Abstract
Hereditary renal mass syndromes, although rare, account for at least 3–5% of kidney cancers and significantly impact affected families. Accurate diagnosis and management by radiologists are crucial as these syndromes often present at imaging with both renal and extra–renal manifestations. The radiologist may be the first to recognize these stigmata at imaging, some of which satisfy major features for diagnosis and obviate the need for genetic testing. Furthermore, radiologists contribute to lifelong imaging surveillance and locoregional treatment. This pictorial review discusses the following major hereditary renal mass syndromes with their typical renal mass appearance, extrarenal manifestations, inheritance pattern, diagnosis, and management strategies based on the most recent National Comprehensive Cancer Network guidelines: Von Hippel–Lindau syndrome, tuberous sclerosis complex, Birt–Hogg–Dube syndrome, hereditary paraganglioma/pheochromocytoma (PGL/PCC) syndrome/succinate dehydrogenase deficiency, hereditary leiomyomatosis and renal cell cancer (HLRCC)/fumarate hydratase deficiency, PTEN hamartoma syndrome, BRCA1-associated protein 1 (BAP1) tumor disposition syndrome, hereditary papillary renal cell carcinoma, and familial clear cell renal cell cancer with chromosome 3 translocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary renal mass syndromes account for at least 3–5% of all renal cell carcinomas (RCC) [1]. While uncommon, such patients account for disproportionate imaging as they require lifelong surveillance often starting in childhood [2]. Timely diagnosis often relies on the radiologist to correctly integrate clinical and imaging findings. Radiologists serve two roles in diagnosis and management. First, many syndromes are diagnosed clinically rather than genetically; patients may meet clinical criteria based on imaging and radiologists may be the first to recognize these patterns. Second, imaging can noninvasively monitor these patients at a higher risk of RCC and from a younger age [2].
The criteria to initiate evaluation for hereditary renal mass syndromes include early age of RCC (≤ 46 years), bilateral or multifocal RCCs, and any of the following histology: multifocal papillary; fumarate hydratase deficiency; succinate dehydrogenase deficiency; multiple chromophobe, oncocytoma, or hybrid; and angiomyolipoma with additional tuberous sclerosis complex criteria. Clinical criteria such as family history are summarized in [2]. Clinical context is emphasized as inherited and sporadic RCCs appear similarly when considered in isolation. Early age presentation, bilateral or multifocal involvement, and systemic stigmata suggests a systemic diagnosis.
This review examines major hereditary renal mass syndromes, highlighting renal mass appearance, extrarenal manifestations, inheritance patterns, diagnosis, and management, focusing on most recent National Comprehensive Cancer Network® (NCCN) (2024), American Urological Association (2021), and World Health Organization 5th edition (2022) nomenclature and guidelines [2,3,4]. Clinical features and renal mass surveillance strategies are summarized in Tables 1 and 2, respectively.
Von Hippel–Lindau Syndrome
Von Hippel–Lindau syndrome (vHL) is caused by germline mutations in the vHL tumor suppressor gene [2]. vHL is the primary cause of hereditary RCC, which develops in about half of patients with vHL at a mean age of 39 [5]. Essentially all RCCs are clear cell subtype and biopsy is typically not required. RCC related death accounts for about 50% of mortality among patients with vHL [5, 6]. Clear cell RCCs can be solid or cystic, and even a cyst relatively few features can represent RCC (Fig. 1). For this reason, the Bosniak classification system does not apply to vHL or any patient with a hereditary renal mass syndrome [5]. vHL-associated RCCs and sporadic clear cell RCCs appear similarly (e.g. hypervascular, T2 hyperintense, and microscopic fat) with the exception that they vHL-associated RCCs are commonly multiple and/or bilateral [7]. Of note, clear cell RCCs account for most sporadic RCCs and mutational inactivation of the vHL gene is the most common cause, though such patients do not have other stigmata of vHL [8].
37-year-old man with von Hippel–Lindau syndrome presents for surveillance with MRI. A Axial T2–weighted images with fat–suppression and B axial T1–weighted corticomedullary phase with fat–suppression show a left cystic renal mass with multiple, thin septa (arrow), pancreatic cystosis (pentagon arrow), and a spinal canal hemangioblastoma (notched arrow). Partial left nephrectomy showed a clear cell RCC
Extra-renal manifestations include pancreatic masses (cysts, serous cystadenomas, and neuroendocrine tumors), paragangliomas, cystadenomas of the broad ligament or epididymis (causing infertility if bilateral), inner ear endolymphatic sac tumors (causing hearing loss), retinal angiomas, and nervous system hemangioblastomas (causing blindness if retinal) [5, 6].
