Abstract
Purpose
Preoperative imaging is now recommended in patients with suspected acute appendicitis (AA) by the World Society of Emergency Surgery. Our aims were (i) to describe our local practice and (ii) to evaluate the efficiency of performing ultrasound (US) and/or computed tomography (CT) by assessing management failure, specificity and sensitivity, and length of stay in the emergency department (ED).
Methods
This single-center retrospective study included all patients who underwent US or CT for the management of suspected AA. Patients were included if they were admitted to the ED in February or June between 2012 and 2021.
Results
The study included 339 patients. US was performed in 278 patients (82%), of whom 91 also had a second-line CT (31.3%). There was a significant increase in the rate of CT over the inclusion period. Three percent (3%) of the patients had management failure and a higher age and CT or US + CT were significantly associated with the risk of management failure. Length of stay in the ED increased significantly when a second-line CT was performed. The sensitivity and specificity of US were 84.8% and 93.2%, respectively. Sensitivity was significantly different from CT (100%, p = 0.03) but not specificity (87.9%, p = 0.29). Both US and CT results were more likely to be considered for further management if positive. The vast majority of patients with negative or inconclusive results were admitted in surgical wards or underwent a second-line examination.
Conclusion
If available in the hospital together with CT, US should probably be performed systematically and as a first-line examination in patients with suspected acute appendicitis.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Acute appendicitis (AA) is common with a rate of 90-100 patients per 100 000 inhabitants [1] and accounts for 7-10 % in emergency department (ED) admissions [2]. The risk of misdiagnosis and management failure of acute appendicitis (AA) is high (0–46% of normal appendectomy reported) and varies between countries [3, 4]. As systematic preoperative imaging has been shown to reduce the rate of normal appendectomy [5], the routine use of non-invasive imaging has been included in the French guidelines. Indeed, the French Health Authority (HAS) recommends systematic preoperative ultrasound (US) in young adult patients and computed tomography (CT) in older patients [6]. The World Society of Emergency Surgery (WSES) recommends the systematic use of combined clinical parameters and US [7]. Despite these recommendations, a recent systematic review found that only 73% of women and 36% of men undergo systematic preoperative imaging for suspected appendicitis [4]. This wide discrepancy between international recommendations and actual real practice raises the question of management efficiency. US as a first-line examination has the advantage of being widely available, radiation-free and potentially more cost-effective. However, there is a discrepancy between studies and some studies report lower diagnostic accuracy for US compared with CT [5]. This may lead to a second-line examination, thus increasing the length of stay in the emergency department and increasing costs. Determining of the best pathway to reduce misdiagnosis, management failure and length of stay in the ED will improve the management of patients with suspected AA and be more cost-effective.
The aims of this study were (i) to describe current practice and (ii) to evaluate the efficiency of performing US and/or CT on suspected AA patients by assessing management failure, specificity and sensitivity, and length of stay in the ED.
Material and methods
Ethical aspects
This study was approved by the National Commission of Informatics and Freedom (CNIL) (Number ar23-0020v0).
Patients
This retrospective observational study included consecutive patients who came to our emergency department (ED) with symptoms of acute abdominal pain in the right lower quadrant. Patients were included when admitted in our emergency department in February or June between years 2012 and 2021. This was considered as a 10-years representative sample. Other inclusion criteria were: pain evaluation with abdominal ultrasonography (US) and/or abdominal computed tomography (CT). Exclusion criteria were: < 18 years and patients for whom the diagnosis of AA was not explored by US or CT.
Study design and outcomes
All electronic US and CT reports in our Radiology Information Systems (RIS: DxImageRIS 4.9.6.1 Medasys 2015) from the inclusion period were electronically screened using the abbreviation appendi*. US and/or CT examinations were considered if the abbreviation appendi* was present in the indication or conclusion of the report.
Patient care was collected from electronic files (M-CrossWay 8.2.7R8.0.2 RC3 Maincare Solutions 2023) to describe clinical practice. The following data were collected: any additional examination (US, CT), patient orientation, the date and exact time of admission to and discharge from the emergency department. Other collected data were: (i) demographic data (age, gender, body mass index (BMI)), (ii) clinical examination and biological results, (iii) management conclusion.
