Abstract
Purpose
To perform a descriptive analysis of individuals with suspected Polyarteritis nodosa (PAN) referred for second opinion imaging consultation.
Methods
A retrospective observational cohort study was performed at a single institution. A consecutive sample was performed of individuals who underwent a second opinion CT or MR angiography subspecialty radiologist consultation between January 2008 and September 2019 for suspected abdominal medium vessel vasculitis. Demographic, clinical, and imaging data were collected. Clinical and imaging findings were reported for PAN, small vessel vasculitis, and “non-vasculitis” groups. Agreement and diagnostic accuracy between final clinical and second opinion imaging diagnoses for PAN were determined. Two-tailed t-tests with a significant p-value < 0.05 were utilized.
Results
Of the 58 participants, 9 were clinically diagnosed with PAN, 11 with small vessel vasculitis (including lupus, IgA, and ANCA-associated vasculitis), and 38 with non-vasculitis diagnoses. The non-vasculitis group included 15 SAM, 3 FMD, and 1 SAM-FMD spectrum diagnoses. Higher C-reactive protein level (51 vs 17, p = 0.04) and superior mesenteric artery involvement (56% vs 21%, p = 0.04) were more common in PAN than non-vasculitis diagnoses, while arterial dissection (40% vs 0%, p = 0.02) and celiac vasculature involvement (53% vs 0%, p = 0.003) were more common in the non-vasculitis group. There was 88% agreement (51/58; Cohen’s kappa 0.56); sensitivity was 67% [95%-confidence interval (CI) 30–93%] and specificity was 92% (95%-CI 80–98%).
Conclusion
Isolated celiac artery involvement and arterial dissection were more common in non-inflammatory vasculopathies than PAN. Our findings highlight the need for multidisciplinary collaboration and awareness of the diverse findings of abdominal vasculopathies.
Graphic abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vasculitis is a pathology that causes vessel wall inflammation and necrosis and is used to describe a large group of conditions with this shared pathology [1]. They are grossly classified based on whether they involve large, medium, small or variable vessels [1]. Polyarteritis nodosa (PAN) is an uncommon medium vessel vasculitis which most frequently affects men in their fourth through sixth decades of life with an annual incidence of 2 to 9 per 1 million adults [2, 3]. Idiopathic cases of PAN are most common, however, associations with hepatitis B virus, hepatitis C virus, human immunodeficiency virus, parvovirus B19, and hairy cell leukemia have been reported [2,3,4]. It can affect multiple organs but commonly the kidneys and gastrointestinal system, and may present with constitutional symptoms, arthralgia, renal failure, hypertension, abdominal pain, or gastrointestinal bleeding [2, 4]. Typical imaging features of PAN include multiple aneurysms (1–5 mm in size) affecting the renal, hepatic, and mesenteric arteries, as
well as coexisting stenotic lesions [2, 3]. The varied clinical presentation of PAN, lack of accurate biomarkers, and frequent difficulty in obtaining a pathology specimen makes the careful integration of clinical and imaging findings a necessity to make an accurate diagnosis [5, 6]. Furthermore, many different vasculopathies can occur in the abdomen, and differentiating between them can be difficult as they can often present similarly. As a result, imaging findings are often relied upon to distinguish amongst them [1, 7].
In diagnostic imaging studies, several non-inflammatory vascular conditions have been found to masquerade as PAN, including segmental arterial mediolysis (SAM) and fibromuscular dysplasia (FMD). SAM is a non-inflammatory vasculopathy which affects medium-sized abdominal arteries, while FMD is an idiopathic, non-inflammatory vasculopathy which can involve small and medium-sized arteries, most commonly renal and carotid. Both FMD and SAM may demonstrate clinical and radiologic overlap with PAN, raising diagnostic uncertainty and requiring specialist review [8,9,10,11].
Given the subtlety and similarity of clinical and imaging findings, comparing these diagnoses to understand what can differentiate them warrants further exploration [1, 2, 5, 7]. We performed a descriptive and comparative analysis of individuals with suspected abdominal medium vessel vasculitis, specifically PAN, referred for second opinion imaging consultation by an experienced subspecialty radiologist. Through this, we assessed the different patterns of presentation for these diseases and how subspecialist review may assist in finding the final diagnosis.