Inheritance is autosomal dominant and highly penetrant. vHL can be diagnosed via a genetic test or clinically. Clinical criteria consist of either a vHL-related manifestation and a 1st or 2nd degree relative with vHL, or ≥ 2 vHL-related manifestations in patients without a family history [2, 5, 6].
For renal masses, patients are recommended multiphasic abdominal MRI or CT every 2 years starting at age 15. For vHL and all subsequent syndromes described, MRI is generally preferred because it does not involve ionizing radiation and patients are expected to undergo repeated imaging at an early age [2, 3]. Patients with RCC are recommended nephron-sparing surgery (NSS) when ≥ 3 cm. Thermal ablation can be considered depending on medical or surgical risk, and this applies to all other hereditary renal mass syndromes described below who are also candidates for NSS [2].
Tuberous sclerosis complex
Tuberous sclerosis complex (TSC) is a neurocutaneous syndrome caused by mutations of the tumor suppressor genes TSC1 or TSC2, most of which are spontaneous germline mutations. TSC affects approximately 1/10,000 people and most (75–80%) develop angiomyolipomas (AMLs), which can include the epithelioid subtype [9]. The RCC risk is similar to that of the general population but occurs earlier at a mean age of 28 [10]. TSC-associated RCCs are histologically unique, diverse, and clinically indolent; clear cell histology is less common [2, 11, 12]. Approximately 5% of TSC patients also have polycystic kidney disease, i.e. continuous gene syndrome, which occurs because the responsible genes are adjacent. These patients have worse prognosis with earlier progression to renal failure [13].
Typical extra-renal manifestations include dermatologic lesions (including focal hypomelanotic areas- “ash leaf lesions” and facial angiofibromas), subependymal nodules, cortical and subependymal tubers (large dysplastic neurons and astrocytes) leading to seizures or developmental delay, lymphangioleiomyomatosis (LAM) leading to cystic lung disease, multifocal micronodular pneumocyte hyperplasia, liver AMLs, and cardiac rhabdomyomas (Fig. 2) [13]. Seizure- and kidney-related complications (including hemorrhagic AML) account for most mortality [10].
31-year-old woman with tuberous sclerosis complex undergoing evaluation for lung transplant. A Lung windows of coronal portal venous phase CT shows hyperinflated lungs with innumerable thin-walled cysts of varying sizes replacing the normal parenchyma compatible with lymphangiomyomatosis (arrows). B Soft tissue windows through the same level shows multiple angiomyolipomas in both the liver (arrows) and kidneys (notched arrows). C Coronal CT without contrast shows myocardial fatty foci (arrows)
Inheritance is autosomal dominant. TSC can be diagnosed via a genetic test that identifies the pathognomonic mutations though 10–25% of patients do not have such identifiable mutation. Alternatively, TSC can be diagnosed clinically with two major features or one major feature and two minor features [2, 10]. One exception is the combination of LAM and AMLs; although both major features, this combination in isolation is insufficient for diagnosis.
For renal masses, patients are recommended multiphasic abdominal MRI or CT every 3–5 years starting at age 12. For RCCs, NSS is recommended [2]. For larger AMLs, embolization, NSS, and/or targeted systemic therapy with mTOR inhibitors are recommended due to the risk of bleeding [2, 10].
Birt–Hogg–Dubé Syndrome
Birt–Hogg–Dubé syndrome (BHD) is caused by an inactivating germline mutation in the folliculin tumor suppressor gene (FLCN) [2]. Patients have a 19–35% likelihood of developing RCC with a median age of diagnosis at 48 [14]. The majority of these RCCs are chromophobe RCC or hybrid oncocytic tumors (i.e. mixed oncocytoma and chromophobe RCC), latter of which is characteristic of BHD [2, 14, 15]. These masses have moderate enhancement relative to renal cortex and T2 iso- or hyperintensity, without microscopic fat [9, 15]. Other RCC subtypes are possible [2].
