Abstract
The solid tumor microenvironment is replete with factors that present a stress to infiltrating immune cells. Endoplasmic reticulum (ER) stress sensor PKR-like ER kinase (PERK) is primed to sense and respond to the burden of misfolded proteins in the ER lumen induced by cell stressors. PERK has documented roles as a master regulator of acute and chronic responses to cell stress as well as in the regulation of cell metabolism. Here, we provide an overview of the roles of PERK based on what is known and remains to be tested in immune cells in tumors and impacts on tumor control. PERK is one of several ER kinases able to preferentially induce activating transcription factor 4 (ATF4) as a response to cell stress. ATF4 orchestrates the oxidative stress response and governs amino acid metabolism. We discuss the tested role of ATF4 in tumor immunity and provide insight on the dueling protective and deleterious roles that ATF4 may play in the stress of solid tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
PERK is a stress-sensing kinase with roles in antitumor immunity
Mammalian cells regularly encounter exogenous cell stress such as nutrient and amino acid deprivation, hypoxia, and reactive oxygen species (ROS). Such cell stressors lead to a burden of misfolded proteins in the endoplasmic reticulum (ER) lumen that engage ER stress sensors to trigger the integrated stress response (ISR) in an attempt to return the cell to homeostatic conditions [1, 2]. Three stress sensors; inositol-requiring enzyme-1α (IRE1α), activating transcription factor 6 (ATF6), and PKR-like ER kinase (PERK) are activated by the unfolded protein response (UPR) [3,4,5]. Each of the aforementioned sensors lead to the activation of the regulatory transcription factors XBP1, ATF6p50, and activating transcription factor 4 (ATF4), respectively [6, 7]. The transcriptional programs induced by ER stress and the UPR lead to increased expression of genes required for protein folding, the inhibition of new protein synthesis through regulated IRE1-dependent mRNA decay (RIDD) and the induction of autophagy programs that help to eliminate unfolded proteins in the ER [8, 9].
A key step in activation of the UPR is the direct inhibition of protein translation following PERK activation. Sensing of a burden of unfolded/misfolded proteins catalyzes the chaperone protein Bip/GRP78 to dissociate from binding the luminal domain of PERK enabling activation of PERK through dimerization and autophosphorylation [5]. Activated PERK inhibits eukaryotic translation initiation factor 2α (eIF2α) through phosphorylation on serine residue 51 which prevents the formation of Met-tRNAiMet complexes and prohibits initiation of translation of cap-dependent mRNAs [10]. Following this discovery, eIF2α was shown to be required for cell survival and organism viability in response to unfolded protein accumulation in the ER. Mice bearing homozygous serine to alanine mutations at residue 51 of eIF2α die shortly after birth due to hypoglycemia and defects in the gluconeogenesis pathway [11]. The kinases PERK and general control nonderepressible 2 (GCN2) were found to play a central role in this process and were required for gluconeogenesis to take place due to their roles in phosphorylating eIF2α. In addition to temporarily restricting protein synthesis as a protective mechanism to the cell, PERK subsequently allows for resumption of protein synthesis after ER stress through a mechanism involving the stimulation of the protein growth arrest and DNA damage-inducible protein, GADD34 [12, 13]. GADD34 is a phosphatase that dephosphorylates p-eIF2α in a PERK-dependent manner, highlighting an important negative feedback loop of the stress response.
The acute role of PERK–p-eIF2α to inhibit protein translation in antitumor immunity remains elusive. Activation of the stress response is intimately connected to T cell differentiation. Primed T helper 2 (Th2) cells exhibit enhanced p-eIF2α and increased features of the ISR. Upon restimulation, Th2 cells exhibit dephosphorylation of p-eIF2α followed by cytokine secretion and cycloheximide treatment extinguished the effect, tying regulation of protein translation to T cell function [14]. We were the first group to show that effector CD8 T cells exposed to the tumor microenvironment (TME) or in tumors experience inhibition of protein synthesis that is associated with poor tumor control [15] but the role of PERK–p-eIF2α to orchestrate this process remains untested and the role of PERK in antitumor immunity is ill-defined. The TME is replete with elements such as lactic acid and ROS that likely present an acute stress to tumor infiltrating T cells (TILs) [16, 17]. However, it was demonstrated that mice with conditional deletion of PERK in the T cell compartment experience superior tumor control of B16 melanomas relative to WT counterparts [18] and we found that PERK-deficient T cells confer powerful tumor control in the adoptive cellular therapy setting [19]. In both instances, the deleterious role of PERK in antitumor immunity was attributed to activation of the chronic arm of the stress response. In contrast to the acutely protective role of PERK–p-eIF2α, a persistent burden of unfolded/misfolded proteins in the ER lumen induces the chronic stress response comprised of ATF4/C/EBP homologous protein (CHOP) and ER oxidoreductase 1α (ERO1α) activity that can induce cell death [20, 21].
In line with PERK’s role to restrict protein translation as a means to protect cells from ER stress, PERK mediates cell cycle. Cell cycle progression is tightly controlled by the temporal expression of cyclins and cyclin-dependent kinases (CDKs) [22]. In cancer immunotherapy, cell cycle inhibitors have been combined with checkpoint therapies and have shown tremendous promise as a treatment modality for cancer patients. The effect occurs by enhancing cytotoxic T cell function toward tumor clearance and by suppression of regulatory T cells [23]. In a breast cancer model, the CDK4/CDK6 inhibitor Abemaciclib led to synergy when administered in combination with programmed death ligand 1 (PD-L1) checkpoint blockade, enabling tumor clearance and development of long-lived memory T cells [24]. We found that anti-programmed cell death protein 1 (a-PD-1) therapy combined with PERK inhibition resulted in complete and durable tumor responses in a mouse model of sarcoma [19]. Following ER stress, activation of PERK results in the loss of cyclin D1 and subsequent cell cycle arrest. Brewer et al. demonstrated that inhibition of PERK-induced p-eIF2α restricted accumulation of cyclin D1; whereas, overexpression of PERK blocked cyclin D1 expression [25]. Loss of PERK kinase activity abrogated the aforementioned effect, directly implicating PERK’s role in phosphorylation as central to regulation of cell cycle arrest [25]. Thereafter, it was discovered that ER stress and activation of PERK also led to the induction of p53 and cell cycle arrest through multiple mechanisms [26, 27]. Based on the robust known roles of PERK to orchestrate elements of biology that are proving to be cornerstones of successful cancer immunotherapy, study of regulation by the ER kinase in tumor immunity is prudent.
Potential impacts of PERK on antitumor metabolism and immunity
Cell stress is intimately linked to bioenergetics. The potential impact of the stress response to program cell metabolism as a reaction to the stress of the TME could present a unifying target to the cancer immunotherapy field. The metabolism of T cells is closely linked to their environment. T cells within the TME of solid tumors face unique stresses that impact their metabolic profiles. In the TME, T cells must overcome cell stressors that negatively impact their metabolism and subsequent function such as hypoxia, high lactate, glucose deprivation, and competition for nutrients [28]. In addition to hypoxia and nutrient deprivation, chronic antigen exposure can lead to exhausted T cell phenotypes with impaired mitochondrial function [29]. Scharping et al. demonstrated that T cells infiltrating murine and human tumors exhibited depletion of mitochondrial biomass and impaired oxidative phosphorylation (OXPHOS) due to loss of PPARG coactivator 1α (PGC1α) expression. PGC1α is a key regulator of mitochondrial biogenesis and forced PGC1α expression restored biomass and improved T cell antitumor function [30]. While suppression of OXPHOS in the TME limits T cell function, general competition for nutrients between tumor and T cells dramatically impacts T cell function. As a consequence of enhanced glycolysis within antigenic solid tumors, restriction of glucose access to effector cells within solid tumors leads to T cell dysfunction [31]. Based on the projected protective role of PERK–p-eIF2α in T cells exposed to the stress of tumors it is surprising that PERK-deficient T cells appear to control tumor growth better than littermate controls [18, 19] and the data suggest that the specific metabolic role of PERK in T cells in tumors needs to be elucidated.