The primary endpoint was management failure. Management failure was defined as: (i) initial misdiagnosis of “appendicitis” with a normal-appearing appendix at surgery confirmed by the pathologist (negative appendectomy); (ii) initial misdiagnosis of “no appendicitis” with patient discharged from the hospital and subsequent readmission with a diagnosis of appendicitis.
The final diagnosis of appendicitis was made during surgery, prior to the analysis by a pathologist. If the patient was discharged without surgery, the diagnosis of appendicitis was made in the case of subsequent readmission and positive surgery. The sensitivity and specificity of US and CT for the non-invasive diagnosis of appendicitis were assessed accordingly.
Statistical analysis
Categorical data were described using percentages and compared using Fisher exact tests, and continuous data using means and standard deviations, and compared using Mann & Whitney tests.
Sensitivity, specificity and their 95% confidence interval were assessed using binomial exact method. Diagnosis tools were considered as presenting good properties is the low boundary of the specificity and sensitivity confidence intervals were higher than 0.8. The evolution trend of scan number per year was assessed using a linear regression considering time and scan number as continuous covariates. All the analyses were performed usng stata 14.2
Results
Three hundred and thirty-nine patients admitted with acute right lower quadrant abdominal pain underwent abdominal US and/or CT. US was performed in 278 patients (278/339, 82%), of whom 91 also had a CT (91/278, 31%). CT was performed as a first-line examination in 61 patients (61/339, 18%). The median BMI of our population was 24.7 kg/m2.
Between 2012 and 2021, the use of CT as a first-line examination (compared to US) increased significantly (p < 0.0001) (Fig. 1). CT was performed as a first-line in 0/15 in 2012, in 3/31 in 2016 and in 13/58 in 2021 (Table 1).
Management failure
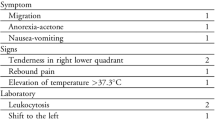
Three-hundred and thirty patients had appendicitis. Ten patients (10/339, 3%) had management failure. A higher median of age and CT and US + CT were associated with the management failure (p = 0.001 and p = 0.001 respectively) (Table 2). One of the patients did not undergo surgery, although both US and CT concluded “appendiceal plastron”. This patient was hospitalized and then discharged, before to be readmitted to emergency department with surgery on the second admission.
The other nine patients with management failure were operated on because of the radiological diagnosis of acute appendicitis but the final diagnosis (surgical or pathological) was no appendicitis with postoperative diagnosis of pyelonephritis (n = 1), no appendicitis (surgical diagnosis) with a diagnosis of chronic appendicitis by the pathologist (n = 2), cholecystitis (n = 3), small bowel obstruction (n = 1), left sided diverticulitis (n = 1) and peritonitis due to small bowel perforation (n = 1).
US and CT accuracy
The sensitivity and specificity of US as a first-line examination were 84.8% (IC95%:76.2–91.3) and 93.2% (IC95%:88.1–96.5), respectively. The sensitivity and specificity of CT as a first-line examination were 100% (IC95%:86.8–100) and 87.9% (IC95%:71.8–96.6), respectively. The sensitivity of CT as a first-line examination was significantly higher than that of US (p = 0.03). The specificities were similar (p = 0.29). The sensitivity and specificity of CT as a second-line examination were 100.0% (IC95%:83.9–100) and 92.5% (IC95%:83.4–97.5), respectively. Sensitivity and specificity were similar between first-line and second-line CT (p = NS and p = 0.45, respectively). When CT was used as the first-line examination, no further imaging was performed.
Length of stay in the emergency department
The mean length of stay was 522 min ± 251) for patients undergoing only US and 515 min (± 264) for patients undergoing only CT (p = 0.85).
When patients underwent an additional CT-scan performed as a second-line examination after US, the mean length of stay was increased (618 min ± 272) (p < 0.0001 compared to patients undergoing US alone).
