Abstract
Background and aims
The placement of Transjugular intrahepatic portosystemic shunt (TIPS) results in a sudden increase in central circulating blood volume, which requires proper regulation of the cardiovascular system. We aimed to investigate the impact of TIPS on cirrhotic cardiomyopathy (CCM).
Method
A consecutive case series of patients with cirrhosis who underwent TIPS were evaluated by echocardiography and pressure measurements before, immediately after TIPS and 2–4 days later (delayed). Furthermore, all patients underwent a one-year follow-up.
Results
In this study, 107 patients were enrolled, 38 (35.5%) with CCM. Echocardiography revealed an increase in postoperative left ventricular filling pressure accompanied by an elevation in left ventricular ejection fraction (LVEF). However, patients in the CCM group exhibited lower LVEF and mean arterial pressure (MAP) compared to the non-CCM group. Post-TIPS, CCM patients showed increased right atrium pressure (RAP) that normalized within 2–4 days, whereas non-CCM patients had lower RAP than baseline. Compared to patient without CCM, CCM patients revealed lower immediate (16.7 ± 4.4 vs. 18.9 ± 4.8, p = 0.022) and delayed 15.9 ± 3.7 vs. 17.7 ± 5.3, p = 0.044) portal vein pressures (PVP) and portal pressure gradients (PPG) (7.7 ± 3.4 vs. 9.2 ± 3.6, p = 0.032 and 10.1 ± 3.1 vs. 12.3 ± 4.9, p = 0.013). The 1-year mortality rates were 13.2% for CCM patients and 4.3% for non-CCM patients (log-rank test, p = 0.093), with MELD score, and preoperative RAP significantly associated with the mortality.
Conclusion
Cirrhotic patients with CCM exhibit lower PVP and PPG immediately after TIPS and 2–4 days later, without significantly impacting one-year survival outcomes.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Portal hypertension-related complications are the leading cause of mortality among patients with cirrhosis [1]. Transjugular intrahepatic portosystemic shunt (TIPS) is a commonly used method for managing portal hypertension, effectively reducing the portal pressure gradient (PPG) [2,3,4]. However, TIPS placement results in a sudden increase in central circulating blood volume [5, 6], which requires precise regulation of the cardiovascular system. Unfortunately, the cardiovascular autoregulatory capacity is impaired in the presence of myocardial dysfunction, potentially leading to adverse outcomes [7, 8].
Cirrhotic cardiomyopathy (CCM) constitutes a unique form of cardiac dysfunction characterized by hyperdynamic circulation, elevated cardiac output, and reduced systemic vascular resistance in cirrhotic patients [9,10,11]. The Cirrhotic Cardiomyopathy Consortium (CCC) recently proposed a standardized algorithm for quantifying left ventricular diastolic and systolic function using multiple echocardiographic parameters in patients with end-stage liver disease [9]. Prior research has indicated that CCM prevalence ranges from 27.5 to 34.7% in populations predominantly diagnosed with alcoholic cirrhosis [8, 12,13,14]. However, data regarding patients primarily affected by hepatitis B virus (HBV) infection remains limited. Latent cardiac dysfunction may lead to unfavorable outcomes during abrupt hemodynamic shifts due to TIPS or liver transplantation. Furthermore, impaired cardiac function may influence PPG and right atrium (RA) pressure measurements, potentially influencing the efficacy of TIPS [15, 16]. Nonetheless, short-term alterations in PPG and RA pressure measurements in patients with CCM following TIPS placement remain unclear. Several studies have identified diastolic dysfunction as a predictor of unfavorable outcomes in cirrhotic patients undergoing TIPS [7, 8]. However, the prognostic significance of CCM, as evaluated by the CCC algorithm in patients undergoing TIPS, has not yet been established and requires further investigation due to the limited available data.
Given this context, we conducted a prospective study with the objectives of determining whether patients with CCM can adapt to acute volume expansion induced by TIPS placement and whether CCM affects patient survival after TIPS in the short term.