Given the competition for glucose that persists in the TME, reprogramming T cell metabolism away from glucose dependence has proven efficacious to promote tumor control and a metabolic shift is accompanied by a change in lineage fate [32, 33]. It is established that T cells that exhibit potent antitumor function display both proficient effector function and the capacity to persist as long-lived memory cells. Enhanced spare respiratory capacity (SRC) and OXPHOS are metabolic traits associated with memory T cells and expression of the enzyme carnitine palmitoyltransferase (Cpt1a) that catalyzes β-oxidation of fatty acids (FAO) generates such traits resulting in T cells with productive tumor control [34]. Reprogramming T cells through transient glucose restriction enables heightened glycolytic capacity measured by increased extracellular acidification rates in response to glucose and oligomycin treatments. The enhanced glycolytic capacity endowed by transient glucose deprivation leads to superior antitumor function of T cells infused into solid tumors [35]. Acute nutrient deprivation such as transient glucose restriction may allow reprogramming of antitumor immunity that ensures T cells can resist the metabolic stress of the TME. For example, inhibition of glycolysis was previously shown to reprogram T cells to depend on FAO that supports antitumor immunity through a robust store of mitochondrial ATP associated with increased effector function in tumors and prolonged survival [32]. Given that acute glucose deprivation increased the capacity for antitumor cytokine secretion [35], it is possible that metabolic conditioning reshapes the ISR that was previously shown to be integral for cytokine secretion upon restimulation [14].
Recent literature contests the importance of FAO for memory T cell development [36] and other metabolic programs are essential to program superior antitumor immunity. Of critical importance, the pathways that regulate glycogen synthesis (glycogenesis) and breakdown (glycogenesis) impact T cell differentiation and function. Ma et al. found that gene deletion and pharmacological inhibition of gluconeogenesis enzyme phosphoenolpyruvate carboxykinase 1 (PCK1) impaired memory T cell development and damaged tumor control [37]. Inhibition of glycogenolysis enzyme glycogen phosphorylase proved critical for memory T cell development in vivo and in vitro, propelling the breakdown of glycogen to the forefront of T cell lineage fate. T cells deficient in gluconeogenesis or impaired in glycogenolysis were unable to control tumor growth and could not retain in vivo development to memory [37]. In our 2019 study, we found that T cells devoid of PERK exhibited memory T cell metabolic traits such as enhanced oxidative metabolism, elevated SRC, and reduced accumulation of ROS in mitochondria [19]. Gene array data of the UPR between cytokine conditioned effector and memory-like T cells in vitro yielded the finding that the PERK axis consisting of Atf4, Ddit3 (Chop), and Ero1l was the sole UPR axis upregulated in cytokine-conditioned effector T cells relative to memory-like cells [38] and proteomic analysis of these populations confirmed these results [15]. These data suggest a potential role of the stress response in T cell immunometabolism and lineage fate.
Though it is established that T cells with memory-like bioenergetics promote superior tumor control, it is not understood whether alternative metabolism enables stress resistance in the TME. The energy sensor mammalian target of rapamycin (mTOR) guides energy production in nutrient replete conditions through glycolysis. mTORC1 and mTORC2 play distinct roles in influencing CD8 T cell differentiation to effector and memory phenotypes. Forced mTORC1 activation enhances glycolytic metabolism and effector maturation generating better antitumor immunity as a result of hyper effector function [39]. Genetic ablation of mTORC1 activation reduced effector T cell function, but retained memory characteristics. Tumor control was lost due to abrogation of effector function. Alternatively, deletion of mTORC2 led to metabolic changes that promoted both memory and effector T cell traits, but antitumor immunity was not tested [39]. PERK exhibits lipid kinase activity acting on the substrate diacylglyceride (DAG), which produces phosphatidic acid and leads to mTOR activation [40]. The concept has not been tested, but PERK-mediated control of mTOR could explain memory-like metabolic traits in PERK−/− T cells (Fig. 1). In contrast to mTOR signaling in nutrient-rich conditions, AMPK is a metabolic energy sensor that responds to nutrient stress [41]. The role of AMPK has not been widely studied in tumor immunity, but several papers showed that pharmacological stimulation of AMPK promotes tumor control [15, 42]. The data suggest that priming an energy sensor designed to control cell function under stress supports antitumor function. Collectively, these findings highlight the unique potential to modulate the ER stress response and UPR to influence metabolic programs and cell fate decisions in T cell-based immunotherapy.
Metabolic avenues of PERK activity. In response to ER stress, the stress-sensing kinase PERK phosphorylates the transcription initiation factor eIF2α to prevent cell cycle progression through loss of cyclin D1, canonical protein translation, and prohibit generation of the active nuclear form SREBP1 (SREBP1c) that induces lipogenesis. Additionally, PERK phosphorylates diacylglyceride (DAG) resulting in the production of phosphatidic acid (PA), and subsequent activation of mTOR signaling
In nutrient-rich conditions, mTORC1 promotes lipid storage through activation of the transcription factor sterol regulatory element binding protein 1 (SREBP1) [43]. Inhibition of mTOR with Rapamycin prevented nuclear accumulation of SREBP1, and RNA silencing of SREBP1 blocked lipogenesis and impaired increases in cell size. The effects were shown to be dependent on Akt [43]. In the context of tumor immunity, Akt is deleterious to antitumor T cells based on hindrance of FAO metabolism and memory T cell formation [33]. Together, the mTOR/Akt axis that regulates SREBP1 appears to be important for T cell-mediated tumor control though the effects need to be further elucidated in the endogenous settings. While PERK has been shown to regulate mTOR, PERK is also required for SREBP1 activation. Gene deletion of PERK in mammary epithelial cells leads to loss of cleaved SREBP1 (SREBP1c), the active nuclear form of SREBP1. The effect was shown to be dependent on p-eIF2α and resulted in abrogation of key lipogenic enzymes, thus deletion of PERK in mouse embryonic fibroblasts (MEFs) led to impaired differentiation into adipocytes [44]. The data highlight the importance of the PERK–SREBP1 axis in lipid metabolism. A consequence of SREBP1 activation is the induction of fatty acid synthesis (FAS) [45], a process that cannot occur simultaneously to FAO. While mTOR/Akt and PERK activate FAS through regulation of SREBP1, under nutrient stress AMPK directly phosphorylates and inhibits SREBP1 [46] to restrict FAS and promote FAO [47]. Collectively, these data suggest that PERK activity in response to cell stress contains the unique capacity to program master regulators of antitumor metabolism.
