Abstract
Purpose
Non-operative management of hepatic trauma with adjunctive hepatic arterial embolization (HAE) is widely accepted. Despite careful patient selection utilizing CTA, a substantial proportion of angiograms are negative for arterial injury and no HAE is performed. This study aims to determine which CT imaging findings and clinical factors are associated with the presence of active extravasation on subsequent angiography in patients with hepatic trauma.
Materials and methods
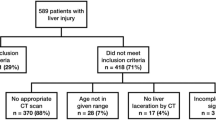
The charts of 243 adults who presented with abdominal trauma and underwent abdominal CTA followed by conventional angiography were retrospectively reviewed. Of these patients, 49 had hepatic injuries on CTA. Hepatic injuries were graded using the American association for the surgery of trauma (AAST) CT classification, and CT images were assessed for active contrast extravasation, arterial pseudoaneurysm, sentinel clot, hemoperitoneum, laceration in-volving more than 2 segments, and laceration involving specific anatomic landmarks (porta hepatis, hepatic veins, and gallbladder fossa). Medical records were reviewed for pre- and post-angiography blood pressures, hemoglobin levels, and transfusion requirements. Angiographic images and reports were reviewed for hepatic arterial injury and performance of HAE.
Results
In multivariate analysis, AAST hepatic injury grade was significantly associated with increased odds of HAE (Odds ratio: 2.5, 95% CI 1.1, 7.1, p = 0.049). Univariate analyses demonstrated no significant association between CT liver injury grade, CT characteristics of liver injury, or pre-angiographic clinical data with need for HAE.
Conclusion
In patients with hepatic trauma, prediction of need for HAE based on CT findings alone is challenging; such patients require consideration of both clinical factors and imaging findings.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-operative management (NOM) is the current standard of care for hemodynamically stable adult patients with blunt hepatic trauma [1,2,3]. Over 95% of blunt hepatic trauma patients receive NOM, and though not as widely accepted, NOM is also effective for a subset of patients with penetrating hepatic trauma [4, 5]. Hepatic arterial embolization (HAE) is widely accepted as an adjunct to NOM in hepatic trauma and included within societal practice guidelines [3, 6]. HAE is highly effective for control of active arterial bleeding, achieving angiographic evidence of cessation in 87% of patients [2].
The success of NOM and adjunctive HAE is dependent upon effective patient selection. Current guidelines recommend consideration of angiography with possible embolization in hemodynamically stable patients with evidence of active contrast extravasation on CT scan [3, 6, 7]. Close observation with planned HAE in the setting of clinical deterioration may also be an option, provided that the facility has adequate staffing and expertise [6]. A substantial proportion of angiograms for blunt hepatic trauma, ranging from 21 to 75%, are negative for extravasation [2, 8, 9]. Even the presence of contrast blush on CT, generally regarded as a highly predictive of active bleeding, has a positive predictive value of only 57–64% when correlated with angiography or surgery [2, 9, 10]. Despite the reliance on CT for triage of hepatic trauma patients, there are few prior studies which investigate the ability of CT imaging findings and CT hepatic injury grading to predict active bleeding, with mixed results [9, 11].
This study aims to determine which CT imaging findings and clinical factors are associated with the presence of active extravasation on subsequent angiography in patients with hepatic trauma. Specifically, we evaluated for (1) the association between CT injury grading of hepatic trauma and need for embolization; (2) the association between CT imaging characteristics related to hepatic trauma and need for embolization; (3) the association between pre-angiogram clinical data and need for embolization; and (4) the sensitivity of CT for detecting arterial extravasation or pseudoaneurysm, using angiography as the gold standard.
Materials and methods
This retrospective study was approved by the Institutional Review Board and is compliant with the Health Insurance Portability and Accountability Act. Written informed consent was waived.
The charts of 243 adult patients who presented to the emergency departments of two Level 1 trauma centers with abdominal trauma and underwent abdominal CTA and subsequent conventional angiography between January 2008 and September 2020 were reviewed. Of these patients, 49 had evidence of hepatic injury (e.g., laceration, fracture) on CTA, and 37 had clinical data available (male, 23; mean age, 36.8; age range, 18–80 years). HAE was performed at the time of angiography if acute arterial injury was detected. The most common mechanisms of injury were pedestrians struck by vehicles (n = 13) and falls (n = 10) (Table 1).