Methods
Study population
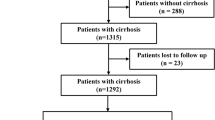
This prospective observational study was conducted between June 2020 and January 2022. A consecutive series of cirrhotic patients undergoing TIPS were prospectively evaluated. Inclusion criteria were: (1) diagnosis of liver cirrhosis, established through clinical, laboratory, imaging, or histologic analysis, (2) age between 18 and 65 years, (3) Child-Pugh score ≤ 13 and a MELD score ≤ 18. Exclusion criteria included: the patients with American College of Cardiology (ACC)/American Heart Association (AHA) Stage C or D heart failure (HF) [17] and AHA/ACC stage C or D untreated valvular heart disease(VHD) [18]; moderate-severe pulmonary hypertension; chronic/acute respiratory failure and acute renal failure; portal vein thrombosis; hepatocellular carcinoma or other malignancy; prior TIPS or liver transplantation; TIPS performed under general anesthesia; emergency TIPS without preoperative echocardiography and refusal to participate. All participants provided informed consent, and the study was approved by the Ethics Committee of Zhongshan Hospital, Fudan University (Approval No: B2020-122R).
Echocardiography
All participants underwent comprehensive echocardiography prior to (within 24 h) TIPS and 2–4 days after TIPS. Transthoracic echocardiography (TTE) was performed using a commercial ultrasound system (Vivid E95; General Electric Vingmed Ultrasound, Milwaukee, WI, USA). Images were acquired in standard parasternal and apical (apical 4, apical 2, and apical long) views at a frame rate of 50–100 frames/s, recording 3–6 cardiac cycles. Images were digitally stored for offline analysis (EchoPAC version 204; General Electric Vingmed). Mitral inflow was assessed by pulsed-wave Doppler echocardiography, with the sample volume between mitral leaflet tips during diastole. Mitral annulus velocities were obtained from the septal and lateral annulus by tissue Doppler imaging (TDI). Electrocardiogram (ECG) was continuously monitored. LVEF was calculated using the biplane Simpson method. Left atrial (LA) volume was measured from apical two- and four-chamber views using the biplane Simpson method and indexed to body surface area (BSA) (LAVi). Images from apical four- and two-chamber and long-axis views were automatically tracked throughout the cardiac cycle to measure LV global longitudinal strain (LV-GLS). Echocardiographic assessments were conducted by an experienced cardiologist. All echocardiograms were digitally archived and subjected to offline analyses on two distinct occasions. Differences were rarely found between the two measurements. In instances where variation did occur, mean values were computed to reconcile the differences.
Diagnosis CCM
In line with the updated criteria from the Cirrhotic Cardiomyopathy Consortium (CCC), the presence of Left ventricular (LV) systolic dysfunction and/or LV diastolic dysfunction constituted a diagnosis of CCM. The systolic component of CCM was characterized as reduced LVEF (≤ 50%) or decline in LV-GLS (absolute value < 18). The diastolic component was defined by having at least 3 of the following: E/e’ (using the medial e’) ratio ≥ 15, left atrial volume index (LAVI) greater than 34 mL/m2, septal early diastolic tissue velocity (septal e’) less than 7 cm/s, or tricuspid regurgitation velocity (TR velocity) greater than 2.8 m/s in the absence of pulmonary hypertension [9].
