti-4-1BB antibodies as a potential candidate for a therapeutic combination [26]. This raised the possibility that anti-4-1BB mAb could be used to capitalize on the ADCC of anti-HER2/neu therapy. Stagg et al. proved that the anti-4-1BB mAb significantly improves the anticancer effect of anti-HER2/neu mAb in breast cancer cell lines [9]. A concordant experiment was performed in pancreatic cancer cell lines [12]. Our study is significant in that it extends the work of Park et al. and Stagg et al., suggesting a strategy to optimize the immune memory response of anti-HER2/neu with anti-4-1BB.
Adjuvant anti-HER2/neu therapy has brought substantial improvement of overall survival in HER2-positive breast cancer. Following the well-known HERA (BIG 1–01) trial, adjuvant anti-HER2/neu therapy has been widely accepted as a standard therapy for HER2-positive breast cancer [5]. Nevertheless, approximately 20%–30% of treated patients still experience late recurrence. Besides improving the anticancer effect of anti-HER2/neu mAb, we assumed that combined treatment with anti-4-1BB mAb could also assure the late immune memory of anti-HER2/neu mAb treatment and may aid in protecting HER2-positive breast cancer patients from late recurrence. First, we anticipated that combination therapy with anti-HER2/neu mAb and anti-4-1BB mAb would incorporate stronger immune memory along with stronger ADCC. Indeed, our experiment showed improved ADCC activation, consistent with the results of previous studies [9, 12]. However, an unexpected result was that the combination therapy that induced stronger antitumor efficacy also produced a deteriorated immune memory. TUBO cells or a mixture of TUBO and TUBO-P2J cells that were more successfully responsive to the combination therapy were more vulnerable to rechallenge with cancer cells than those initially treated with a single therapy of anti-HER2/neu mAb or anti-4-1BB mAb. This was contradictory to the usual belief that successful immune activation usually leads to the generation of superior immune memory.
When the adaptive immunity induced by anti-HER2/neu therapy was first revealed, CD8+ T cells were suspected to be responsible for the development of immune memory following therapy [3]. This was proven by the recurrence of previously anti-HER2/neu-treated TUBO cell tumors in CD8+-depleted BALB/c mice. We initially hypothesized that anti-4-1BB added to anti-HER2/neu therapy would interfere with the immune cells responsible for adaptive immunity. This was supported by our immunoassay data showing a decrease in the proportion of CD44+ CD8+ cells after anti-4-1BB and anti-HER2 combination therapy amongst the global increase in immune cells. Memory CD8+ T cells can be differentiated from naive CD8+ T cells by the increased expression of adhesion molecules, such as CD44 [13]. This raised the possibility that anti-4-1BB addition may induce additive ADCC; however, it could not evoke the immune memory function of CD8+ T cells. Therefore, clarifying the mechanism of this phenomenon and solving this barrier would be important for utilizing anti-4-1BB and anti-HER2/neu mAb combination in cancer treatment.
Our data showed that activation of CD8+ T cells by cancer cells is crucial in developing adaptive immune memory after anti-4-1BB mAb treatment. The initiation of adaptive immunity occurs more slowly than innate immunity [27]. Induction of a response from CD8+ T cells countering an antigen is known as T cell priming and generally takes place in lymphoid tissues [28]. After the priming phase, CD8+ T cells are activated to memory CD8+ T cells or to effector cytotoxic T lymphocytes [29]. In our experiment, the naive CD8+ T cells of anti-4-1BB mAb-treated mice were not significantly increased by rechallenge with OVA emulsified in IFA and could not produce immune memory. We speculated that the administration of anti-4-1BB mAb would affect the memory function of CD8+ T cells during the priming step, but in practical settings, the method to protect only the priming stage from anti-4-1BB mAb administration would be challenging to actualize.