Extra-renal manifestations include cystic lung disease, which affects > 80% of patients and can lead to spontaneous pneumothorax in 25% of patients [15]. The cysts are usually basilar, irregularly-shaped with variable sizes, and abut pleural surfaces. Dermatologic lesions are common [14].
Inheritance is autosomal dominant and is highly penetrant. Patients can be diagnosed via a genetic test or clinically [2, 14]. Cystic lung disease and RCC (oncocytic tumors, early onset RCC (defined as < 50 years of age), or multifocal or bilateral RCCs) are each minor criteria and this combination establishes the diagnosis. Radiologists may be the first clinician to recognize this combination [16] (Fig. 3).
45-year-old man with Birt–Hogg–Dubé presents with shortness of breath. A Axial CT chest in the lung windows shows a large right pneumothorax (asterisk) causing leftward mediastinal shift and lung collapse (arrow). B Coronal portal venous phase CT abdomen in the lung windows shows a large right pneumothorax (asterisk) and in the soft tissue windows, C bilateral renal masses (arrows). Surgical pathology showed hybrid chromophobic oncocytic tumors. D Axial CT of the lungs after re-expansion shows bibasilar, irregularly shaped, subpleural cysts of variable sizes (notched arrow)
For renal masses, patients are recommended multiphasic abdominal MRI or CT every 3 years starting at age 20. For RCCs, NSS is recommended [2].
Hereditary paraganglioma/pheochromocytoma (PGL/PCC) syndrome/succinate dehydrogenase deficiency
PGL/PCC refers to a family of mutations in the succinate dehydrogenase (SDH) enzyme. SDH is responsible for catalyzing the oxidation of succinate to fumarate in the Krebs cycle. When deficient, the cellular microenvironment becomes hypoxic. The oxidative stress leads to abnormal cell proliferation and the Warburg effect [17]. The enzyme has four subunits (A through D) and each subunit mutation result in a different syndrome. All syndromes nevertheless result in paragangliomas or pheochromocytoma. Associated RCCs are termed SDH-deficient RCCs and most commonly have mutations in subunit B (SDHB). SDHB affect ~ 1/1,000,000 people and SDH-deficient RCCs comprise 0.05–0.2% of all RCCs. For patients with SDHB mutations, the risk of RCC is estimated to be 14% which develops at a mean age of 33 [17,18,19]. About 26% of patients have bilateral RCCs at presentation. RCCs can be either cystic or solid (with internal cystic or necrotic components) and intensely hypermetabolic at FDG-PET/CT due to the Warburg effect (Fig. 4) [17,18,19]. Local invasion and metastases are common [18, 20].
36-year-old woman with SDHB mutation presented with headaches, anxiety, palpitations, and high metanephrines. Maximum intensity projection FDG-PET/CT in the A anterior and B posterior projections show 3 hypermetabolic masses: a left adrenal mass (arrow) and two left renal masses. C Axial FDG-PET/CT shows that adrenal mass (arrow) and the upper pole renal mass (notched arrow) are intensely hypermetabolic. D Axial FDG-PET/CT shows that the lower pole renal mass (notched arrow) is also intensely hypermetabolic. E Coronal corticomedullary phase CT shows a hypervascular adrenal mass (arrow) and a cystic renal mass (notched arrow). Surgical pathology confirmed a pheochromocytoma and two succinate dehydrogenase deficient renal cell carcinomas
Extra-renal manifestations include gastrointestinal stromal tumors (GIST) and pheochromocytoma/paragangliomas, each of which can occur synchronously with the RCC in 15% of patients [18]. Pulmonary chondromas can also occur, and this combined with GIST and pheochromocytoma/paragangliomas is known as Carney triad.
Inheritance is autosomal dominant with variable penetrance [19]. Diagnosis is multidisciplinary, integrating clinical symptoms, family history, identification of a paraganglioma or pheochromocytoma at imaging, biochemical testing, and genetic testing. Immunohistochemistry can also confirm SDH-deficient RCC in the absence of family history or confirmed genetic mutation, which occurs due to variable penetrance and unconventional mutations.
For renal masses, patients are recommended multiphasic abdominal MRI or CT every 4–6 years starting at age 12. For RCCs, wide surgical margin is recommended due to the aggressive nature of the tumor [2, 3, 17].