The available medical records of all patients were examined to collect information on pre- and post-angiography blood pressures, hemoglobin levels, and transfusion requirements, and to determine the outcomes of operative or NOM, including hospitalization length, need for repeat angiography or surgery, and death. Admission clinical values were defined as those recorded upon arrival to the emergency department. Immediate post-angiogram values were defined as the first values obtained after the conclusion of the procedure. Admission and post-angiogram clinical characteristics are summarized in Table 2. Patient outcomes, including lengths of stay and ICU admission, performance of HAE or surgical re-intervention, death, and discharge destination are provided in Table 3.
All initial abdominal CTAs were obtained within 24 h of presentation (mean, 1.0; range 0.1–3.0 h). The scans were obtained by either a Revolution HD (GE Medical Systems, Chicago, IL) or Aquilion PRIME (Canon Medical Systems, Irvine, CA). Scanning was routinely performed as per institutional trauma protocol with intravenous iodinated contrast administration using a power-injected bolus of 110 mL injected at a rate of 4 mL/sec. Initially, a uniphasic late arterial/early venous phase scan with a delay of 50 s from the time of contrast injection initiation was obtained. These initial images were reviewed by a diagnostic radiology physician, who is physically present within the CT control room at time of image acquisition. If the reviewing radiologist detected evidence of acute traumatic injury, including, but not limited to, solid organ, viscus, vascular, or musculoskeletal injury, delayed images were obtained at a scan delay of 4 min. Delayed images were obtained in 47/49 (96%) patients.
Within this study, the CTA images were reviewed and interpreted by a fellowship-trained diagnostic radiologist with 17 years of experience in emergency and trauma radiology (M.B.) and a PGY5 interventional radiology resident (K.Z.) who were blinded to the clinical, angiographic, and surgical findings. Differences in ratings were resolved through consensus discussion. This protocol included an initial grading of the injury based on the CT findings using the American Association for the Surgery of Trauma CT organ injury scale [1, 12].
CTA images were additionally assessed for the following findings: active contrast extravasation, arterial pseudoaneurysm, sentinel clot, hemoperitoneum, laceration involving more than 2 segments, and laceration involving specific anatomic landmarks (porta hepatis, hepatic veins, and gallbladder fossa). Hemoperitoneum was further graded into small (one abdominal quadrant), moderate (2–3 abdominal quadrants), and large (> 3 abdominal quadrants). On imaging, active contrast extravasation was defined as contrast blush adjacent to hepatic injury on arterial phase. If available, delayed images were assessed for enlargement of the contrast blush, confirming extravasation. If the contrast blush did not expand on delayed imaging, it was designated a pseudoaneurysm. The largest and shortest axes of extravasation were measured on the arterial phase, axial plane images, and the area of the extravasation was calculated as an ellipse based on the measured axes.
Digital subtraction angiography of the liver was performed using a digital angiographic system (Philips America Medical Systems, Andover Massachusetts or Toshiba America Medical Systems, Tustin, Calif). An initial anteroposterior celiac arteriogram was obtained to demonstrate the overall anatomy, followed by selective hepatic angiograms per the operator’s discretion. The indications for hepatic angiography included confirmation of and potential embolization for CT signs of vascular injury or contrast material extravasation, exclusion of hepatic arterial injury in patients with CT evidence of high-grade liver injury without direct CT findings of vascular injury, and exclusion of hepatic arterial injury in patients with concerning clinical findings (transient hypotension, persistent tachycardia, multiple transfusions). Hepatic angiography was performed within 12 h after CT in all but one patient (median 2.6 h; range 0.6–45.2 h). Procedures were performed by fellowship-trained, board-certified interventional radiologists (median operator experience 6 years; range 2–22 years). Selective transcatheter HAE was performed to treat hepatic arterial injuries using gelatin sponge and/or microcoils, based on operator preference.
Statistical analysis
Contingency tables were constructed to compare CTA hepatic injury characteristics and hepatic injury grade.
Univariate associations between need for HAE to treat vascular injuries seen on angiography and the following covariates were assessed, using Chi-square, simple logistic regression, or Fisher exact tests where appropriate: an ordinal variable for AAST hepatic injury grade, a numerical variable for area of contrast extravasation, and binary variables for CT characteristics of liver injury (active extravasation, pseudoaneurysm, sentinel clot, hemoperitoneum, injury involvement of > 2 segments, involvement of the hepatic veins, involvement of the gallbladder fossa, involvement of the hepatic hilum), pre-procedural shock, and pre-procedural blood transfusion requirement.