The potential suggestion for a breakthrough strategy against the loss of adaptive immunity after a stronger ADCC with a combination of anti-4-1BB mAb could be dose optimization. When the dose of anti-4-1BB mAb was tapered to 1 mg/kg, immune memory was significantly induced. Another theoretical method might be targeting the specific application time of anti-41BB to only target activated CD8+ T cells. Nevertheless, this would be challenging to accomplish clinically in the real world, and our proposal for dose optimization would be more applicable. The exhaustion describes a condition of T cell dysfunction and CD8+ TILs that upregulate PD1 expression indicate an exhausted phenotype [30,31,32]. The expression of PD1 in CD8+ T cells was restored 10 mg/kg of anti-4-1BB mAb. Therefore, it will be necessary to investigate the effect on PD1 inhibition, as preventing T cell exhaustion maybe the key to resolving the immune memory damage caused by high concentration of 4-1BB mAb. Hence, we carefully suggest future clinical trials testing anti-4-1BB mAb with anti-HER2/neu mAb to optimize the dose of anti-4-1BB mAb by starting from a lower dose. Thus, trials are more likely to achieve favorable results. Two anti-41BB mAbs have been tested in the clinical setting: urelumab (BMS-663513) and utolimumab (PF-05082566). Urelumab is a fully human IgG4-based anti-CD137 mAb that does not block CD137L–CD137 interactions and has a high agonist activity but exhibits liver toxicity at dosages higher than 1 mg/kg. Utolimumab, a ligand-blocking-humanized IgG1 mAb has weaker agonistic activity but does not have dose-limiting toxicities. Ongoing trials (NCT03364348 and NCT03414658) of anti-4-1BB mAb testing combinational strategies with anti-HER2/neu mAb were designed using utolimumab [33]. Further investigation is warranted for the practical use of anti-4-1BB and anti-HER2/neu mAbs, and taking our study into account, careful dosage optimization may be required to achieve one-step closure for successful clinical adaptation.
A challenge left for our study is that it could not be clarified that the mechanism of dose optimization of anti-4-1BB is able to protect against adaptive immunity. Notwithstanding the success of determining the optimal dosage of anti-4-1BB as a combination with anti-HER2/neu mAb, the challenge remains to unveil and understand the underlying mechanism. In addition, the fundamental weakness of murine study models remains, and future analysis in clinical settings is required. Nonetheless, our study explores the anticancer potential of anti-HER2/neu and anti-4-1BB mAb combination therapy in breast cancer. In addition, this study is significant in raising awareness of the hurdles to effective therapy caused by the acquisition of adaptive immunity, which is critical in fighting against the late recurrence of cancer. Finally, we demonstrated a breakthrough method that preserves immune memory by dose optimization of anti-4-1BB mAb.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Hudis CA (2007) Trastuzumab–mechanism of action and use in clinical practice. N Engl J Med 357(1):39–51
Clynes RA et al (2000) Inhibitory Fc receptors modulate in vivo cytotoxicity against tumor targets. Nat Med 6(4):443–446
Park S et al (2010) The therapeutic effect of anti-HER2/neu antibody depends on both innate and adaptive immunity. Cancer Cell 18(2):160–170
Cameron D et al (2017) 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet 389(10075):1195–1205
Watts TH (2005) TNF/TNFR family members in costimulation of T cell responses. Annu Rev Immunol 23:23–68
Melero I et al (1997) Monoclonal antibodies against the 4–1BB T-cell activation molecule eradicate established tumors. Nat Med 3(6):682–685
Takahashi C et al (1999) Cutting edge: 4–1BB is a bona fide CD8 T cell survival signal. J Immunol 162(9):5037–5040
Stagg J et al (2011) Anti-ErbB-2 mAb therapy requires type I and II interferons and synergizes with anti-PD-1 or anti-CD137 mAb therapy. Proc Natl Acad Sci USA 108(17):7142–7147
Song H et al (2014) Intratumoral heterogeneity impacts the response to anti-neu antibody therapy. BMC Cancer 14:647
Kang SW et al (2017) Anti-CD137 Suppresses Tumor Growth by Blocking Reverse Signaling by CD137 Ligand. Cancer Res 77(21):5989–6000
Masu T et al (2018) Anti-CD137 monoclonal antibody enhances trastuzumab-induced, natural killer cell-mediated cytotoxicity against pancreatic cancer cell lines with low human epidermal growth factor-like receptor 2 expression. PLoS ONE 13(12):e0200664
Sallusto F et al (1999) Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401(6754):708–712