Methods
Local institutional research ethics board approval was obtained for this study and the requirement for informed consent was waived prior to commencement (project number 8103). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for observational studies were followed [12].
Study design and participants
A retrospective observational cohort study was performed at a single institution (St. Joseph’s Healthcare Hamilton, Canada) that is a regional assessment centre for the diagnosis and management of vasculopathies. A consecutive sample of eligible participants who had received consults on outside imaging on our local Picture And Archiving System (PACS) was gathered between January 1, 2008 and September 30, 2019. All second opinions were formal imaging reviews requested from rheumatologists to assess CT angiography or MR angiography studies performed at outside institutions. For each case, the clinical question asked on the consult request form was to rule in/rule out vasculitis affecting the splanchnic vasculature. Individuals without a clinical history, serologic and imaging evaluation at presentation (prior to any treatment), and final clinical diagnosis (made by the rheumatology/ vasculitis team) were excluded.
Data collection
Demographic, clinical, and imaging data for each patient was extracted from a chart review of rheumatology notes. Demographic data consisted of date of birth and sex. Clinical data included the following: initial clinical diagnosis, reason for referral, final clinical diagnosis, presence of clinical signs and symptoms (abdominal pain, neuropathy, weight loss > 5 kg or 10% of body weight, fever/chills/night sweats, arthralgias, myalgias, rash, palpable purpura, transient ischemic attack, testicular pain, hypertension), bloodwork results (leukocytes, platelets, C-reactive protein [CRP], erythrocyte sedimentation rate [ESR], rheumatoid factor [RF], anti-cyclic citrullinated peptide [anti-CCP] antibody, anti-nuclear antibody [ANA], antineutrophil cytoplasmic antibodies [ANCA], cryoglobulins, hepatitis B serology, hepatitis C serology, and urinalysis), history of treatment with steroids, and genetic testing, if available. If multiple results were available for serologic/hematologic parameters, the peak value was recorded.
The second opinion interpretations of all imaging studies for eligible participants were performed by a radiologist with 15 years of experience interpreting vasculitis-relating imaging examinations (RR). The radiologist was blinded to the final clinical diagnosis, but not to other clinical information at time of second opinion assessment. The reports were then reviewed by a single co-author (MA). If a study participant underwent multiple abdominal CT and/or MRI examinations for which a second opinion consultation was obtained, the data for each examination was extracted and compiled. For each report, the most likely diagnosis based on imaging was extracted. The number of abdominal vascular territories involved was also assessed. The abdominal arterial vasculature was grouped as the following for the purposes of assessing the number of vascular beds affected: aorta; celiac artery and any associated branches; superior mesenteric artery (SMA) and any associated branches; renal arteries; inferior mesenteric artery and any associated branches; common iliac arteries and any associated branches. Furthermore, each examination was coded according to the presence or absence of the following findings related to the abdominal arterial vasculature: aneurysm or pseudoaneurysm; dissection (and/or intramural hematoma); wall thickening (including soft tissue rind); luminal irregularity; beading, corrugation, or corkscrew appearance; luminal webs; stenosis; occlusion; and/or visceral infarction. A vessel was labelled aneurysmal/pseudoaneurysmal if there was fusiform enlargement (more than 1.5 times the calibre of the vessel proximal or distal to the affected segment) or any focal saccular outpouching from the normal path of the vessel. Wall thickening and/or soft tissue rind was the descriptor used when a circumferential cuff of soft tissue attenuation was noted around any vessel whether felt to be mural-based or peri-adventitial. Luminal irregularity was deemed present when the normal smooth inner contour of the vessel was disrupted but subjectively was different than a beaded, corrugated or corkscrew appearance. The degree of stenosis, whether mild, moderate, or severe, was not subcategorized, but was differentiated from vascular occlusion. The co-author performing data collection retrieved the imaging data and was blinded to all clinical information, including the final clinical diagnosis at that time. Imaging and clinical data collection were performed with a 6-week washout gap to minimize recall bias.