ATF4 is a stress-induced transcription factor with potential roles in antitumor immunity
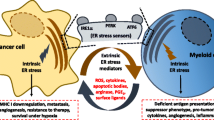
While PERK has intrinsic kinase activity that allows for regulation of multiple metabolic players, PERK-mediated phosphorylation of eIF2α has potent consequences for cell biology and fate. PERK phosphorylation of eIF2α results in the selective translation of the transcription factor ATF4 [6]. In this way, ATF4 acts as a critical downstream effector of the PERK arm of the UPR to induce expression of genes involved in processes crucial to the ISR, such as amino acid metabolism and the oxidative stress response [48]. Globally, phosphorylation of eIF2α is a key process in numerous stress-signaling pathways as the post-translational modification can be catalyzed through multiple stress-induced kinases that include (1) PERK, in response to ER stress [21, 49, 50], (2) GCN2, in response to amino acid deprivation [51, 52], (3) heme-regulated inhibitor (HRI) responding to oxidative stress [53] or (4) protein kinase RNA-activated (PKR), in the face of stress response to viral infection [54]. Upon phosphorylation of eIF2α by one of the aforementioned stress kinases, global protein synthesis is suppressed to temporarily alleviate ER, amino acid, oxidative, or viral stressors [6, 55]. Thus, ATF4 activation induced by p-EIF2α is a converging point for multiple ER kinases responding to diverse cell stressors [21, 48, 55, 56] that ensures the capacity to tune cell survival in the face of acute stress [48] and to induce cell death in response to a burden of persistent/chronic misfolded proteins (Fig. 2) [20]. In the context of antitumor immunity, it is likely that differential TME conditions engage the unique ER kinases that unilaterally converge on ATF4. Treatment with ovarian cancer ascites induces phosphorylation of PERK in CD8 T cells, indicating that the TME alone generates unfolded protein stress that activates the PERK response [18]. We found that the TME restricts protein synthesis in T cells in tumors, suggesting that a critical downstream function of the stress response mediated by p-eIF2α may be enacted to thwart antitumor immunity [15]. Multiple studies have shown that ROS secreted by tumor cells in the TME suppress T cell activation and infiltration to tumors [57, 58]. Though activation of HRI in T cells by TME ROS has yet to be tested, it is plausible that the stress kinase could play a role in controlling antitumor outcomes. Finally, in murine gliomas T cell-specific GCN2 was required for proliferation and function in tumors [59], suggesting activation of another stress kinase pathway that leads to induction of ATF4.
ATF4 is a converging point for cell stress pathways. The induction of ER stress kinases PERK, HRI, GCN2 or PKR through the URP, oxidative stress, nutrient deprivation or viral stress, respectively, results in the phosphorylation of eIF2α. To temporarily alleviate cell stress p-eIF2α suppresses global protein translation while access to ATF4 mRNA is increased. Under acute oxidative stress, ATF4 serves a protective role by increasing GSH production resulting in a decrease in ROS and ultimately promoting cell survival. Conversely, when faced with persistent cell stress, ATF4 cooperatively binds with CHOP. Together the two transcription factors act upon genes that increase protein translation that leads to indirect cell death through generation of ROS
ATF4 is a basic leucine-zipper (bZIP) class transcription factor that drives the expression of genes involved in multiple metabolic pathways. ATF4 has been shown to enhance metabolic processes such as glycolysis, glutaminolysis, and OXPHOS by regulating a network of genes controlling amino acid intake, mTORC1 activation, and protein translation [60, 61]. To regulate target gene expression ATF4 forms transcription factor complexes by binding DNA and other transcription factors. ATF4 binds to DNA at CREs (cAMP responsive elements) or C/EBP-ATF response elements (CAREs) [62, 63]. In addition to binding DNA, ATF4 forms transcription factor complexes to collectively regulate target gene expression. Alone, AFT4 homodimers are unstable, and stability must be increased to effectively regulate gene expression. Increasing stability is accomplished when ATF4 forms heterodimers with other transcription factors such as FOS/JUN or CHOP [48, 62,63,64]. Together, FOS and JUN regulate genes known to protect cells from apoptosis [65,66,67], while ATF4 and CHOP synergize to increase protein synthesis, in turn accumulating ROS and leading to cell death (Fig. 2) [20]. As indicated above, the role of ATF4 varies greatly and whether ATF4 acts in a protective or deleterious manner is determined by several variables, including its relationship with binding partners.
Antioxidant defense is a well-studied acute role of ATF4. ATF4 regulates the expression of genes involved in protection from oxidative stress such as those involved in the biosynthesis of glutathione (GSH), a key component for reducing endogenous peroxides [21]. For example, endogenous peroxides in Atf4−/− MEF cells are elevated relative to WT levels [21] and Atf4−/− MEFs experience elevated cell death. Treatment of Atf4−/− MEFs with reducing agents sustains cell survival, indicative of intrinsic ROS that promote cell death in the absence of ATF4 [21]. Along these lines, in Hepa1-6 cells, mRNA levels of Cth, a critical gene in the GSH pathway, and Sod2, a gene involved in clearing ROS from the mitochondria, are reduced in the absence of ATF4 leading to increased cell death [68]. Of note, Sod2 was determined to be a gene associated with better tumor control in T cells selected for low mitochondrial membrane potential [69]. In vivo ATF4 is required for protecting cells from oxidative stress. Mice with liver-specific ATF4 deletion exhibit increased cell death and heightened levels of malondialdehyde, a highly reactive compound that serves as a marker for oxidative stress [68]. Together, the studies suggest that ATF4 is critical for cellular protection from oxidative stress.
While ATF4 acutely protects cells from oxidative stress, in the face of chronic stress the induction of ATF4 promotes cell death through accumulation of intracellular ROS [20]. ATF4 binds with CHOP and RNA-seq of genes targeted by these transcription factors suggests that together they direct deleterious protein synthesis and the UPR [20]. In vitro and in vivo studies found that together the two transcription factors induce cell death. Forced expression of CHOP did not reduce MEF viability but forced expression of ATF4 promoted low levels of death. When ATF4 and CHOP were co-expressed in MEFs, apoptosis was increased beyond ATF4 expression alone [20]. In vivo results amplified the in vitro findings as adenovirus-mediated overexpression of ATF4 and CHOP in the liver of mice proved that ATF4/CHOP led to cell death [20]. ERO1α is an oxidoreductase enzyme that catalyzes protein folding in the ER lumen. Both in vivo and in vitro, ATF4- and CHOP-dependent cell autonomous apoptosis was attributed to an increase in protein synthesis that led to ERO1α-mediated generation of ROS that was the direct mechanism to promote cell death [20].
Regarding global tumor immunity, it has been shown that the suppressive nature of myeloid-derived suppressor cells (MDSCs) is catalyzed by the oxidative stress of the TME and alleviation of MDSC-intrinsic ATF4-CHOP response allays their protumorigenic nature [70]. These data indicate that ATF4-CHOP plays a deleterious role in the immune response to promote tumor growth. In multiple studies that established a detrimental role for PERK in tumor control [18, 38], the antitumor efficacy of PERK−/− T cells was attributed to abrogation of the chronic arm of the stress response. The oxidative stress of the TME was found to enhance PERK–ATF4–CHOP in CD8 TILs and led to inhibition of antitumor capability in a CHOP-dependent manner [18]. We demonstrated that the ATF4–CHOP–ERO1α axis is significantly increased in effector T cells relative to memory-like T cells [15, 19, 38]. These data suggest that ATF4 could have a contribution to T cell lineage fate and play a defining role in antitumor immunity. In CD4 T cells, the oxidative stress response activates ATF4 to promote redox homeostasis, proliferation, and cytokine production [61]. These data point to a protective role of ATF4 in CD4 T cells. It is likely that ATF4’s role in the face of acute stress is protective to antitumor immunity through buffering antioxidant capacity. In contrast, chronic activation and expression of ATF4 likely has a deleterious role in antitumor immunity through ATF4’s hyperactivating role in concert with CHOP that drives protein translation that results in cell death through generation of intrinsic cell ROS [20].