Patients’ orientation after the emergency department
Of the 339 patients, 143 underwent surgery (143/339, 42%) and 196 did not (196/339, 58%). One hundred and thirty-six patients (136/339, 40%) were discharged from the ED, 51 patients (51/339, 15%) were immediately transferred from the ED to the theater and 152 patients were transferred into surgery wards (152/339, 45%). Of the latter, 92 (92/152, 60%) underwent surgery after admission to the ward (Table 3).
Thirty patients had a positive CT for appendicitis and 26 (26/30, 87%) underwent surgery. Twenty-nine patients had a negative CT for appendicitis and 16 were discharged (16/29, 55%) (Fig. 2A). When US was performed as a first-line examination, 75/165 (45%) patients with negative examination were discharged and 71/165 (43%) patients underwent further CT (Fig. 2B). Appendicitis was diagnosed by US in 95 patients, 80 of whom underwent surgery (80/95, 84%). Of these patients, 7 of them (7/95, 7%) underwent second-line CT (Fig. 2C). Eighteen patients had a negative or inconclusive final radiology report, of whom 13 (13/18, 72%) underwent second-line CT (Fig. 2D).
Patients’ disposition after the emergency department. A If the first examination was a CT. B If the first examination was an US and concluded “no appendicitis”. C If the first examination was an US and concluded “appendicitis”. D If the first examination was an US that was inconclusive. CT-scan computed tomography scan, US ultrasonography
Discussion
This retrospective study included 339 patients over a ten-year period who underwent US and/or CT for suspected acute appendicitis. US was performed as a first-line examination in 278 patients (82%) and CT in 61 patients (18%). The sensitivities of US and CT were 84.8% and 100%, respectively; and the specificities were 93.2% and 87.9%. Although the sensitivity was significantly higher for CT, the use of CT versus US for the non-invasive diagnosis of appendicitis was a risk factor for management failure (management failure rate was 3% in our study). Ninety-one patients (31%) had a second-line CT after US. The use of CT increased significantly from 2012 to 2021. The conclusions of both US and CT were more likely to be to be considered for the subsequent management when positive. The majority of negative or inconclusive reports lead to hospitalization or second-line examination (CT).
Investigation of suspected appendicitis varies between countries, with 32.8% of preoperative imaging in the UK compared to 99.5% in the Netherlands [8]. Similar national recommendations lead to similar management. Indeed, recommendations are similar between France and the Netherlands, and our results in the first period (2012–2018) are in line with those of the Netherlands, with US performed as a first-line and single examination in 73% of the patients and combined US + CT in 21% [8]. It also leads to similar management failures, with a similar rate of initial misdiagnosis of ‘appendicitis’ with a normal-appearing appendix at surgery (3%). This rate is much lower than in countries without systematic preoperative imaging (6.2 to 20%) [3, 8, 9]. Interestingly, this rate was also very high in the Netherlands (22%) before the recommendation for systematic preoperative imaging [5, 8]. In our cohort study, the higher rate of CT is reported in 2020 in our cohort study. This difference is probably explained by the emergence of the coronavirus disease 19 (COVID 19). Indeed, there was an abrupt change in clinical practice guidelines and new hygiene protocols to reduce contact person-to-person contact. As a result, CT was often preferred as a first line examination [10, 11].
Secondly, we wanted to assess the risk factors for management failure. Surprisingly, the use of CT was associated with higher management failure. This may be due to the fact that, in our cohort, the most of the appendicitis described by CT underwent surgery despite a specificity between 87.9 and 92.5% while appendicitis described by the US were or confirmed by a CT or admitted in a specialized department. This difference regarding the confidence with the examination is probably due to the belief that US is less reliable than CT to diagnose normal appendix [12].
Also, we reported that a greater age was associated with the risk for management failure. A recent study reported that both female gender and age ≤ 40 years old were risk factors for a normal appendix at surgery [9]. However, the patients in this study did not undergo systematic preoperative imaging. In addition, the study confirms that a positive US or CT for appendicitis does indeed reduce the risk of a normal appendix at surgery (OR = 0.04, p < 0.01 and OR = 0.07, p < 0.01, respectively) [9].