TIPS procedure and related pressure measurement
TIPS was created under local anesthesia with lidocaine, and intravenous oxycodone hydrochloride was used for analgesia. Celiac arteriography was conducted via radial access using a 4-French MPA catheter (Cordis, Mexico, USA) to obtain an indirect portal venogram. DSA overlay software merged hepatic artery and portal vein images to create a portal vein puncture navigation map. After transjugular approach, the 10 F sheath was advanced into the inferior vena cava. Simply, the hepatic vein was catheterized by Rösch-Uchida transjugular liver access set (RUPS-100; Cook, Bloomington, Ind) and then the first branch of the right or left PV was punctuated. A 2.4-French microcatheter (Progreat; TERUMO, Fujinomiya City, Japan) was then inserted into the selected hepatic artery branch with its tip serving as a marker. After confirming portal vein (PV) access via contrast medium injection, a 0.035-inch, 260 cm guidewire (TERUMO, Fujinomiya City, Japan) was introduced into the splenic vein using a 4-French pigtail catheter (Cordis, Mexico, USA) for direct portal venography and portal vein pressure measurement. Based on the patient’s clinical status, an 8-millimeter balloon (RIVAL; BARD, Arizona, USA) was employed to dilate the puncture route. Subsequently, an 8-millimeter VIATORR stent (GORE VIATORR; GORE, Arizona, USA) was implanted, and an 8-millimeter balloon (RIVAL; BARD, Arizona, USA) was used for re-dilation. Post-TIPS portal venography was performed after TIPS creation, and portal pressure was measured. Hepatic arteriography was conducted to exclude hepatic artery injury, arterioportal fistula, and arteriovenous fistula. Pressure measurements were taken in the right atrium, inferior vena cava (at the hepatic vein level), and portal vein (at the confluence of splenic and superior mesenteric veins) using a 4-Fr pigtail catheter before and after stent placement, with pressure tracings permanently recorded on paper. The definition of a successful is a PPG reduction to below 12 mmHg or a decrease of more than 50%, as recommended by the guidelines. All enrolled patients met this standard. In the period of 2–4 days post-TIPS, delayed pressure measurement is conducted via the transjugular approach using a 4-Fr pigtail catheter to measure pressures in the portal vein (at the confluence of splenic and superior mesenteric veins), inferior vena cava (at the hepatic vein level), and right atrium. For all measurements, the pressure transducer was calibrated to 0 mmHg at the level of the patient’s mid-axillary line. Each measurement was performed three times and then averaged. The pressure tracings were permanently recorded on paper. In this study, PPG is defined as the pressure differences between PV and IVC. Record the patient’s blood pressure measured by arm cuff, and calculate the mean arterial pressure (MAP). Immediate and delayed PPG measurements quantify the pressure differences between the PV and IVC at the time of TIPS completion and 2–4 days afterwards, respectively. Post-TIPS, patients received symptomatic and supportive therapies until discharge.
Follow-up
Patients were followed up at months one, three, and six, and every six months thereafter, or in case of clinical relapse or events necessitating hospitalization. Telephone follow-ups were conducted between scheduled visits to prevent missing patient status or clinical event information. Each follow-up includes assessment of clinical symptoms, physical examination, laboratory tests, and survival status. If the patient dies during the follow-up period, the date and cause of death are recorded in detail. The primary study endpoint was all-cause mortality post-TIPS.
Statistical analysis
Quantitative variables were expressed as median (25th -75th) or means ± standard deviation (SD) and compared using one-way ANOVA analysis, Kruskal–Wallis tests or student t test, accordingly. Qualitative variables were presented as numbers (percentages) and compared by chi-squared test or Fisher’s exact test as appropriate. Cumulative risks were assessed with Kaplan–Meier curves and compared using the log-rank test. The independent predictors for survival were calculated using the Cox regression model. Covariates incorporated into the multivariate analysis were variables reaching statistical significance (p < 0.1) in univariate analysis. Exploratory subgroup analyses with statistical tests of interaction were performed to estimate heterogeneity in the effect of Normal and CCM on all-cause mortality in the prespecified subgroups (sex, age, BMI, etiology of cirrhosis, Child–Pugh class, ascites, pre-TIPS RAP, post-TIPS PPG). The subgroup analyses were performed using R software, version 4.2.2, along with MSTATA software (www.mstata.com). Two-tailed p-values < 0.05 were considered statistically significant.
Results
Study population and baseline characteristics
According to inclusion and exclusion criteria, 107 patients were ultimately included from June 2020 to January 2022. According to the algorithm proposed by the CCC, 38(35.5%) patients are considered CCM. Of these, 25(23.4%) patients had systolic dysfunction, while 21(19.6%) patients had diastolic dysfunction. Baseline characteristics of the study population are summarized in Table 1. We did not observe significant differences between the two groups in terms of etiology, indications, liver function, or other clinical baselines. Meanwhile, all enrolled patients underwent each hemodynamic assessment.