Hereditary leiomyomatosis and renal cell cancer (HLRCC)/fumarate hydratase deficiency
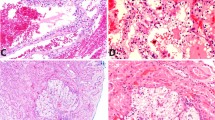
Hereditary leiomyoma renal cell carcinoma (HLRCC) is caused by mutations on the fumarate hydratase (FH) gene. The gene encodes for a Krebs cycle enzyme that converts fumarate to malate. Similar to succinate dehydrogenase deficiency, FH deficiency causes a hypoxic microenvironment, leading to abnormal cell growth. In one series, RCC developed in 32% of patients, as early as age 11 [21] though the median age of RCC presentation is 46. These RCCs are now termed FH-deficient RCCs but were previously labeled as Type 2 papillary RCCs [4]. FH-deficient RCCs are biologically aggressive, appear infiltrative at imaging, have cystic or necrotic components, and present as locally advanced disease with both nodal and distant organ metastases even when the primary tumor is small (Fig. 5) [21, 22]. Similar to SDH-deficient RCCs, FH-deficient RCCs are intensely hypermetabolic at FDG-PET/CT [22].
58-year-old man with hereditary leiomyomatosis and renal cell cancer. Serial coronal portal venous phase CTs showed A an ill-defined hypoenhancing mass in the right lower pole (arrow). B In only 17 months, the mass enlarged and replaced the right lower pole, with infiltrative spread to the upper pole (arrow). The mass directly extended into the inferior vena cava (IVC; notched arrow). C One month later, the mass continued to grow, now replacing the entire kidney (arrow) and extending further along the IVC (notched arrow). The mass had also bled with blood products layering along the extraperitoneal fascial planes (pentagon arrow). Radical nephrectomy confirmed a grade 4 fumarate hydratase-deficient renal cell carcinoma with inferior vena cava, fascia, and adrenal gland invasion. Molecular testing lating confirmed that the patient had hereditary leiomyomatosis and renal cell cancer
Extra-renal manifestations include cutaneous leiomyomas and uterine leiomyomas (in women), both of which are common with 90–100% penetrance [21]. Uterine leiomyomas present at an earlier age and are larger. Cutaneous leiomyomas, when present, usually continue to grow in size and number [21].
Inheritance is autosomal dominant. While HLRCC is considered rare, it is likely underdiagnosed as penetrance is variable and low [22]. Diagnosis is through genetic testing. There is currently no consensus on clinical diagnosis although proposed criteria include a combination of leiomyomas and a FH-deficient RCC.
For renal masses, patients are recommended multiphasic abdominal MRI or CT every year starting at 8–10, the earliest and most frequent recommendation among the syndromes described here. For RCCs, radical nephrectomy is recommended due to aggressive biology and rapid growth [2].
PTEN Hamartoma Tumor Syndrome
PTEN Hamartoma Tumor Syndrome is caused by mutations in the tumor suppressor gene PTEN [3]. The syndrome may manifest in one of four distinct sub-syndromes: Cowden syndrome, Bannayan–Riley–Ruvalcaba syndrome, Proteus syndrome, and Proteus-like syndrome [23]. The incidence is 1/200,000 and patients have a 34% lifetime risk of RCC, which occurs at a mean age of 40 [23]. The RCC subtypes vary though clear cell is the least common [2, 23, 24].
Inheritance is autosomal dominant and can be diagnosed via genetic testing or clinically, which varies based on the sub-syndromes [23, 24]. Clinical criteria include major criteria (e.g. breast cancer, endometrial cancers, follicular thyroid cancer, mucocutaneous lesions, gastrointestinal hamartomas) and minor criteria (e.g. goiter, lipomas, fibroids, testicular lipomatosis, RCCs, vascular anomalies, developmental delay) (Fig. 6).
51-year-old woman with a history of breast cancer, thyroid cancer, and PTEN hamartoma syndrome presents for evaluation of a right renal mass and left femoral vein vascular malformation. A Coronal portal venous phase CT shows a hypovascular, solid right renal mass (arrow) and a left femoral vascular malformation (notched arrow), shown at surgical pathology to represent a papillary RCC. B Conventional catheter angiography of the left femoral artery shows C early venous drainage through a complex, tangled network corresponding to the arteriovenous malformations (notched arrows)
For renal masses, patients undergo ultrasound every 1–2 years starting at age 40 [24]. Patients who develop RCCs are recommended NSS [2].