Taken together a picture has emerged in T cell biology of a delicate balance for intracellular ROS, likely moderated by the stress response, as a positive regulator of cell growth and signaling contrasted to accumulation of pathological levels of ROS that trigger death. A seminal paper by Sena et al. determined that ROS generated by mitochondria (mitoROS) are required for nuclear factor of activated T cells (NFAT) activation and IL-2 production as well as antigen-specific inflammatory responses in CD4 T cell in vivo [71]. Along these lines, CD8 T cells proliferating in tumor-draining lymph nodes of mice treated with a-PD-L1 therapy expressed elevated mitoROS relative to T cells with diminished proliferation and pharmacological promotion of ROS-activated responses to a-PD-L1 therapy in tumor-bearing mice [72]. We discovered that PD-1 CD8 TILs in mice and patients bearing sarcomas are replete with mitoROS, but mitoROShigh T cells exhibit reduced SRC, diminished IFN-γ production, and signs of early cell death [19]. Together the data illustrate the necessity for mitoROS generation in T cells for successful immunotherapy, but suggest that a constant cycle of ROS detoxification must also take place. GSH is a key mediator of antioxidant capability in T cells necessary for mitoROS detoxification. GSH was shown to be critical to support NFAT activation and subsequent metabolic reprogramming needed for T cell antiviral defense [73]. In successful antitumor T cells enriched for gluconeogenesis, the cycle was critical to produce NADPH to reduce oxidized glutathione (GSSG) back to GSH. Inhibition of gluconeogenesis through multiple substrates diminished NADPH/NADP+ ratios leading to accumulation of GSSG and elevated intracellular ROS [37]. The data show the essential role of GSH to detoxify cell ROS to support antitumor T cells.
ATF4 and amino acid stress in tumor immunity
A common stress presented to immune cells in the TME is deficiency of amino acids and ATF4 is likely central to the stress response of antitumor TILs. Amino acids are precursors for protein and nucleic acid synthesis [74] and the metabolic shift that occurs in response to T cell activation requires robust increases in amino acid intake and production for effector function and development of memory [74, 75]. A seminal paper by Harding et al. identified the essential role of ATF4 in transcribing genes necessary for import of amino acids. Under cell stress induced by ER stress enhancer tunicamycin ATF4−/− MEFs were unable to generate amino acids, glycine transporter 1 (Glyt), and Asparagine Synthetase (ASNS), an enzyme that catalyzes the biosynthesis of asparagine and glutamate from aspartate and glutamine, respectively. Thus, ATF4−/− MEFs were unable to proliferate in the absence of non-essential amino acids (NEAA), indicating an intrinsic defect in NEAA production [21]. In CD4 T cells, oxidizing environments and amino acid deprivation were shown to induce ATF4 expression that subsequently was imperative for activation of mTORC1 and synthesis of amino acids. Based on deficiency of mTORC1 in ATF4−/− CD4 T cells, ATF4 was required to generate glycolysis, OXPHOS, and effector function in CD4 T cells [61]. The intrinsic role of ATF4 in antitumor TILs remains to be elucidated.
GCN2 is the ER stress sensor primed to sense and respond amino acid stress by binding uncharged tRNAs [76, 77]. Upon amino acid starvation, GCN2 phosphorylates eIF2α and enables the increased translation of ATF4. This event serves as the converging point between nutrient stress and ATF4 signaling [61, 78]. A seminal paper by Munn et al. indicated that GCN2 acts as a sensor enabling T cells to detect and react to amino acid deprivation in their environment. Dendritic cell (DC) expression of indoleamine 2,3 dioxygenase (IDO), an enzyme that degrades the essential amino acid tryptophan, induced GCN2-mediated stress sensing and response in T cells. GCN2-deficient antigen-specific CD8 T cells primed in the presence of IDO-producing plasmacytoid DCs (pDCs) exhibited enhanced proliferation relative to WT controls. The effect in WT T cells was rescued by administration of tryptophan or inhibition of IDO, leading to the conclusion that GCN2 senses tryptophan deprivation causing inhibition of T cell proliferation [79]. The findings were later challenged by the demonstration that GCN2−/− T cells failed to proliferate in the presence of IDO or low tryptophan by employing a titration assay to determine the limiting amount of tryptophan required for cell proliferation. Of note, the latter study commented that limiting amounts of amino acids may impact the capacity of antigen presenting cells, thus potentially accounting for low proliferative activity of GCN2−/− T cells. However, in vivo a proliferation defect was also noted in GCN2-deficient T cells [77]. Together the data suggest that GCN2 impacts T cell proliferation and homeostasis.
Regarding tumor immunity, recent works established that GCN2 is required for proliferation, survival, and function of CD8 T cells in murine gliomas. In vitro, GCN2−/− T cells were less activated compared to WT counterparts. In GCN2−/− mice bearing glioblastoma, the number and percentage of CD8 T cells was significantly reduced in tumors, but no significant changes were noted in peripheral lymphoid organs [59]. These data indicate that the TME may be responsible for driving the reduction of CD8 T cells in tumor. Upon examination of the effects of amino acid deprivation on GCN2−/− T cells in vivo, WT T cells survived nutrient deplete conditions better than GCN2−/− T cells. Thus, GCN2 may be required for CD8 T cell survival in the TME, a plausible explanation for the reduction in CD8 T cells in gliomas [59].
GCN2 has also been proven critical for myeloid cells and their suppressive function in tumors. In mice with B16F10 melanomas, GCN2−/− myeloid cells generated reduced tumor volume relative to controls. Analysis suggested that tumors from mice harboring GCN2−/− myeloid cells produced tenfold less immunosuppressive IL-10 [80]. ATF4 is a critical downstream mediator of GCN2 and was shown to drive the immunosuppressive nature of MDSCs in a GCN2-dependent manner. Specifically, ATF4 activation did not occur in myeloid cells devoid of GCN2 and siRNA-mediated knockdown of ATF4 in macrophages in vivo resulted in decreased tumor growth. These data support reports that ATF4-CHOP axis promotes suppression in MDSC populations that enable tumor growth [70], and identify GCN2 as the potential upstream mediator to promote the protumorigenic effects.
Summary
The family of ER kinases that includes PERK, GCN2, HRI, and PKR primed to activate eIF2α and generate ATF4 expression, comprise a hub of stress sensors poised to respond to a variety of environmental insults. PERK and GCN2 have already been implicated in responding to stressors presented by the TME, but the specific acute and chronic responses imparted in pro- and antitumor immune populations remain poorly understood. It is important to note that the family of ER kinases represents a group of druggable targets that could serve to promote the efficacy of standard immune checkpoint blockade (ICB) therapies. We found that PERK inhibition with first-generation inhibitor GSK26064141 [81] generated complete responses in mice bearing sarcomas when combined with ICB therapy [19]. However, toxicity associated with pancreatic islet cell degradation is a concern for applications with first- and second-generation [82] inhibitors that directly target PERK. If PERK proves to tune T cell antitumor metabolism, it is possible that such therapies could be administered on a schedule that alleviates in vivo toxicity. Along these lines, non-toxic therapeutics that affect downstream targets of PERK are in development and could prove useful in the space of immune oncology. Integrated stress response inhibitor (ISRIB) is a small molecule that selectively inhibits p-eIF2α-mediated attenuation of translation [83, 84] downstream of PERK and early reports suggest that ISRIB treatment circumvents pancreatic toxicity [85] associated with targeting PERK. Given that the ER is a hub for cell metabolism and fate, study of master ER stress sensors to refine metabolic efficacy and tune stress relief in tumor immunity holds immense potential to generate novel therapeutic strategies to improve the efficacy of cancer immunotherapies.