Third, US has long been considered the first-line examination for the non-invasive diagnosis of appendicitis worldwide due to its wide and easy availability, cost-effectiveness, and the absence of radiation and contrast media side-effects [13]. Indeed, our study confirms the very good diagnostic accuracy of US. US should definitely remain the first choice in paediatric patients because of its radiation-free characteristics. However, the use of CT as a first-line examination can also be considered in adult patients. Our study showed that there was no difference in the length of stay in the ED whether the patient underwent US or CT as a first-line examination. This highlights the similar availability of CT compared to US in the ED. The LOCAT group recently showed that the use of low-dose CT compared with standard-dose CT in adolescents and young adults significantly reduced the radiation dose (to 2 mSv) without impairing clinical outcomes [14]. This has been confirmed by subsequent studies with similar results and mean radiation doses for low-dose CT of 3 to 3.33 mSv [15, 16]. These low radiation doses are approximately equivalent to one year of natural radiation, which has a more than acceptable risk–benefit ratio. The remaining issue is the intravenous contrast injection, with one case of anaphylaxis to iodinated contrast material in the study, which was a life-threatening adverse event. Finally, diagnostic accuracy of US has been found to vary a lot in the literature.
US and CT had similar specificities but different sensitivities in our cohort. The radiological conclusions were more likely to be considered for the subsequent management if they were positive. Patients were more likely to be discharged after negative CT than after a negative US. The majority of the patients with negative or inconclusive radiological reports were admitted to the surgical wards and either underwent a second-line examination and/or had subspecialized clinical reassessment [17]. Because of this management, the high specificity of US and CT is more important than the sensitivity.
Our study has some bias because of its retrospective nature. Some relevant characteristics such as body mass index were not collected. This may have affected the results, but our study was designed to be representative of the general population of patients with AA in our center. Then, only patients with preoperative imaging were included in the cohort. This probably improved the results of the management, but also has the advantage of showing the outcome in the centre with systematic preoperative imaging. Finally, we weren’t able to do a cost-effectiveness analysis because the information about the different cost were not provided for. US has previously been reported in the literature to be more cost-effective than CT [18]. Overall, the use of imaging for the non-invasive diagnosis of appendicitis is cost-effective by reducing the number of negative appendectomies [19].
Conclusion
The systematic use of US or CT for the preoperative non-invasive diagnosis of appendicitis reduces the rate of management failure. Both US and CT have excellent diagnostic accuracy. If available, US should probably be performed as a first-line examination in patients with suspected for acute appendicitis. Considering the advantages of US (radiation-free, injection-free), this approach is particularly interesting for non-obese patients in large centers were both CT and US are available as there is a failure rate of US.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AA:
-
Acute appendicitis
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- ED:
-
Emergency department
- HAS:
-
French health authority
- US:
-
Ultrasonography
- WSES:
-
World society of emergency surgery
References
Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT (2017) Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 386(10000):1278‑87.
Cervellin G, Mora R, Ticinesi A, Meschi T, Comelli I, Catena F, et al (2016) Epidemiology and outcomes of acute abdominal pain in a large urban Emergency Department: retrospective analysis of 5340 cases. Ann Transl Med 4(19):362.
Bhangu A (2020) Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg 107(1):73‑86.
Henriksen SR, Christophersen C, Rosenberg J, Fonnes S (2023) Varying negative appendectomy rates after laparoscopic appendectomy: a systematic review and meta-analysis. Langenbecks Arch Surg 408(1):205.
van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA (2008) Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology 249(1):97‑106.
Appendicectomie : Eléments décisionnels pour une indication pertinente - Rapport d’évaluation. Haute Autorité de Santé. https://www.has-sante.fr/jcms/c_1218019/fr/appendicectomie-elements-decisionnels-pour-une-indication-pertinente-rapport-d-evaluation
Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, et al (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15(1):27.
van Rossem CC, Bolmers MDM, Schreinemacher MHF, Bemelman WA, van Geloven A A. W, Pinkney TD, et al (2016) Diagnosing acute appendicitis: surgery or imaging? Colorectal Dis 18(12):1129‑32.