BRCA1-associated protein 1 (BAP1) Tumor Disposition Syndrome
BAP1 Tumor Disposition Syndrome is caused by mutations on the BRCA associated protein, a tumor suppressor [2]. The syndrome is associated with clear cell RCC, and the mean age of RCC diagnosis is 53 [25]. Patients are more likely to develop extrarenal malignancies and the lifetime risk of any malignancy is 85% [28]. Of note, patients can also develop sporadic clear cell RCCs with BAP1 mutations, and these are associated with higher Fuhrman grades and poorer survival. Inheritance is autosomal dominant and can only be diagnosed genetically [2, 26].
Extrarenal manifestations include mesothelioma, cutaneous or uveal melanoma, and other cutaneous neoplasms (both malignant and benign) [2, 25, 26]. More recently proposed associations include meningioma, cholangiocarcinoma, and hepatocellular carcinoma (Fig. 7) [26].
59-year-old man with BAP1 tumor disposition syndrome presents with abdominal pain and jaundice. A Axial T1-weighted late hepatic arterial phase MRI shows a bilobed targetoid central mass with rim arterial phase hyperenhancement (arrow). B Axial T1-weighted delayed phase MRI shows that the mass has peripheral washout (arrow) and delayed central enhancement (notched arrow), as well as subtle intrahepatic bile duct dilation in the lateral left lobe. C Axial T1-weighted late hepatic arterial phase (equivalent to corticomedullary phase in this patient) MRI shows a hypervascular solid renal mass in the right posterior interpolar region (arrow). Tissue sampling confirmed cholangiocarcinoma and clear cell renal cell carcinoma, respectively
Patients are recommended multiphasic abdominal MRI or CT 2 years starting at age 30 [2]. Patients who develop RCCs are recommended NSS [3].
Hereditary papillary renal cell carcinoma
Hereditary papillary RCC is caused by activating germline mutations in the Mesenchymal Epithelial Transition (MET) gene, which encodes a tyrosine kinase receptor. This rare syndrome is reported in fewer than 60 reported families and causes a higher risk of papillary RCCs, occurring at a mean age of 42 [27]. Patients present with multifocal and/or bilateral papillary RCCs (Fig. 8), which are usually solid renal masses with hypovascular enhancement, T2-hypointense signal, and variable intrinsic T1-hyperintense signal, or less commonly, cystic renal mass with variable intrinsic T1-hyperintense signal [28]. Patients can develop numerous microscopic precursor lesions such as adenomas and papillary lesions. There are no known extra-renal manifestations.
68-year-old man with a history of hereditary papillary renal cell carcinoma presents for surveillance of renal masses. A Axial T1-weighted corticomedullary phase MRI and B coronal corticomedullary phase CT show multiple, bilateral hypoenhancing masses (arrows). Radical left nephrectomy confirmed 7 papillary renal cell carcinomas. Partial right nephrectomy confirmed a single papillary renal cell carcinoma
Inheritance is autosomal dominant, highly penetrant, and diagnosed via genetic testing as all pathologic variants so far have been localized to the MET gene [27]. Genetic testing can be performed when a patient has a known family history, papillary RCC diagnosed < 45 years, personal history of > 1 papillary RCC, or a papillary RCC with precursor lesions in the surrounding parenchyma [27].
Patients are recommended to undergo a multiphasic abdominal MRI or CT every 1–2 years starting at age 30. Patients who develop RCCs are recommended NSS [2].
Familial clear cell renal cancer with chromosome 3 translocation
Familial clear cell renal cancer with chromosome 3 translocation involves a balanced translocation of the short arm of chromosome 3 and is associated with clear cell RCC [2, 29]. The mean age of RCC diagnosis is 52 [30]. Although the vHL gene is located on 3p, the vHL portion is typically intact and patients do not have the other vHL manifestations. As discussed above, clear cell RCCs are hypervascular and T2 hyperintense, with possible microscopic fat [9]. There are no known extra-renal manifestations [1].
Inheritance is autosomal dominant [2]. Not all patients have a higher risk of RCC, as the translocation may not disrupt a tumor suppressor gene. Without a family history, patients have a similar risk of RCC as the general population [30]. The translocation can be diagnosed by karyotyping white blood cells [29]. Due to rarity and variable RCC risk, there are no specific surveillance guidelines.