References
Pakos-Zebrucka K, Koryga I, Mnich K, Ljujic M, Samali A, Gorman AM (2016) The integrated stress response. EMBO Rep 17(10):1374–1395. https://doi.org/10.15252/embr.201642195
Hetz C (2012) The unfolded protein response: controlling cell fate decisions under ER stress and beyond. Nat Rev Mol Cell Biol 13(2):89–102. https://doi.org/10.1038/nrm3270
Lee K, Tirasophon W, Shen X, Michalak M, Prywes R, Okada T, Yoshida H, Mori K, Kaufman RJ (2002) IRE1-mediated unconventional mRNA splicing and S2P-mediated ATF6 cleavage merge to regulate XBP1 in signaling the unfolded protein response. Genes Dev 16(4):452–466. https://doi.org/10.1101/gad.964702
Yamamoto K, Sato T, Matsui T, Sato M, Okada T, Yoshida H, Harada A, Mori K (2007) Transcriptional induction of mammalian ER quality control proteins is mediated by single or combined action of ATF6alpha and XBP1. Dev Cell 13(3):365–376. https://doi.org/10.1016/j.devcel.2007.07.018
Harding HP, Zhang Y, Ron D (1999) Protein translation and folding are coupled by an endoplasmic-reticulum-resident kinase. Nature 397(6716):271–274. https://doi.org/10.1038/16729
Harding HP, Novoa I, Zhang Y, Zeng H, Wek R, Schapira M, Ron D (2000) Regulated translation initiation controls stress-induced gene expression in mammalian cells. Mol Cell 6(5):1099–1108. https://doi.org/10.1016/s1097-2765(00)00108-8
Yoshida H, Matsui T, Yamamoto A, Okada T, Mori K (2001) XBP1 mRNA is induced by ATF6 and spliced by IRE1 in response to ER stress to produce a highly active transcription factor. Cell 107(7):881–891. https://doi.org/10.1016/s0092-8674(01)00611-0
Maurel M, Chevet E, Tavernier J, Gerlo S (2014) Getting RIDD of RNA: IRE1 in cell fate regulation. Trends Biochem Sci 39(5):245–254. https://doi.org/10.1016/j.tibs.2014.02.008
Kouroku Y, Fujita E, Tanida I, Ueno T, Isoai A, Kumagai H, Ogawa S, Kaufman RJ, Kominami E, Momoi T (2007) ER stress (PERK/eIF2alpha phosphorylation) mediates the polyglutamine-induced LC3 conversion, an essential step for autophagy formation. Cell Death Differ 14(2):230–239. https://doi.org/10.1038/sj.cdd.4401984
Krishnamoorthy T, Pavitt GD, Zhang F, Dever TE, Hinnebusch AG (2001) Tight binding of the phosphorylated alpha subunit of initiation factor 2 (eIF2alpha) to the regulatory subunits of guanine nucleotide exchange factor eIF2B is required for inhibition of translation initiation. Mol Cell Biol 21(15):5018–5030. https://doi.org/10.1128/mcb.21.15.5018-5030.2001
Scheuner D, Song B, McEwen E, Liu C, Laybutt R, Gillespie P, Saunders T, Bonner-Weir S, Kaufman RJ (2001) Translational control is required for the unfolded protein response and in vivo glucose homeostasis. Mol Cell 7(6):1165–1176. https://doi.org/10.1016/s1097-2765(01)00265-9
Kojima E, Takeuchi A, Haneda M, Yagi A, Hasegawa T, Yamaki K, Takeda K, Akira S, Shimokata K, Isobe K (2003) The function of GADD34 is a recovery from a shutoff of protein synthesis induced by ER stress: elucidation by GADD34-deficient mice. FASEB J 17(11):1573–1575. https://doi.org/10.1096/fj.02-1184fje
Novoa I, Zeng H, Harding HP, Ron D (2001) Feedback inhibition of the unfolded protein response by GADD34-mediated dephosphorylation of eIF2alpha. J Cell Biol 153(5):1011–1022. https://doi.org/10.1083/jcb.153.5.1011
Scheu S, Stetson DB, Reinhardt RL, Leber JH, Mohrs M, Locksley RM (2006) Activation of the integrated stress response during T helper cell differentiation. Nat Immunol 7(6):644–651. https://doi.org/10.1038/ni1338
Hurst KE, Lawrence KA, Robino RA, Ball LE, Chung D, Thaxton JE (2020) Remodeling translation primes CD8(+) T-cell antitumor immunity. Cancer Immunol Res 8(5):587–595. https://doi.org/10.1158/2326-6066.Cir-19-0516
Brand A, Singer K, Koehl GE, Kolitzus M, Schoenhammer G, Thiel A, Matos C, Bruss C, Klobuch S, Peter K, Kastenberger M, Bogdan C, Schleicher U, Mackensen A, Ullrich E, Fichtner-Feigl S, Kesselring R, Mack M, Ritter U, Schmid M, Blank C, Dettmer K, Oefner PJ, Hoffmann P, Walenta S, Geissler EK, Pouyssegur J, Villunger A, Steven A, Seliger B, Schreml S, Haferkamp S, Kohl E, Karrer S, Berneburg M, Herr W, Mueller-Klieser W, Renner K, Kreutz M (2016) LDHA-associated lactic acid production blunts tumor immunosurveillance by T and NK cells. Cell Metab 24(5):657–671. https://doi.org/10.1016/j.cmet.2016.08.011
Kusmartsev S, Nefedova Y, Yoder D, Gabrilovich DI (2004) Antigen-specific inhibition of CD8+ T cell response by immature myeloid cells in cancer is mediated by reactive oxygen species. J Immunol 172(2):989–999. https://doi.org/10.4049/jimmunol.172.2.989
Cao Y, Trillo-Tinoco J, Sierra RA, Anadon C, Dai W, Mohamed E, Cen L, Costich TL, Magliocco A, Marchion D, Klar R, Michel S, Jaschinski F, Reich RR, Mehrotra S, Cubillos-Ruiz JR, Munn DH, Conejo-Garcia JR, Rodriguez PC (2019) ER stress-induced mediator C/EBP homologous protein thwarts effector T cell activity in tumors through T-bet repression. Nat Commun 10(1):1280. https://doi.org/10.1038/s41467-019-09263-1
Hurst KE, Lawrence KA, Essman MT, Walton ZJ, Leddy LR, Thaxton JE (2019) Endoplasmic reticulum stress contributes to mitochondrial exhaustion of CD8(+) T cells. Cancer Immunol Res 7(3):476–486. https://doi.org/10.1158/2326-6066.Cir-18-0182
Han J, Back SH, Hur J, Lin YH, Gildersleeve R, Shan J, Yuan CL, Krokowski D, Wang S, Hatzoglou M, Kilberg MS, Sartor MA, Kaufman RJ (2013) ER-stress-induced transcriptional regulation increases protein synthesis leading to cell death. Nat Cell Biol 15(5):481–490. https://doi.org/10.1038/ncb2738
Harding HP, Zhang Y, Zeng H, Novoa I, Lu PD, Calfon M, Sadri N, Yun C, Popko B, Paules R, Stojdl DF, Bell JC, Hettmann T, Leiden JM, Ron D (2003) An integrated stress response regulates amino acid metabolism and resistance to oxidative stress. Mol Cell 11(3):619–633. https://doi.org/10.1016/S1097-2765(03)00105-9
Lim S, Kaldis P (2013) Cdks, cyclins and CKIs: roles beyond cell cycle regulation. Development 140(15):3079–3093. https://doi.org/10.1242/dev.091744