Multivariate logistic regression was additionally performed to assess the association of predetermined independent variables (AAST hepatic injury grade, pre-procedural shock, and pre-procedural blood transfusion requirement) with need for HAE. Variables with a P value of less than 0.05 were considered statistically significant. Regression analyses were repeated with the exclusion of the small subset of patients who underwent penetrating trauma as opposed to blunt trauma.
The sensitivity, specificity, positive predictive value, and negative predictive value of CT identification of active extravasation or pseudoaneurysm, with angiographic identification of active extravasation or pseudoaneurysm as the gold standard, were calculated.
Inter-reader agreement of binary CTA findings was assessed in terms of the percentage of times the readers provided concordant opinions for the same patient and using a simple kappa coefficient. The level of agreement was interpreted as poor when kappa (K) was less than zero, slight when 0 ≤ K ≤ 0.2, fair when 0.2 < K ≤ 0.4, moderate when 0.4 < K ≤ 0.6, substantial when 0.6 < K ≤ 0.8 and almost perfect when K > 0.8.
Results
Patient cohort and clinical characteristics
Demographic and clinical characteristics of the final patient cohort, including pre- and post-angiographic vital signs, laboratory data, blood transfusion requirements, and post-angiographic outcomes are presented in Tables 1, 2, 3.
Imaging characteristics
Imaging characteristics of hepatic injury extracted from CTA studies are described in Table 4. Hepatic injuries were predominantly grade 3 (43.2%) and grade 4 (35.1%). No grade 5 injuries were identified in the cohort. The majority of patients demonstrated evidence of active extravasation (59.5%) and hemoperitoneum (73.0%) on initial abdominal CTA.
Correlation of CT findings of liver injury with CT based injury grade
Injury characteristics as extracted from initial CTAs are compared with hepatic injury grade in Table 5. In patients with active extravasation, pseudoaneurysm, sentinel clot, moderate or large hemoperitoneum, and/or extension of liver laceration to > 2 hepatic segments, the hepatic veins, the gallbladder fossa, and/or the liver hilum identified on CTA, ≥ 90% had hepatic injuries of grade 3 or 4.
Risk factors for need for embolization
Univariate analyses assessing association between CT characteristics of liver injury, CT liver injury grade, and pre-angiographic clinical data to the performance of HAE are summarized in Table 6. None of the assessed risk factors were statistically significantly associated with need for HAE in univariate analyses (Figs. 1, 2). Area of contrast extravasation was also not associated with need for HAE (p = 0.22). Results did not substantially change with the exclusion of the four patients who underwent penetrating trauma.
23-year-old male pedestrian struck. a CT shows grade 4 hepatic laceration involving the hepatic vein. b More inferiorly, active extravasation is seen (arrow). c Subsequent hepatic angiogram demonstrates frank arterial extravasation (arrow) arising from a segmental branch, which was coil embolized. d Completion angiogram confirms stasis at the coil pack (arrow)
In a multivariate model, AAST hepatic injury grade was significantly associated with increased odds of HAE (Odds ratio: 2.5, 95% CI 1.1, 7.1, p = 0.049), while pre-procedural shock and pre-procedural packed red blood cell transfusion were not significantly associated with HAE. Results did not substantially change with the exclusion of the four patients who underwent penetrating trauma.
Identification of extravasation or pseudoaneurysm on CT as criteria for active bleeding
The sensitivity of active hepatic extravasation on CT for detecting active bleeding on angiography was 79%; specificity, 52%; positive predictive value, 50%; and negative predictive value, 80% (Table 7). Active extravasation on CT was not significantly associated with differences in pre-procedural vitals or transfusion requirements. For example, patients with active extravasation on CT had mean lowest pre-procedural systolic blood pressure of 93.9 (SD 24.8) mmHg versus 88.8 (SD 29.1) mmHg (p = 0.62) for patients without extravasation on CT. Similarly, patients with active extravasation on CT were transfused with mean 1.41 (SD 2.19) units of packed red blood cells prior to procedure versus 1.93 (SD 1.77) units (p = 0.38) for patients without extravasation on CT.