Effect of TIPS on cardiac function
A comparison of echocardiographic variables before and after TIPS was shown in Table 2. Patients with CCM had significantly higher peak TR velocity (2.2 ± 0.49 VS 2.65 ± 0.47 m/sec, p < 0.001) and E/e’ ratio (8.78 ± 2.16 VS 10.08 ± 2.49, p = 0.006), lower septal e’ velocity (7.9 ± 2.0 VS 5.9 ± 1.2 cm/sec, p < 0.001), LV-GLS (-21.39 ± 1.82 VS -17.6 ± 3.43%, p < 0.001) and LVEF (60.93 ± 4.71 VS 55.5 ± 3.68%, p = 0.001), and larger LAVi (35.64 ± 12.39 VS 41.08 ± 6.25 ml/m2, p = 0.001) compared to those without CCM at baseline. At 48 h after TIPS, in patients with normal cardiac function, elevations in LAVI and E/e’ ratios were concomitant with a marked rise in the E/A ratio, indicating elevated left ventricular filling pressures. Additionally, the rise in TR velocity and PASP velocity suggested increased pulmonary artery pressures attributed to the acute shift of portal venous blood into the systemic circulation. In patients with CCM, a comparable phenomenon of increased left ventricular filling pressures and pulmonary artery pressures was noted, which also significantly higher than the normal group. But MAP (80.47 ± 6.68 VS 77.75 ± 6.15 mm Hg, p = 0.040) and LVEF (61.74 ± 3.6 VS 60.13 ± 3.98%, p = 0.036) were significantly lower than normal group after TIPS.
Effect of CMM on TIPS hemodynamics and survival
Figure 1 illustrated intra-group comparison of the pressures of RA and PPG measured before stent implantation, immediately after TIPS completion (Immediate pressure), and 2–4 days after TIPS (Delayed pressure). As shown in Fig. 1, after TIPS, the normal group exhibited an immediate significant rise in RAP (Pre-RAP VS Immediate-RAP:5.7 ± 3.2mmHg VS 8.8 ± 3.2mmHg, p < 0.001) but fell below preoperative levels at 48 h (Pre-RAP VS Delay-RAP:5.7 ± 3.2mmHg VS 4.6 ± 3.1mmHg, p = 0.002). In contrast, CCM group also had an immediate rise (Pre-RAP VS Immediate-RAP:5.5 ± 2.6mmHg VS 8.5 ± 2.3mmHg, p < 0.001) but reverted to preoperative baselines within the same postoperative period (Pre-RAP VS Delay-RAP:5.7 ± 3.2mmHg VS 5.3 ± 2.2mmHg, p = 0.669). Inter-group comparisons of pressure measurement at different time are presented in Table 3 .Our results also showed that in patients with CCM, their PV pressures were significantly lower than those in the normal group, both measured in the immediate (Normal VS CCM: 18.9 ± 4.8mmHg VS 16.7 ± 4.4mmHg, p = 0.022) and delayed (Normal VS CCM: 17.7 ± 5.3mmHg VS 15.9 ± 3.7mmHg, p = 0.044), as well as PPG (Immediate-PPG Normal VS CCM: 9.2 ± 3.6 mmHg VS 7.7 ± 3.4 mmHg, p = 0.032; Delayed-PPG Normal VS CCM: 12.3 ± 4.9 mmHg VS 10.1 ± 3.1 mmHg, p = 0.013).