Moasser MM (2007) Targeting the function of the HER2 oncogene in human cancer therapeutics. Oncogene 26(46):6577–6592
Kiessling R et al (2002) Cellular immunity to the Her-2/neu protooncogene. Adv Cancer Res 85:101–144
Le XF et al (2005) Genes affecting the cell cycle, growth, maintenance, and drug sensitivity are preferentially regulated by anti-HER2 antibody through phosphatidylinositol 3-kinase-AKT signaling. J Biol Chem 280(3):2092–2104
Mittendorf EA et al (2010) A novel interaction between HER2/neu and cyclin E in breast cancer. Oncogene 29(27):3896–3907
Pegram M et al (1999) Inhibitory effects of combinations of HER-2/neu antibody and chemotherapeutic agents used for treatment of human breast cancers. Oncogene 18(13):2241–2251
Clynes RA et al (2000) Inhibitory Fc receptors modulate in vivo cytoxicity against tumor targets. Nat Med 6(4):443–446
Musolino A et al (2008) Immunoglobulin G fragment C receptor polymorphisms and clinical efficacy of trastuzumab-based therapy in patients with HER-2/neu-positive metastatic breast cancer. J Clin Oncol 26(11):1789–1796
Arnould L et al (2006) Trastuzumab-based treatment of HER2-positive breast cancer: an antibody-dependent cellular cytotoxicity mechanism? Br J Cancer 94(2):259–267
Varchetta S et al (2007) Elements related to heterogeneity of antibody-dependent cell cytotoxicity in patients under trastuzumab therapy for primary operable breast cancer overexpressing Her2. Cancer Res 67(24):11991–11999
Gennari R et al (2004) Pilot study of the mechanism of action of preoperative trastuzumab in patients with primary operable breast tumors overexpressing HER2. Clin Cancer Res 10(17):5650–5655
Ladjemi MZ et al (2010) Anti-HER2 vaccines: new prospects for breast cancer therapy. Cancer Immunol Immunother 59(9):1295–1312
Wang W et al (2015) NK cell-mediated antibody-dependent cellular cytotoxicity in cancer immunotherapy. Front Immunol 6:368
Chester C et al (2016) 4–1BB agonism: adding the accelerator to cancer immunotherapy. Cancer Immunol Immunother 65(10):1243–1248
Dranoff G (2004) Cytokines in cancer pathogenesis and cancer therapy. Nat Rev Cancer 4(1):11–22
Topalian SL et al (2016) Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat Rev Cancer 16(5):275–287
Farhood B et al (2019) CD8(+) cytotoxic T lymphocytes in cancer immunotherapy: A review. J Cell Physiol 234(6):8509–8521
Etxeberria I et al (2020) New emerging targets in cancer immunotherapy: CD137/4–1BB costimulatory axis. ESMO Open 4(Suppl 3):e000733
Ahmadzadeh M et al (2009) (2009) Tumor antigen-specific CD8 T cells infiltrating the tumor express high levels of PD-1 and are functionally impaired. Blood 114(8):1537–1544
Miller BC et al (2019) Subsets of exhausted CD8(þ) T cells differentially mediate tumor control and respond to checkpoint blockade. Nat Immunol 20(3):326–336
Paley MA et al (2012) Progenitor and terminal subsets of CD8þ T cells cooperate to contain chronic viral infection. Science 338(6111):1220–1225
Krasniqi E et al (2019) Immunotherapy in HER2-positive breast cancer: state of the art and future perspectives. J Hematol Oncol 12(1):111
Funding
This work was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) of Korea funded by the Korean Government (MSIT) Under Grant (No.2019M3A9H1103607); Under Grant (No.2017R1C1B5076247); Under Grant (No.2016R1D1A1B03935426); and the SAMJINPHARM.CO., LTD Under Grant (SJ-IIT-17-07).
Author information
Authors and Affiliations
Contributions
HYK, J-HC and SGP conceptualized the study and reviewed the writing of the manuscript. HYK, J-HC and MMH wrote the original draft of the manuscript and analyzed the data. JHP, I-HK and BKC investigated the immune cell population and activity. AL and SGP were involved in supervision, funding acquisition and project administration.
Corresponding authors
Ethics declarations
Conflict of interest
The researcher claims no conflicts of interest.
Ethics approval and consent to participate
The experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee of Inje University (2019-002).
Consent for publication
I would like to declare that the manuscript is approved by all authors for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.Y., Choi, JH., Haque, M.M. et al. Combined treatment with anti-HER2/neu and anti-4-1BB monoclonal antibodies induces a synergistic antitumor effect but requires dose optimization to maintain immune memory for protection from lethal rechallenge. Cancer Immunol Immunother 71, 967–978 (2022). https://doi.org/10.1007/s00262-021-03120-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-021-03120-1