Inter-reader agreement
Data on inter-reader agreement are included within the supplemental data.
Discussion
This study characterizes clinical and imaging findings in patients who suffer from hepatic trauma and correlates them with performance of HAE. In multivariate analysis, AAST hepatic injury grade was associated with 2.5 times increased odds of requiring HAE, when controlling for hemodynamic shock and blood transfusion requirement, suggesting that higher hepatic injury grades as seen on CTA may help predict treatable targets on hepatic artery angiography. However, no other clinical or imaging variable was significantly associated with need for HAE, highlighting the difficulty in predicting which patients will require endovascular therapy.
At the study institutions, the selection of patients for hepatic angiography is multifactorial and depends not only on imaging findings but also on patient presentation and clinical scenario. The majority (62%) of patients within the cohort did not require HAE, even though all patients underwent hepatic angiography. While this study offers AAST hepatic injury grade as a potential variable to consider when deciding whether a patient is likely to require HAE, it is unlikely to fundamentally alter the selection of patients who are taken for hepatic angiography.
The lack of reproducibility of correlations between imaging findings and need for intervention points to the underlying difficulty of correlating CT findings to active hemodynamic processes. While nearly all (36/37) hepatic angiograms in the study cohort were performed within 12 h of the initial CT (median 2.6 h), some cases of active bleeding at the time of CT will inevitably cease by the time of angiography. Conversely, delayed bleeding may also occur. The low specificity (52%) and positive predictive value (50%) of CTA reflect this discrepancy.
Nevertheless, CTA remains a useful screening test for presence of traumatic hepatic arterial injury. Given its relatively high sensitivity (79%) and negative predictive value (80%), patients without evidence of arterial injury on CTA are unlikely to have corresponding angiographic findings or require HAE. At the study institutions, it is standard to perform angiography with possible HAE when arterial injury is found on CTA. Presence of arterial injury on CTA was not associated with a difference in pre-procedural vitals or transfusion requirements; patients who underwent angiography despite lack of arterial injury on CTA were hemodynamically unstable or did not respond adequately to transfusion. Stable patients without arterial injury on CTA that were managed conservatively without angiography were not included in this study.
Prior studies have also reported difficulty correlating CT findings with presence of arterial injury. In 2000, Poletti et al. evaluated the CT scans of 72 patients with blunt hepatic trauma [9]. Most patients (65/72) first received NOM with angiography, but several (7/72) were unstable and underwent emergent laparotomy. Ultimately, 22/72 patients had active arterial bleeding, 16 detected on angiography and 6 surgically. The presence of contrast extravasation on CTA had a low sensitivity (56%) and high specificity (83%) for arterial injury when compared to either angiographic or surgical findings. The current study utilizes only angiography as a reference standard, representing a difference in study methodology and patient acuity. Poletti et al. also used AAST grading and found statistically significant results only when CT severity grades 2 and 3 were analyzed in isolation. Though both sensitivity (100%) and specificity (94%) were high, the constraint in severity grades suggests limited predictive value of the AAST system.
In 2009, Cohn et al. evaluated the CT scans of 154 patients with blunt hepatic trauma, 21 of whom required laparotomy or HAE [11]. In contrast to the current study, a relatively small subset (59/154, 38%) of patients underwent angiography within 12 h after CT. Anatomic injury grading with the AAST criteria and a novel system developed by MacLean et al. were applied, and both were found to be poor predictors of need for surgery or HAE. AAST grades were grouped to compare grades 1–3 versus grades 4–5 injuries, which resulted in low sensitivity (32%) and high specificity (90%) [13]. Given the lesser need for invasive angiography, these values likely reflect a lower prevalence of arterial injury within the study population.
The involvement of specific anatomic landmarks and degree of hemoperitoneum on CT for blunt hepatic trauma has been suggested to correlate with need for intervention [9, 11, 13, 14]. In 2006, Fang et al. reported that CT findings of porta hepatis involvement and large volume hemoperitoneum, defined as involving all six abdominal compartments, are independently associated with need for surgery [14]. Poletti et al. reported a statistically significant association between involvement of the hepatic vein on CT and active bleeding [9]. The current study found no association between involvement of the porta hepatis or hepatic vein, or extent of hemoperitoneum, with need for HAE.