Intra-group comparison of the pressures of RA and PPG at different time. (A) The changes in RAP at different time points in the CCM group and the non-CCM group; (B) The changes in PPG at different time points in the CCM group and the non-CCM group. Abbreviations CCM, Cirrhotic cardiomyopathy; PPG-pre, the portal pressure gradient before stent implantation; PPG-post, the portal pressure gradient at the time of TIPS completion; PPG-del, the portal pressure gradient at 2–4 days after TIPS; RAP-pre, the right atrium pressure before stent implantation; RAP-post, the right atrium pressure at the time of TIPS completion; RAP-del, the right atrium pressure at 2–4 days after TIPS; TIPS, transjugular intrahepatic portosystemic shunt
At the end of follow-up, 8(7.5%) patients died. The 1-year probability of all-cause mortality for CCM and no-CCM groups were 13.2% and 4.3% (log-rank test, p = 0.093, HR 0.313, 95%CI [0.075–1.309]) (Fig. 2). MELD score (p = 0.014, HR = 2.03, 95%CI [1.156–3.561]) and preoperative RAP (p = 0.003, HR = 1.66, 95%CI [1.188–2.323]) were significantly associated with the mortality in multivariate Cox proportional hazard model, which adjusted by age (Table 4). In a subgroup analysis, we did not find any evidence of heterogeneity in the effect of Normal vs. CCM on all-cause mortality across the subsets (Fig. 3). Causes of death were Sepsis/pneumonia(n = 3), hepatic failure(n = 3), cardiac failure(n = 2). Notably, all cases of cardiac failure were observed in CCM group. However, due to the limited sample size, no statistically significant conclusions could be drawn from these findings (Normal VS CCM: 0% VS 5.3%, p = 0.124).
Forest plots showing the effects of Normal vs. CCM in subgroups on the all-cause mortality after TIPS. Abbreviations CCM, Cirrhotic cardiomyopathy; CI, confidence interval; HR, hazard ratio; PPG, portal pressure gradient; RAP, right atrium pressure; TIPS, transjugular intrahepatic portosystemic shunt
Discussion
Our findings indicate that patients maintained effective regulated hemodynamic alterations induced by TIPS in the short term, with the CCM group showing a lower PVP and PPG immediately after TIPS and 2–4 days later. Additionally, CCM did not serve as independent prognostic factors for one-year all-cause mortality post-TIPS.
Our study revealed a 35.5% incidence of CCM, similar to previous findings (27.5–34.7%) [8, 12]. Research to date, predominantly from Europe and North America, focuses on alcoholic cirrhosis as the primary cause, leaving the prevalence among hepatitis B as the primary etiology populations less defined. As the patients enrolled in our study were decompensated cirrhosis the true incidence of CCM may potentially be higher than the reported result. However, since our study had a relatively small sample size, multicenter and larger-scale studies are needed to examine whether the incidence of CCM varies across different liver diseases.
TIPS-induced acute volume expansion is noteworthy as it may negatively impact short-term hyperdynamic circulation, requiring cardiac and renal function compensation [19, 20]. CCM is especially characterized by the inability to increase ejection fraction adequately due to blunted contractility as a response to stress. Impaired myocardial contractility may affect organ perfusion, which might development the organ failure, acute-on‐ chronic liver failure and death, as well as further affecting the efficacy of TIPS. Comparing the postoperative cardiac function changes between the two groups, we found that patients with cardiac dysfunction exhibited higher left ventricular filling pressures on days 2–4 post-TIPS.RAP changes were immediately apparent after TIPS, showing an initial increase, followed by a decrease to preoperative levels within 2–4 days, whereas in the normal group, it dropped below the preoperative baseline levels, despite no significant differences in RAP at any measured time point across both groups. Additionally, our results also indicate that patients with cardiac dysfunction showed lower PVP immediately after TIPS and 2–4 days later. The postoperative echocardiography results also indicated an increase in LV-GLS synchronicity with LVEF, an elevation attributed to the increased cardiac load. However, the postoperative LVEF and MAP were significantly lower than those in the no-CCM group, suggesting a blunted response to volume changes in the CCM group. This pattern of increased central venous pressure (elevated preload) and decreased visceral blood supply (reduced afterload) leads to a comparatively lower PPG. These observations align with theories previously put forth by Rössle, M et al. [16], underscoring the complex interplay between cardiac function and portal hemodynamics postoperatively. Additionally, previous research indicates that a lower delayed PPG is associated with a reduced risk of rebleeding [21]. But researches also demonstrated that post-TIPS PPGs under 5 mmHg or reductions over 60% significantly escalate low-pressure gradient complications (e.g., hepatic encephalopathy, acute liver failure), detrimentally influencing patient prognosis [22, 23]. Meanwhile, it must also be acknowledged that the hemodynamic changes after TIPS are influenced by multiple factors, with cardiac regulation being just one aspect. It remains unclear whether patients require a longer period to achieve a more stable hemodynamic state. The role and impact of cardiac regulation in the process of postoperative hemodynamic alterations require further, more in-depth research.