Chaochankit W, Boocha A, Samphao S (2022) Negative appendectomy rate in patients diagnosed with acute appendicitis. BMC Surg 22(1):404.
English W, Habib Bedwani N, Smith C, Doganay E, Marsden M, Muse S, et al (2021) Suspected appendicitis and COVID-19, a change in investigation and management-a multicentre cohort study. Langenbecks Arch Surg 406(2):357‑65.
Collins BW, Robart A, Lockyer EJ, Fairbridge NA, Rector T, Hartery A (2023) Effect of the COVID-19 pandemic on emergency department utilization of computed tomography scans of appendicitis and diverticulitis. Emerg Radiol 30(3):297‑306.
Kim DW, Suh CH, Yoon HM, Kim JR, Jung AY, Lee JS, et al (2018) Visibility of normal appendix on CT, MRI, and sonography: a systematic review and meta-analysis. AJR Am J Roentgenol 211(3):W140‑50.
Hwang ME (2018) Sonography and computed tomography in diagnosing acute appendicitis. Radiol Technol 89(3):224‑37.
LOCAT Group (2017) Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): a pragmatic, multicentre, randomised controlled non-inferiority trial. Lancet Gastroenterol Hepatol 2(11):793‑804.
Sippola S, Virtanen J, Tammilehto V, Grönroos J, Hurme S, Niiniviita H, et al (2020) The accuracy of low-dose computed tomography protocol in patients with suspected acute appendicitis: the OPTICAP study. Ann Surg 271(2):332‑8.
Haijanen J, Sippola S, Tammilehto V, Grönroos J, Mäntyoja S, Löyttyniemi E, et al (2021) Diagnostic accuracy using low-dose versus standard radiation dose CT in suspected acute appendicitis: prospective cohort study. Br J Surg 108(12):1483‑90.
Lloyd AJ, Boland MR, Cleere E, Fallon F, Toale J, Hill ADK (2023) Assessing clinical acumen in predicting acute appendicitis in emergency surgery: a prospective study. World J Surg 47(4):922‑7.
D’Souza N, Marsden M, Bottomley S, Nagarajah N, Scutt F, Toh S (2018) Cost-effectiveness of routine imaging of suspected appendicitis. Ann R Coll Surg Engl 100(1):47‑51.
Jennings R, Guo H, Goldin A, Wright DR (2020) Cost-effectiveness of imaging protocols for suspected appendicitis. Pediatrics 145(2):e20191352.
Acknowledgements
The authors want to acknowledge France Blandignère and Sybille de Vanssay de Blavous for their kind help in the collection of the data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Guarantor of integrity of the entire study: A Venara. Study concepts and design: Paisant A, Faroche E, Aube C, Fouche A, Legrand A, Aube C, Hamel JF, Venara A. Literature research: Paisant A, Fouche A, Legrand A, Venara A. Experimental studies / data analysis: Paisant A, Faroche E, Aube C, Fouche A, Legrand A, Aube C, Hamel JF, Venara A. Statistical analysis: Hamel JF, Venara A. Manuscript preparation: Paisant A, Hamel JF, Venara A. Manuscript editing: Paisant A, Faroche E, Aube C, Fouche A, Legrand A, Aube C, Hamel JF, Venara A.
Corresponding author
Ethics declarations
Competing interests
Prof. Venara declares conflicts of interest with Takeda, Coloplast, ThermoFisher, Biom’up and Sanofi-Aventis (consulting and lecture). The other authors do not declare any conflict of interest.
Ethical approval
This study was approved by the National Commission of Informatics and Freedom (CNIL) (Number ar23-0020v0).
Consent for publication
Not applicable.
Informed consent
Being a retrospective study, the consent of the patient was not collected but patients were informed that their data could be collected. Patients that did not want their data to be used were asked to manifest themselves.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paisant, A., Faroche, E., Fouche, A. et al. Time to improve the management of patients with suspected acute appendicitis: a retrospective study. Abdom Radiol (2024). https://doi.org/10.1007/s00261-024-04471-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00261-024-04471-w