Splenic trauma literature has described a correlation between CT contrast blush greater than 1 cm in diameter and need for intervention [15]. However, the current study found no association between size of contrast blush on CT and need for HAE. This may represent an intrinsic difference between hepatic and splenic trauma. Additionally, measurement of contrast blush on CT is dependent upon technical factors, such as image slice thickness and window/level, as well as interrater variance. The interrater variability of diameter measurements on CT has been previously described [16, 17].
This study has several limitations. Analyses were performed based on retrospective data extracted from the electronic medical record, but clinical data were completely missing for 12 patients who would have otherwise been included in the study. The missing data were likely lost during the institutional transition from a paper-based to electronic medical record system which occurred during the study period. Given the relatively limited sample size, when determining clinical variables of potential significance a priori for multivariate analyses, we included only AAST hepatic injury grade, pre-procedural shock, and pre-procedural blood transfusions. We were unable to justify a full model using all imaging characteristics of hepatic injury as covariates, and opted instead to include AAST hepatic injury grade as a proxy for these imaging findings. Another limitation of this study is the lack of grade 5 hepatic injuries; study results should not be extrapolated to the most severe hepatic injuries. Unstable patients with the most severe injuries went straight to the operating room instead of receiving angiography, and thus were not included in the cohort.
The data on inter-reader agreement were felt highly limited as this study included two interpreting radiologists with widely different levels of experience. As such, it was felt that consensus discussion to resolve differences in ratings of CT imaging findings was most appropriate for purposes of statistical analysis. Binary imaging findings initially hypothesized to be associated with positive angiography, such as active extravasation, pseudoaneurysm, and large hemoperitoneum, had substantial or almost perfect agreement per Kappa. Interpretation by an additional attending was felt unlikely to change the study results. The inter-reader agreement data are included within supplemental materials for interested readers.
Conclusion
CTA is an important test in the setting of hepatic trauma to help determine which patients should undergo angiography with possible HAE. While AAST hepatic injury grade was associated with need for HAE, most imaging findings and clinical parameters, including hemodynamic instability, were not significantly associated with need for intervention. Prediction of need for HAE is difficult, requiring consideration of both clinical factors and imaging findings. Since angiography can be both diagnostic and therapeutic, and is associated with lower risk and morbidity than laparotomy, it is acceptable in current practice for select individuals to undergo angiography without embolization.
References
Tinkoff, G., T. J. Esposito, J. Reed, P. Kilgo, J. Fildes, M. Pasquale, and J. W. Meredith. "American Association for the Surgery of Trauma Organ Injury Scale I: Spleen, Liver, and Kidney, Validation Based on the National Trauma Data Bank." J Am Coll Surg 207, no. 5 (2008): 646-55.
Samuels, J. M., S. Urban, E. Peltz, T. Schroeppel, H. Heise, W. C. Dorlac, L. J. Britton, C. C. Burlew, C. Robinson, M. L. Swope, and R. C. McIntyre, Jr. "A Modern, Multicenter Evaluation of Hepatic Angioembolization - Complications and Readmissions Persist." Am J Surg 219, no. 1 (2020): 117-22.
Stassen, N. A., I. Bhullar, J. D. Cheng, M. Crandall, R. Friese, O. Guillamondegui, R. Jawa, A. Maung, T. J. Rohs, Jr., A. Sangosanya, K. Schuster, M. Seamon, K. M. Tchorz, B. L. Zarzuar, A. Kerwin, and Trauma Eastern Association for the Surgery of. "Nonoperative Management of Blunt Hepatic Injury: An Eastern Association for the Surgery of Trauma Practice Management Guideline." J Trauma Acute Care Surg 73, no. 5 Suppl 4 (2012): S288-93.
Polanco, P. M., J. B. Brown, J. C. Puyana, T. R. Billiar, A. B. Peitzman, and J. L. Sperry. "The Swinging Pendulum: A National Perspective of Nonoperative Management in Severe Blunt Liver Injury." J Trauma Acute Care Surg 75, no. 4 (2013): 590-5.
Navsaria, P. H., A. J. Nicol, J. E. Krige, and S. Edu. "Selective Nonoperative Management of Liver Gunshot Injuries." Ann Surg 249, no. 4 (2009): 653-6.