There is limited research using the 2019 CCC algorithm to investigate the impact of CCM on survival post-TIPS. Our study suggested that the presence of CCM did not affect survival up to one years after TIPS. A study with long-term follow‐up and the comprehensive clinical and echocardiographic assessments similarly showing that diastolic dysfunction does not predict survival after TIPS [24]. However, it has also been shown that diastolic and systolic dysfunction affect survival after TIPS, contrary to our finding [7, 8]. The reasons for this difference may be the following. Firstly, in prior research, alcoholic cirrhosis was predominantly the main etiological factor for cirrhosis, whereas in our study, HBV infection serves as the principal cause. Alcohol consumption can detrimentally affect cardiac function, potentially resulting in confounding factors due to alcoholic cardiomyopathy in the outcomes of these investigations [25, 26]. Secondly, our study population may exhibit better liver function, with the degree of liver function severity being intricately connected to the prognosis following TIPS treatment. Thirdly, in China, shunts with an 8 mm diameter are commonly utilized, in contrast to the West, where larger diameter shunts are typically employed. This leads to an increased volume of blood flow diverted directly from the portal system into the systemic circulation, potentially imposing a greater cardiac burden and exacerbating liver dysfunction [5, 16, 27]. Finally, our results also demonstrate that patients without CCM exhibited a higher survival rate, although there was no significant statistical difference between the two groups. This may be attributed to the relatively small number of patients with CCM included in our study, necessitating larger sample sizes for validation. These factors might account for the observed discrepancies between our research outcomes and those of previous investigations. Comparing the baseline levels of the two groups of patients, it is evident that there are no significant differences in age, gender, etiology, liver function, etc., between the groups. Furthermore, the baseline levels of the enrolled patients are also similar to those from other large prospective cohort studies in China [28, 29]. Our study also paid particular attention to this point, and these factors were analysed in subgroups in the results, which showed homogeneous across subgroups. Our findings also demonstrated that higher RAP was associated with overall mortality in patients undergoing TIPS, consistent with prior research [20]. Increased RAP can elevate back pressure in the liver, be linked to heart failure, and limit TIPS efficacy in reducing the PPG [20, 30, 31], which may affect the prognosis of patients.
Our study has several limitations. Firstly, it was an observational single-center prospective cohort study. Therefore, further validation through multi-center, large population, and prospective studies is necessary. Secondly, as most patients had cirrhosis due to HBV, the generalizability of the findings is limited. Thirdly, our study does not provide insights into long-term cardiac outcomes post-TIPS, necessitating further research to elucidate whether TIPS exacerbates or ameliorates cardiac function over a longer follow-up period. Finally, we did not perform cardiac catheterization to obtain additional hemodynamic information, which could help elucidate the hemodynamic changes caused by TIPS and their impact on patients with CCM.
In conclusion, cirrhotic patients with CCM exhibit lower PVP and PPG immediately after TIPS and 2–4 days later in response to hemodynamic alterations elicited by TIPS, without adversely impacting one-year survival outcomes. These findings need to be further investigated the long-term effects and the corresponding clinical course of the patients.
Data availability
Data available on request from the authors.