Conclusion
Hereditary renal cancer syndromes present a significant risk for RCC and extra-renal manifestations. Early diagnosis, imaging surveillance, and timely interventions can improve outcomes. MRI is preferred for surveillance over CT as patients are expected to undergo repeated imaging at an early age. Once diagnosed with RCC, standard treatment consists of observation if small or NSS versus thermal ablation. Two exceptions are RCCs from HLRCC and PGL/PCC, which require wide resection margins due aggressive biology. Understanding the genetic and clinical aspects of these syndromes is essential for radiologists to ensure comprehensive patient care.
Data availability
No datasets were generated or analysed during the current study.
References
Haas NB, Nathanson KL. Hereditary kidney cancer syndromes. Adv Chronic Kidney Dis. 2014;21(1):81–90. https://doi.org/10.1053/j.ackd.2013.10.001
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Kidney Cancer V.1.2025. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed [July 9, 2024]. To view the most recent and complete version of the guideline, go online to NCCN.org.
Campbell SC, Uzzo RG, Karam JA, Chang SS, Clark PE, Souter L. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow–up: AUA Guideline: Part II. J Urol. 2021;206(2):209–218. https://doi.org/10.1097/JU.0000000000001912
Moch H, Amin MB, Berney DM, et al. The 2022 World Health Organization Classification of Tumours of the Urinary System and Male Genital Organs–Part A: Renal, Penile, and Testicular Tumours. Eur Urol. 2022;82(5):458–468. https://doi.org/10.1016/j.eururo.2022.06.016
Chahoud J, McGettigan M, Parikh N, et al. Evaluation, diagnosis and surveillance of renal masses in the setting of VHL disease. World J Urol. 2021;39(7):2409–2415. https://doi.org/10.1007/s00345-020-03441-3
van Leeuwaarde RS, Ahmad S, van Nesselrooij B, et al. Von Hippel–Lindau Syndrome. 2000 May 17 [Updated 2024 Feb 29]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1463/
Shetty AS, Fraum TJ, Ballard DH, et al. Renal Mass Imaging with MRI Clear Cell Likelihood Score: A User's Guide. RadioGraphics. 2023;43(7):e220209. https://doi.org/10.1148/rg.220209
Cowey CL, Rathmell WK. VHL gene mutations in renal cell carcinoma: role as a biomarker of disease outcome and drug efficacy. Curr Oncol Rep. 2009;11(2):94–101. https://doi.org/10.1007/s11912-009-0015-5
Dixon BP, Hulbert JC, Bissler JJ. Tuberous sclerosis complex renal disease. Nephron Exp Nephrol. 2011;118(1):e15–e20. https://doi.org/10.1159/000320891
Wang MX, Segaran N, Bhalla S, et al. Tuberous Sclerosis: Current Update. RadioGraphics. 2021;41(7):1992–2010. https://doi.org/10.1148/rg.2021210103
Yang P, Cornejo KM, Sadow PM, et al. Renal cell carcinoma in tuberous sclerosis complex. Am J Surg Pathol. 2014;38(7):895–909. https://doi.org/10.1097/PAS.0000000000000237
Guo J, Tretiakova MS, Troxell ML, et al. Tuberous sclerosis–associated renal cell carcinoma: a clinicopathologic study of 57 separate carcinomas in 18 patients. Am J Surg Pathol. 2014;38(11):1457–1467. https://doi.org/10.1097/PAS.0000000000000248
Rout P, Zamora EA, Aeddula NR. Tuberous Sclerosis. [Updated 2024 May 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538492/
Sattler EC, Steinlein OK. Birt–Hogg–Dubé Syndrome. In: Adam MP, Mirzaa GM, Pagon RA, et al., eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; February 27, 2006.