Kozar, R. A., F. A. Moore, E. E. Moore, M. West, C. S. Cocanour, J. Davis, W. L. Biffl, and R. C. McIntyre, Jr. "Western Trauma Association Critical Decisions in Trauma: Nonoperative Management of Adult Blunt Hepatic Trauma." J Trauma 67, no. 6 (2009): 1144-8; discussion 48-9.
Coccolini, F., F. Catena, E. E. Moore, R. Ivatury, W. Biffl, A. Peitzman, R. Coimbra, S. Rizoli, Y. Kluger, F. M. Abu-Zidan, M. Ceresoli, G. Montori, M. Sartelli, D. Weber, G. Fraga, N. Naidoo, F. A. Moore, N. Zanini, and L. Ansaloni. "Wses Classification and Guidelines for Liver Trauma." World J Emerg Surg 11 (2016): 50.
Letoublon, C., I. Morra, Y. Chen, V. Monnin, D. Voirin, and C. Arvieux. "Hepatic Arterial Embolization in the Management of Blunt Hepatic Trauma: Indications and Complications." J Trauma 70, no. 5 (2011): 1032-6; discussion 36-7.
Poletti, P. A., S. E. Mirvis, K. Shanmuganathan, K. L. Killeen, and D. Coldwell. "Ct Criteria for Management of Blunt Liver Trauma: Correlation with Angiographic and Surgical Findings." Radiology 216, no. 2 (2000): 418-27.
Misselbeck, T. S., E. J. Teicher, M. D. Cipolle, M. D. Pasquale, K. T. Shah, D. A. Dangleben, and M. M. Badellino. "Hepatic Angioembolization in Trauma Patients: Indications and Complications." J Trauma 67, no. 4 (2009): 769-73.
Cohn, S. M., J. I. Arango, J. G. Myers, P. P. Lopez, R. B. Jonas, L. L. Waite, M. G. Corneille, R. M. Stewart, and D. L. Dent. "Computed Tomography Grading Systems Poorly Predict the Need for Intervention after Spleen and Liver Injuries." Am Surg 75, no. 2 (2009): 133-9.
Moore, E. E., S. R. Shackford, H. L. Pachter, J. W. McAninch, B. D. Browner, H. R. Champion, L. M. Flint, T. A. Gennarelli, M. A. Malangoni, M. L. Ramenofsky, and et al. "Organ Injury Scaling: Spleen, Liver, and Kidney." J Trauma 29, no. 12 (1989): 1664-6.
MacLean, A. A., A. Durso, S. M. Cohn, J. Cameron, and F. Munera. "A Clinically Relevant Liver Injury Grading System by Ct, Preliminary Report." Emerg Radiol 12, no. 1-2 (2005): 34-7.
Fang, J. F., Y. C. Wong, B. C. Lin, Y. P. Hsu, and M. F. Chen. "The Ct Risk Factors for the Need of Operative Treatment in Initially Hemodynamically Stable Patients after Blunt Hepatic Trauma." J Trauma 61, no. 3 (2006): 547-53; discussion 53-4.
Thompson, B. E., F. Munera, S. M. Cohn, A. A. MacLean, J. Cameron, L. Rivas, and D. Bajayo. "Novel Computed Tomography Scan Scoring System Predicts the Need for Intervention after Splenic Injury." J Trauma 60, no. 5 (2006): 1083-6.
McNitt-Gray, M. F., G. H. Kim, B. Zhao, L. H. Schwartz, D. Clunie, K. Cohen, N. Petrick, C. Fenimore, Z. Q. Lu, and A. J. Buckler. "Determining the Variability of Lesion Size Measurements from Ct Patient Data Sets Acquired under "No Change" Conditions." Transl Oncol 8, no. 1 (2015): 55-64.
Cayne, N. S., F. J. Veith, E. C. Lipsitz, T. Ohki, M. Mehta, N. Gargiulo, W. D. Suggs, A. Rozenblit, Z. Ricci, and C. H. Timaran. "Variability of Maximal Aortic Aneurysm Diameter Measurements on Ct Scan: Significance and Methods to Minimize." J Vasc Surg 39, no. 4 (2004): 811-5.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, K., Mabud, T.S., Patel, N. et al. Predictors of need for endovascular intervention in hepatic trauma. Abdom Radiol 48, 1131–1139 (2023). https://doi.org/10.1007/s00261-022-03765-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03765-1