Goel S, DeCristo MJ, Watt AC, BrinJones H, Sceneay J, Li BB, Khan N, Ubellacker JM, Xie S, Metzger-Filho O, Hoog J, Ellis MJ, Ma CX, Ramm S, Krop IE, Winer EP, Roberts TM, Kim HJ, McAllister SS, Zhao JJ (2017) CDK4/6 inhibition triggers anti-tumour immunity. Nature 548(7668):471–475. https://doi.org/10.1038/nature23465
Schaer DA, Beckmann RP, Dempsey JA, Huber L, Forest A, Amaladas N, Li Y, Wang YC, Rasmussen ER, Chin D, Capen A, Carpenito C, Staschke KA, Chung LA, Litchfield LM, Merzoug FF, Gong X, Iversen PW, Buchanan S, de Dios A, Novosiadly RD, Kalos M (2018) The CDK4/6 inhibitor Abemaciclib induces a T cell inflamed tumor microenvironment and enhances the efficacy of PD-L1 checkpoint blockade. Cell Rep 22(11):2978–2994. https://doi.org/10.1016/j.celrep.2018.02.053
Brewer JW, Diehl JA (2000) PERK mediates cell-cycle exit during the mammalian unfolded protein response. Proc Natl Acad Sci USA 97(23):12625–12630. https://doi.org/10.1073/pnas.220247197
Zhang F, Hamanaka RB, Bobrovnikova-Marjon E, Gordan JD, Dai MS, Lu H, Simon MC, Diehl JA (2006) Ribosomal stress couples the unfolded protein response to p53-dependent cell cycle arrest. J Biol Chem 281(40):30036–30045. https://doi.org/10.1074/jbc.M604674200
Bourougaa K, Naski N, Boularan C, Mlynarczyk C, Candeias MM, Marullo S, Fåhraeus R (2010) Endoplasmic reticulum stress induces G2 cell-cycle arrest via mRNA translation of the p53 isoform p53/47. Mol Cell 38(1):78–88. https://doi.org/10.1016/j.molcel.2010.01.041
Buck MD, Sowell RT, Kaech SM, Pearce EL (2017) Metabolic instruction of immunity. Cell 169(4):570–586. https://doi.org/10.1016/j.cell.2017.04.004
Beckermann KE, Dudzinski SO, Rathmell JC (2017) Dysfunctional T cell metabolism in the tumor microenvironment. Cytokine Growth Factor Rev 35:7–14. https://doi.org/10.1016/j.cytogfr.2017.04.003
Scharping NE, Menk AV, Moreci RS, Whetstone RD, Dadey RE, Watkins SC, Ferris RL, Delgoffe GM (2016) The tumor microenvironment represses T cell mitochondrial biogenesis to drive intratumoral T cell metabolic insufficiency and dysfunction. Immunity 45(2):374–388. https://doi.org/10.1016/j.immuni.2016.07.009
Chang CH, Qiu J, O’Sullivan D, Buck MD, Noguchi T, Curtis JD, Chen Q, Gindin M, Gubin MM, van der Windt GJ, Tonc E, Schreiber RD, Pearce EJ, Pearce EL (2015) Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell 162(6):1229–1241. https://doi.org/10.1016/j.cell.2015.08.016
Sukumar M, Liu J, Ji Y, Subramanian M, Crompton JG, Yu Z, Roychoudhuri R, Palmer DC, Muranski P, Karoly ED, Mohney RP, Klebanoff CA, Lal A, Finkel T, Restifo NP, Gattinoni L (2013) Inhibiting glycolytic metabolism enhances CD8+ T cell memory and antitumor function. J Clin Investig 123(10):4479–4488. https://doi.org/10.1172/jci69589
Crompton JG, Sukumar M, Roychoudhuri R, Clever D, Gros A, Eil RL, Tran E, Hanada K, Yu Z, Palmer DC, Kerkar SP, Michalek RD, Upham T, Leonardi A, Acquavella N, Wang E, Marincola FM, Gattinoni L, Muranski P, Sundrud MS, Klebanoff CA, Rosenberg SA, Fearon DT, Restifo NP (2015) Akt inhibition enhances expansion of potent tumor-specific lymphocytes with memory cell characteristics. Cancer Res 75(2):296–305. https://doi.org/10.1158/0008-5472.Can-14-2277
van der Windt GJ, Everts B, Chang CH, Curtis JD, Freitas TC, Amiel E, Pearce EJ, Pearce EL (2012) Mitochondrial respiratory capacity is a critical regulator of CD8+ T cell memory development. Immunity 36(1):68–78. https://doi.org/10.1016/j.immuni.2011.12.007
Klein Geltink RI, Edwards-Hicks J, Apostolova P, O’Sullivan D, Sanin DE, Patterson AE, Puleston DJ, Ligthart NAM, Buescher JM, Grzes KM, Kabat AM, Stanczak M, Curtis JD, Hässler F, Uhl FM, Fabri M, Zeiser R, Pearce EJ, Pearce EL (2020) Metabolic conditioning of CD8(+) effector T cells for adoptive cell therapy. Nat Metab 2(8):703–716. https://doi.org/10.1038/s42255-020-0256-z
Raud B, Roy DG, Divakaruni AS, Tarasenko TN, Franke R, Ma EH, Samborska B, Hsieh WY, Wong AH, Stüve P, Arnold-Schrauf C, Guderian M, Lochner M, Rampertaap S, Romito K, Monsale J, Brönstrup M, Bensinger SJ, Murphy AN, McGuire PJ, Jones RG, Sparwasser T, Berod L (2018) Etomoxir actions on regulatory and memory T cells are independent of Cpt1a-mediated fatty acid oxidation. Cell Metab 28(3):504-515.e507. https://doi.org/10.1016/j.cmet.2018.06.002
Ma R, Ji T, Zhang H, Dong W, Chen X, Xu P, Chen D, Liang X, Yin X, Liu Y, Ma J, Tang K, Zhang Y, Peng Y, Lu J, Zhang Y, Qin X, Cao X, Wan Y, Huang B (2018) A Pck1-directed glycogen metabolic program regulates formation and maintenance of memory CD8(+) T cells. Nat Cell Biol 20(1):21–27. https://doi.org/10.1038/s41556-017-0002-2
Hurst KE, Lawrence KA, Reyes Angeles L, Ye Z, Zhang J, Townsend DM, Dolloff N, Thaxton JE (2019) Endoplasmic reticulum protein disulfide isomerase shapes T cell efficacy for adoptive cellular therapy of tumors. Cells. https://doi.org/10.3390/cells8121514
Pollizzi KN, Patel CH, Sun IH, Oh MH, Waickman AT, Wen J, Delgoffe GM, Powell JD (2015) mTORC1 and mTORC2 selectively regulate CD8+ T cell differentiation. J Clin Investig 125(5):2090–2108. https://doi.org/10.1172/jci77746
Bobrovnikova-Marjon E, Pytel D, Riese MJ, Vaites LP, Singh N, Koretzky GA, Witze ES, Diehl JA (2012) PERK utilizes intrinsic lipid kinase activity to generate phosphatidic acid, mediate Akt activation, and promote adipocyte differentiation. Mol Cell Biol 32(12):2268–2278. https://doi.org/10.1128/mcb.00063-12
Garcia D, Shaw RJ (2017) AMPK: mechanisms of cellular energy sensing and restoration of metabolic balance. Mol Cell 66(6):789–800. https://doi.org/10.1016/j.molcel.2017.05.032
Pearce EL, Walsh MC, Cejas PJ, Harms GM, Shen H, Wang LS, Jones RG, Choi Y (2009) Enhancing CD8 T-cell memory by modulating fatty acid metabolism. Nature 460(7251):103–107. https://doi.org/10.1038/nature08097
Porstmann T, Santos CR, Griffiths B, Cully M, Wu M, Leevers S, Griffiths JR, Chung YL, Schulze A (2008) SREBP activity is regulated by mTORC1 and contributes to Akt-dependent cell growth. Cell Metab 8(3):224–236. https://doi.org/10.1016/j.cmet.2008.07.007
Bobrovnikova-Marjon E, Hatzivassiliou G, Grigoriadou C, Romero M, Cavener DR, Thompson CB, Diehl JA (2008) PERK-dependent regulation of lipogenesis during mouse mammary gland development and adipocyte differentiation. Proc Natl Acad Sci USA 105(42):16314–16319. https://doi.org/10.1073/pnas.0808517105