Bhatnagar A, Rowe SP, Gorin MA, Pomper MG, Fishman EK, Allaf ME. Computed Tomography Appearance of Renal Hybrid Oncocytic/Chromophobe Tumors. J Comput Assist Tomogr. 2016;40(4):513–516. https://doi.org/10.1097/RCT.0000000000000409
Lee E, Sayyouh M, Haggerty JE, Kazerooni E, Agarwal PP. Role of Radiologists in the Diagnosis of Unsuspected Birt–Hogg–Dubé Syndrome in a Tertiary Clinical Practice. AJR Am J Roentgenol. 2019;213(4):792–797. https://doi.org/10.2214/AJR.19.21176
Ricketts CJ, Shuch B, Vocke CD, et al. Succinate dehydrogenase kidney cancer: an aggressive example of the Warburg effect in cancer. J Urol. 2012;188(6):2063–2071. https://doi.org/10.1016/j.juro.2012.08.030
Gill AJ, Hes O, Papathomas T, et al. Succinate dehydrogenase (SDH)–deficient renal carcinoma: a morphologically distinct entity: a clinicopathologic series of 36 tumors from 27 patients. Am J Surg Pathol. 2014;38(12):1588–1602. https://doi.org/10.1097/PAS.0000000000000292
Withey SJ, Perrio S, Christodoulou D, et al. Imaging Features of Succinate Dehydrogenase–deficient Pheochromocytoma–Paraganglioma Syndromes. RadioGraphics. 2019;39(5):1393–1410. https://doi.org/10.1148/rg.2019180151
Charbel C, Causa Andrieu PI, Soliman M, et al. The Prevalence and Radiologic Features of Renal Cancers Associated with FLCN, BAP1, SDH, and MET Germline Mutations. Radiol Imaging Cancer. 2024;6(2):e230063. https://doi.org/10.1148/rycan.230063
Vocke CD, Ricketts CJ, Merino MJ, et al. Comprehensive genomic and phenotypic characterization of germline FH deletion in hereditary leiomyomatosis and renal cell carcinoma. Genes Chromosomes Cancer. 2017;56(6):484–492. https://doi.org/10.1002/gcc.22452
Nikolovski I, Carlo MI, Chen YB, Vargas HA. Imaging features of fumarate hydratase–deficient renal cell carcinomas: a retrospective study. Cancer Imaging. 2021;21(1):24. Published 2021 Feb 19. https://doi.org/10.1186/s40644-021-00392-9
Mester JL, Zhou M, Prescott N, Eng C. Papillary renal cell carcinoma is associated with PTEN hamartoma tumor syndrome. Urology. 2012;79(5):1187.e1-1187.e11877.
Tischkowitz M, Colas C, Pouwels S, Hoogerbrugge N; PHTS Guideline Development Group; European Reference Network GENTURIS. Cancer Surveillance Guideline for individuals with PTEN hamartoma tumour syndrome. Eur J Hum Genet. 2020;28(10):1387–1393. https://doi.org/10.1038/s41431-020-0651-7
Farley MN, Schmidt LS, Mester JL, et al. A novel germline mutation in BAP1 predisposes to familial clear–cell renal cell carcinoma. Mol Cancer Res. 2013;11(9):1061–1071. https://doi.org/10.1158/1541-7786.MCR-13-0111
Lalloo F, Kulkarni A, Chau C, et al. Clinical practice guidelines for the diagnosis and surveillance of BAP1 tumour predisposition syndrome. Eur J Hum Genet. 2023;31(11):1261–1269. https://doi.org/10.1038/s41431-023-01448-z
PDQ Cancer Genetics Editorial Board. Hereditary Papillary Renal Carcinoma (PDQ®): Health Professional Version. 2024 Feb 16. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002–. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568504/
Shen L, Yoon L, Mullane PC, Liang T, Tse JR. World Health Organization (WHO) 2022 Classification Update: Radiologic and Pathologic Features of Papillary Renal Cell Carcinomas. Acad Radiol. Published online February 15, 2024. https://doi.org/10.1016/j.acra.2024.01.034
Cohen AJ, Li FP, Berg S, et al. Hereditary renal–cell carcinoma associated with a chromosomal translocation. N Engl J Med. 1979;301(11):592–595. https://doi.org/10.1056/NEJM197909133011107
Woodward ER, Skytte AB, Cruger DG, Maher ER. Population–based survey of cancer risks in chromosome 3 translocation carriers. Genes Chromosomes Cancer. 2010;49(1):52–58. https://doi.org/10.1002/gcc.20718
Author information
Authors and Affiliations
Contributions
A.Y. and J.R.T. wrote the initial draft, revised the manuscript during peer review, prepared all tables, and prepared all figures. All authors reviewed and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Justin R Tse receives grant support from GE Healthcare and Bayer Healthcare, and is a consultant for Intuitive Surgical, Inc., AbSolutions Med, Inc., and Ascelia Pharma AB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoon, A.H., Tse, J.R. Hereditary renal mass syndromes: a pictorial review. Abdom Radiol (2024). https://doi.org/10.1007/s00261-024-04534-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00261-024-04534-y