Abbreviations
- ALBI:
-
Albumin – bilirubin
- BMI:
-
Body mass index
- CCC:
-
Cirrhotic Cardiomyopathy Consortium
- CI:
-
Confidence interval
- CCM:
-
Cirrhotic cardiomyopathy
- CK-MB:
-
Creatine kinase-MB
- E / A:
-
Early maximal ventricular filling velocity / atrial maximal filling velocity
- HR:
-
Hazard ratio
- HBV:
-
Hepatitis B virus
- INR:
-
International normalized ratio
- IVC:
-
Inferior vena cava
- LAVi:
-
Left atrial volume indexed
- LV:
-
Left ventricular
- LVDD:
-
Left ventricular diastolic dysfunction
- LVEF:
-
Left ventricular ejection fraction
- LV-GLS:
-
Left ventricular global longitudinal strain
- MAP:
-
Mean arterial pressure
- MELD:
-
Model for end-stage liver disease
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- PPG:
-
Portal pressure gradient
- PV:
-
Portal vein
- RA:
-
Right atrium
- Septal e’:
-
Septal early diastolic tissue velocity
- TR:
-
Tricuspid regurgitation
- TIPS:
-
Transjugular intrahepatic portosystemic shunt
References
Mokdad AA, Lopez AD, Shahraz S et al (2014) Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med 12:145
Ochs A, Rossle M, Haag K et al (1995) The transjugular intrahepatic portosystemic stent-shunt procedure for refractory ascites. N Engl J Med 332:1192–1197
Rossle M, Haag K, Ochs A et al (1994) The transjugular intrahepatic portosystemic stent-shunt procedure for variceal bleeding. N Engl J Med 330:165–171
Garcia-Pagan JC, Caca K, Bureau C et al (2010) Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med 362:2370–2379
Saugel B, Mair S, Meidert AS et al (2014) The effects of transjugular intrahepatic portosystemic stent shunt on systemic cardiocirculatory parameters. J Crit Care 29:1001–1005
Huonker M, Schumacher YO, Ochs A, Sorichter S, Keul J, Rossle M (1999) Cardiac function and haemodynamics in alcoholic cirrhosis and effects of the transjugular intrahepatic portosystemic stent shunt. Gut 44:743–748
Billey C, Billet S, Robic MA et al (2019) A Prospective Study Identifying Predictive Factors of Cardiac Decompensation After Transjugular Intrahepatic Portosystemic Shunt: The Toulouse Algorithm. Hepatology 70:1928–1941
Meucci MC, Hoogerduijn Strating MM, Butcher SC et al (2022) Left atrial dysfunction is an independent predictor of mortality in patients with cirrhosis treated by transjugular intrahepatic portosystemic shunt. Hepatol Commun 6:3163–3174
Izzy M, VanWagner LB, Lin G et al (2020) Redefining Cirrhotic Cardiomyopathy for the Modern Era. Hepatology 71:334–345
Møller S, Henriksen JH (2010) Cirrhotic cardiomyopathy. J Hepatol 53:179–190
Izzy MJ, VanWagner LB (2021) Current Concepts of Cirrhotic Cardiomyopathy. Clin Liver Dis 25:471–481
Razpotnik M, Bota S, Wimmer P et al (2021) The prevalence of cirrhotic cardiomyopathy according to different diagnostic criteria. Liver Int 41:1058–1069
Jansen C, Schroder A, Schueler R et al (2019) Left Ventricular Longitudinal Contractility Predicts Acute-on-Chronic Liver Failure Development and Mortality After Transjugular Intrahepatic Portosystemic Shunt. Hepatol Commun 3:340–347
Ruiz-del-Arbol L, Achecar L, Serradilla R et al (2013) Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology 58:1732–1741
Filì D, Falletta C, Luca A et al (2015) Circulatory response to volume expansion and transjugular intrahepatic portosystemic shunt in refractory ascites: Relationship with diastolic dysfunction. Dig Liver Dis 47:1052–1058
Rössle M, Bettinger D, Thimme R, Schultheiss M (2023) The transjugular intrahepatic portosystemic shunt: Smaller stent diameters are required to optimize pressure response. iLIVER 2:89–96
Yancy CW, Jessup M, Bozkurt B et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62:e147-239
Otto CM, Nishimura RA, Bonow RO et al (2021) 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143:e72-e227
Pitton MB, Weinmann A, Kloeckner R et al (2022) Transjugular Portosystemic Stent Shunt: Impact of Right Atrial Pressure on Portal Venous Hemodynamics Within the First Week. Cardiovasc Intervent Radiol 45:102–111
Bommena S, Mahmud N, Boike JR et al (2023) The impact of right atrial pressure on outcomes in patients undergoing TIPS, an ALTA group study. Hepatology 77:2041–2051