Horton JD, Goldstein JL, Brown MS (2002) SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Investig 109(9):1125–1131. https://doi.org/10.1172/jci15593
Li Y, Xu S, Mihaylova MM, Zheng B, Hou X, Jiang B, Park O, Luo Z, Lefai E, Shyy JY, Gao B, Wierzbicki M, Verbeuren TJ, Shaw RJ, Cohen RA, Zang M (2011) AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice. Cell Metab 13(4):376–388. https://doi.org/10.1016/j.cmet.2011.03.009
Hardie DG (2004) The AMP-activated protein kinase pathway—new players upstream and downstream. J Cell Sci 117(Pt 23):5479–5487. https://doi.org/10.1242/jcs.01540
Wortel IMN, van der Meer LT, Kilberg MS, van Leeuwen FN (2017) Surviving stress: modulation of ATF4-mediated stress responses in normal and malignant cells. Trends Endocrinol Metab 28(11):794–806. https://doi.org/10.1016/j.tem.2017.07.003
Liu Z, Lv Y, Zhao N, Guan G, Wang J (2015) Protein kinase R-like ER kinase and its role in endoplasmic reticulum stress-decided cell fate. Cell Death Dis 6(7):e1822–e1822. https://doi.org/10.1038/cddis.2015.183
Donnelly N, Gorman AM, Gupta S, Samali A (2013) The eIF2α kinases: their structures and functions. Cell Mol Life Sci 70(19):3493–3511. https://doi.org/10.1007/s00018-012-1252-6
Deng J, Harding HP, Raught B, Gingras A-C, Berlanga JJ, Scheuner D, Kaufman RJ, Ron D, Sonenberg N (2002) Activation of GCN2 in UV-irradiated cells inhibits translation. Curr Biol 12(15):1279–1286. https://doi.org/10.1016/S0960-9822(02)01037-0
Masson GR (2019) Towards a model of GCN2 activation. Biochem Soc Trans 47(5):1481–1488. https://doi.org/10.1042/bst20190331
Lu L, Han AP, Chen JJ (2001) Translation initiation control by heme-regulated eukaryotic initiation factor 2alpha kinase in erythroid cells under cytoplasmic stresses. Mol Cell Biol 21(23):7971–7980. https://doi.org/10.1128/mcb.21.23.7971-7980.2001
Ilan L, Osman F, Namer LS, Eliahu E, Cohen-Chalamish S, Ben-Asouli Y, Banai Y, Kaempfer R (2017) PKR activation and eIF2α phosphorylation mediate human globin mRNA splicing at spliceosome assembly. Cell Res 27(5):688–704. https://doi.org/10.1038/cr.2017.39
Wek RC, Jiang HY, Anthony TG (2006) Coping with stress: eIF2 kinases and translational control. Biochem Soc Trans 34(Pt 1):7–11. https://doi.org/10.1042/bst20060007
Blais JD, Filipenko V, Bi M, Harding HP, Ron D, Koumenis C, Wouters BG, Bell JC (2004) Activating transcription factor 4 is translationally regulated by hypoxic stress. Mol Cell Biol 24(17):7469–7482. https://doi.org/10.1128/mcb.24.17.7469-7482.2004
Cemerski S, Cantagrel A, Van Meerwijk JP, Romagnoli P (2002) Reactive oxygen species differentially affect T cell receptor-signaling pathways. J Biol Chem 277(22):19585–19593. https://doi.org/10.1074/jbc.M111451200
Ligtenberg MA, Mougiakakos D, Mukhopadhyay M, Witt K, Lladser A, Chmielewski M, Riet T, Abken H, Kiessling R (2016) Coexpressed catalase protects chimeric antigen receptor-redirected T cells as well as bystander cells from oxidative stress-induced loss of antitumor activity. J Immunol 196(2):759–766. https://doi.org/10.4049/jimmunol.1401710
Rashidi A, Miska J, Lee-Chang C, Kanojia D, Panek WK, Lopez-Rosas A, Zhang P, Han Y, Xiao T, Pituch KC, Kim JW, Talebian M, Fares J, Lesniak MS (2020) GCN2 is essential for CD8(+) T cell survival and function in murine models of malignant glioma. Cancer Immunol Immunother 69(1):81–94. https://doi.org/10.1007/s00262-019-02441-6
Tameire F, Verginadis II, Leli NM, Polte C, Conn CS, Ojha R, Salas Salinas C, Chinga F, Monroy AM, Fu W, Wang P, Kossenkov A, Ye J, Amaravadi RK, Ignatova Z, Fuchs SY, Diehl JA, Ruggero D, Koumenis C (2019) ATF4 couples MYC-dependent translational activity to bioenergetic demands during tumour progression. Nat Cell Biol 21(7):889–899. https://doi.org/10.1038/s41556-019-0347-9
Yang X, Xia R, Yue C, Zhai W, Du W, Yang Q, Cao H, Chen X, Obando D, Zhu Y, Chen X, Chen JJ, Piganelli J, Wipf P, Jiang Y, Xiao G, Wu C, Jiang J, Lu B (2018) ATF4 regulates CD4(+) T cell immune responses through metabolic reprogramming. Cell Rep 23(6):1754–1766. https://doi.org/10.1016/j.celrep.2018.04.032
Vallejo M, Ron D, Miller CP, Habener JF (1993) C/ATF, a member of the activating transcription factor family of DNA-binding proteins, dimerizes with CAAT/enhancer-binding proteins and directs their binding to cAMP response elements. Proc Natl Acad Sci USA 90(10):4679–4683. https://doi.org/10.1073/pnas.90.10.4679
Hai T, Curran T (1991) Cross-family dimerization of transcription factors Fos/Jun and ATF/CREB alters DNA binding specificity. Proc Natl Acad Sci USA 88(9):3720–3724. https://doi.org/10.1073/pnas.88.9.3720
Huggins CJ, Mayekar MK, Martin N, Saylor KL, Gonit M, Jailwala P, Kasoji M, Haines DC, Quiñones OA, Johnson PF (2015) C/EBPγ is a critical regulator of cellular stress response networks through heterodimerization with ATF4. Mol Cell Biol 36(5):693–713. https://doi.org/10.1128/mcb.00911-15
Zhou H, Gao J, Lu ZY, Lu L, Dai W, Xu M (2007) Role of c-Fos/JunD in protecting stress-induced cell death. Cell Prolif 40(3):431–444. https://doi.org/10.1111/j.1365-2184.2007.00444.x
Angel P, Karin M (1991) The role of Jun, Fos and the AP-1 complex in cell-proliferation and transformation. Biochim Biophys Acta (BBA) Rev Cancer 1072(2):129–157. https://doi.org/10.1016/0304-419X(91)90011-9
Shaulian E, Karin M (2001) AP-1 in cell proliferation and survival. Oncogene 20(19):2390–2400. https://doi.org/10.1038/sj.onc.1204383
Fusakio ME, Willy JA, Wang Y, Mirek ET, Al Baghdadi RJ, Adams CM, Anthony TG, Wek RC (2016) Transcription factor ATF4 directs basal and stress-induced gene expression in the unfolded protein response and cholesterol metabolism in the liver. Mol Biol Cell 27(9):1536–1551. https://doi.org/10.1091/mbc.E16-01-0039
Sukumar M, Liu J, Mehta GU, Patel SJ, Roychoudhuri R, Crompton JG, Klebanoff CA, Ji Y, Li P, Yu Z, Whitehill GD, Clever D, Eil RL, Palmer DC, Mitra S, Rao M, Keyvanfar K, Schrump DS, Wang E, Marincola FM, Gattinoni L, Leonard WJ, Muranski P, Finkel T, Restifo NP (2016) Mitochondrial membrane potential identifies cells with enhanced stemness for cellular therapy. Cell Metab 23(1):63–76. https://doi.org/10.1016/j.cmet.2015.11.002
Thevenot PT, Sierra RA, Raber PL, Al-Khami AA, Trillo-Tinoco J, Zarreii P, Ochoa AC, Cui Y, Del Valle L, Rodriguez PC (2014) The stress-response sensor chop regulates the function and accumulation of myeloid-derived suppressor cells in tumors. Immunity 41(3):389–401. https://doi.org/10.1016/j.immuni.2014.08.015
Sena LA, Li S, Jairaman A, Prakriya M, Ezponda T, Hildeman DA, Wang CR, Schumacker PT, Licht JD, Perlman H, Bryce PJ, Chandel NS (2013) Mitochondria are required for antigen-specific T cell activation through reactive oxygen species signaling. Immunity 38(2):225–236. https://doi.org/10.1016/j.immuni.2012.10.020
Chamoto K, Chowdhury PS, Kumar A, Sonomura K, Matsuda F, Fagarasan S, Honjo T (2017) Mitochondrial activation chemicals synergize with surface receptor PD-1 blockade for T cell-dependent antitumor activity. Proc Natl Acad Sci USA 114(5):E761-e770. https://doi.org/10.1073/pnas.1620433114
Mak TW, Grusdat M, Duncan GS, Dostert C, Nonnenmacher Y, Cox M, Binsfeld C, Hao Z, Brüstle A, Itsumi M, Jäger C, Chen Y, Pinkenburg O, Camara B, Ollert M, Bindslev-Jensen C, Vasiliou V, Gorrini C, Lang PA, Lohoff M, Harris IS, Hiller K, Brenner D (2017) Glutathione primes T cell metabolism for inflammation. Immunity 46(4):675–689. https://doi.org/10.1016/j.immuni.2017.03.019
Sinclair LV, Rolf J, Emslie E, Shi YB, Taylor PM, Cantrell DA (2013) Control of amino-acid transport by antigen receptors coordinates the metabolic reprogramming essential for T cell differentiation. Nat Immunol 14(5):500–508. https://doi.org/10.1038/ni.2556
van der Windt GJ, Pearce EL (2012) Metabolic switching and fuel choice during T-cell differentiation and memory development. Immunol Rev 249(1):27–42. https://doi.org/10.1111/j.1600-065X.2012.01150.x
Castilho BA, Shanmugam R, Silva RC, Ramesh R, Himme BM (1843) Sattlegger E (2014) Keeping the eIF2 alpha kinase Gcn2 in check. Biochim Biophys Acta 9:1948–1968. https://doi.org/10.1016/j.bbamcr.2014.04.006
Van de Velde LA, Guo XJ, Barbaric L, Smith AM, Oguin TH 3rd, Thomas PG, Murray PJ (2016) Stress kinase GCN2 controls the proliferative fitness and trafficking of cytotoxic T cells independent of environmental amino acid sensing. Cell Rep 17(9):2247–2258. https://doi.org/10.1016/j.celrep.2016.10.079
Wek SA, Zhu S, Wek RC (1995) The histidyl-tRNA synthetase-related sequence in the eIF-2 alpha protein kinase GCN2 interacts with tRNA and is required for activation in response to starvation for different amino acids. Mol Cell Biol 15(8):4497–4506. https://doi.org/10.1128/mcb.15.8.4497
Munn DH, Mellor AL (2007) Indoleamine 2,3-dioxygenase and tumor-induced tolerance. J Clin Investig 117(5):1147–1154. https://doi.org/10.1172/jci31178
Halaby MJ, Hezaveh K, Lamorte S, Ciudad MT, Kloetgen A, MacLeod BL, Guo M, Chakravarthy A, Medina TDS, Ugel S, Tsirigos A, Bronte V, Munn DH, Pugh TJ, De Carvalho DD, Butler MO, Ohashi PS, Brooks DG, McGaha TL (2019) GCN2 drives macrophage and MDSC function and immunosuppression in the tumor microenvironment. Sci Immunol. https://doi.org/10.1126/sciimmunol.aax8189
Axten JM, Medina JR, Feng Y, Shu A, Romeril SP, Grant SW, Li WH, Heerding DA, Minthorn E, Mencken T, Atkins C, Liu Q, Rabindran S, Kumar R, Hong X, Goetz A, Stanley T, Taylor JD, Sigethy SD, Tomberlin GH, Hassell AM, Kahler KM, Shewchuk LM, Gampe RT (2012) Discovery of 7-methyl-5-(1-{[3-(trifluoromethyl)phenyl]acetyl}-2,3-dihydro-1H-indol-5-yl)-7H-pyrrolo[2,3-d]pyrimidin-4-amine (GSK2606414), a potent and selective first-in-class inhibitor of protein kinase R (PKR)-like endoplasmic reticulum kinase (PERK). J Med Chem 55(16):7193–7207. https://doi.org/10.1021/jm300713s
Atkins C, Liu Q, Minthorn E, Zhang SY, Figueroa DJ, Moss K, Stanley TB, Sanders B, Goetz A, Gaul N, Choudhry AE, Alsaid H, Jucker BM, Axten JM, Kumar R (2013) Characterization of a novel PERK kinase inhibitor with antitumor and antiangiogenic activity. Cancer Res 73(6):1993–2002. https://doi.org/10.1158/0008-5472.Can-12-3109
Sidrauski C, McGeachy AM, Ingolia NT, Walter P (2015) The small molecule ISRIB reverses the effects of eIF2α phosphorylation on translation and stress granule assembly. Elife. https://doi.org/10.7554/eLife.05033
Zyryanova AF, Weis F, Faille A, Alard AA, Crespillo-Casado A, Sekine Y, Harding HP, Allen F, Parts L, Fromont C, Fischer PM, Warren AJ, Ron D (2018) Binding of ISRIB reveals a regulatory site in the nucleotide exchange factor eIF2B. Science 359(6383):1533–1536. https://doi.org/10.1126/science.aar5129
Halliday M, Radford H, Sekine Y, Moreno J, Verity N, le Quesne J, Ortori CA, Barrett DA, Fromont C, Fischer PM, Harding HP, Ron D, Mallucci GR (2015) Partial restoration of protein synthesis rates by the small molecule ISRIB prevents neurodegeneration without pancreatic toxicity. Cell Death Dis 6(3):e1672–e1672. https://doi.org/10.1038/cddis.2015.49
Acknowledgements
This work was supported by Grant funds 1R01CA248359-01 to JET, 1R01CA244361-01A1 JET, T32 CA 193201 to AMA, and T32 DE01755 to MDT. We thank Sage Jadrnicek for figure design and artwork.
Funding
1R01CA248359-01 (JET), 1R01CA244361-01A1 (JET), T32 CA 193201 (AMA), T32 DE01755 (MDT).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the manuscript conception, outline, and overall design. AMA reviewed and wrote the first section. MDT reviewed and wrote the second section; JET revised, edited, and formalized the manuscript. All the authors read and approved the final manuscript and agreed that they are accountable for all the aspects of the work and assure the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andrews, A.M., Tennant, M.D. & Thaxton, J.E. Stress relief for cancer immunotherapy: implications for the ER stress response in tumor immunity. Cancer Immunol Immunother 70, 1165–1175 (2021). https://doi.org/10.1007/s00262-020-02740-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-020-02740-3