Ma L, Ma J, Zhang W et al (2023) Predictive power of portal pressure gradient remeasured shortly after transjugular intrahepatic portosystemic shunt. Hepatol Int 17:417–426
Ma L, Ma J, Zhang W, Luo J (2021) Acute Hepatic Ischemia after Transjugular Intrahepatic Portosystemic Shunt Creation Despite Preserved Arterial Perfusion. J Vasc Interv Radiol 32:1510–1512
Chung HH, Razavi MK, Sze DY et al (2008) Portosystemic pressure gradient during transjugular intrahepatic portosystemic shunt with Viatorr stent graft: what is the critical low threshold to avoid medically uncontrolled low pressure gradient related complications? J Gastroenterol Hepatol 23:95–101
Armstrong MJ, Gohar F, Dhaliwal A et al (2019) Diastolic dysfunction on echocardiography does not predict survival after transjugular intrahepatic portosystemic stent-shunt in patients with cirrhosis. Aliment Pharmacol Ther 49:797–806
Milić S, Lulić D, Štimac D, Ružić A, Zaputović L (2016) Cardiac manifestations in alcoholic liver disease. Postgrad Med J 92:235–239
Abrahamovych M, Tolopko S, Farmaha M, Ferko M, Bilous Z (2020) Criteria for diagnosis of cardiomyopathy in patients with alcoholic liver cirrhosis before the onset of heart damage clinical signs. Georgian Med News:81–85
Boike JR, Thornburg BG, Asrani SK et al (2022) North American Practice-Based Recommendations for Transjugular Intrahepatic Portosystemic Shunts in Portal Hypertension. Clin Gastroenterol Hepatol 20:1636–1662 e1636
Lv Y, Chen H, Luo B et al (2022) Transjugular intrahepatic portosystemic shunt with or without gastro-oesophageal variceal embolisation for the prevention of variceal rebleeding: a randomised controlled trial. Lancet Gastroenterol Hepatol 7:736–746
Lv Y, Chen H, Luo B et al (2022) Concurrent large spontaneous portosystemic shunt embolization for the prevention of overt hepatic encephalopathy after TIPS: A randomized controlled trial. Hepatology 76:676–688
La Mura V, Abraldes JG, Berzigotti A et al (2010) Right atrial pressure is not adequate to calculate portal pressure gradient in cirrhosis: a clinical-hemodynamic correlation study. Hepatology 51:2108–2116
Ma L, Liu Y, Yan Z et al (2023) Comparing the predictive ability of portoatrial and portocaval gradient after transjugular intrahepatic portosystemic shunt creation for variceal rebleeding. J Gastroenterol 58:494–502
Acknowledgements
Not applicable.
Funding
This study was supported by grants from Device development exploration project from National Clinical Research Center for Interventional Medicine (2021-001), Shanghai key clinical specialty construction program (W2019028), Excellent youth program from Zhongshan Hospital, Fudan University (2019ZSYXQN38), Clinical research special fund from Zhongshan Hospital, Fudan University (2018ZSLC23), National Natural Science Foundation of China (82302323).
Author information
Authors and Affiliations
Contributions
Cuizhen Pan and Jianjun Luo contributed to the study conception and design. Material preparation and data collection were performed by Jingqin Ma, Wen Zhang, Jiaze Yu, Yongjie Zhou, Wuxu Zuo, Zhiping Yan, Cuizhen Pan and Jianjun Luo. Data analysis and interpretation were performed by Yaozu Liu, Fangmin Meng, Wen Zhang and Jianjun Luo. The first draft of the manuscript was written by Yaozu Liu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
The protocol of this study was approved by the ethics committee of Zhongshan hospital, Fudan university (No. B2020-122R). This study was conducted in accordance with the Helsinki Declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Yaozu Liu, Fangmin Meng, Jingqin Ma, Wen Zhang, Jiaze Yu, Yongjie Zhou, Wuxu Zuo, Zhiping Yan, Cuizhen Pan and Jianjun Luo declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Y., Meng, F., Ma, J. et al. Unveiling the impact of cirrhotic cardiomyopathy on portal hemodynamics and survival after transjugular intrahepatic portosystemic shunt: a prospective study. Abdom Radiol 49, 3507–3516 (2024). https://doi.org/10.1007/s00261-024-04446-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-024-04446-x