Outcomes and statistical analysis
Study participants were categorized into three groups based on the final clinical diagnosis: PAN (medium vessel vasculitis), small vessel vasculitis, or “non-vasculitis”. The “non-vasculitis” group incorporated multiple diagnoses, including SAM, FMD, atherosclerotic disease, and no underlying abdominal vasculitis/vasculopathy. Mean age and standard deviation (SD) was reported for each group. For binary clinical and imaging variables, frequency was reported for each group. For continuous clinical and imaging variables, median and interquartile range (IQR) was reported for each group. Two-tailed t-tests were utilized to compare the PAN and non-vasculitis groups; a p-value < 0.05 was considered statistically significant. The small vessel vasculitis group was not included in the statistical comparison as differentiation between PAN and small vessel vasculitis is often made clinically, and medium vessel changes are not expected in individuals with small vessel vasculitis on imaging. Frequency of agreement between the second opinion and final diagnosis was found and agreement was assessed using Cohen’s Kappa. Furthermore, the diagnostic accuracy of the second opinion imaging consultation for determining the presence of PAN was determined. Sensitivity and specificity were calculated with 95% confidence intervals (95%-CI) based on the exact Clopper-Pearson method. A true positive result was defined as an imaging and final clinical diagnosis of PAN. A false negative result was defined as a final clinical diagnosis of PAN with no imaging diagnosis of PAN. A true negative result was defined as no imaging or final clinical diagnosis of PAN. A false positive result was defined as an imaging diagnosis of PAN with no clinical diagnosis of PAN.
Results
Outcomes and statistical analysis
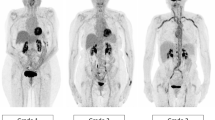
A total of 58 participants were referred for a second opinion review of 62 abdominal CTs and 9 abdominal MRIs performed for suspected abdominal medium vessel vasculitis, specifically PAN, and included in the study. Based on final clinical diagnosis, 9 individuals were diagnosed with PAN (Fig. 1), 11 with small vessel vasculitis, and 38 with non-inflammatory vasculopathies (non-vasculitis). In the non-vasculitis group, 19 were diagnosed with SAM-FMD spectrum disorders, 5 with genetic vasculopathies, and 14 diagnoses of other diseases (Table 1). Fifteen were diagnosed with SAM (Fig. 2), 3 were diagnosed with FMD (Fig. 3), and 1 individual was diagnosed with SAM-FMD spectrum disorder. Five individuals with genetic vasculopathies were identified, including 2 individuals involving the COL3A1 gene (Fig. 4), 1 individual involving the TGFBR2 gene, 1 individual involving the PRDM5 gene, and 1 individual involving the ZNF469 gene. Other diagnoses included median arcuate ligament syndrome, spontaneous/traumatic arterial dissection, IgG4-related disease (Fig. 5), post-surgical vasospasm, varicella zoster vasculopathy, polymyalgia rheumatica, atherosclerosis, and no underlying abdominal vasculitis/vasculopathy. Small vessel vasculitis etiologies included ANCA-associated vasculitis (n = 2), systemic lupus erythematosus (SLE) (n = 1), and IgA vasculitis (n = 3).
Coronal arterial-phase CT image of the abdomen in an individual with polyarteritis nodosa (PAN) demonstrates a thick concentric soft tissue rind surrounding the superior mesenteric artery (SMA) and multiple jejunal and ileal branches, with resulting luminal narrowing (solid arrows), as well as occlusion of several jejunal branches (chevrons). A proximal SMA pseudoaneurysm is also noted (open arrows)
Coronal (A) and axial (B) arterial-phase CT images of the abdomen demonstrate isolated celiac artery disease with a non-enhancing eccentric area of thickening representing an intramural hematoma (solid arrow), as well as a dissecting aneurysm (open arrow) in an individual with segmental arterial mediolysis (SAM)
Multiple axial CT angiography images A–C of the abdomen and pelvis in an individual with a COL3A1 gene mutation diagnosed with vascular Ehlers-Danlos Syndrome (vEDS) demonstrate a beaded and corkscrew appearance of the left gastric artery (solid arrow), aneurysmal dilatation of the common and right hepatic arteries with non-enhancing thrombus and luminal irregularity (open arrows), as well as dissection of the right common iliac artery (chevron)
Axial CT angiography image (A) and axial delayed phase contrast-enhanced MR image (B) of the abdomen demonstrate findings of a slightly eccentric rind of soft surrounding the aorta (arrows) in an individual with IgG4-related disease. Note the enhancement of the rind of soft tissue, best appreciated on the MRI (B)
Clinical and imaging data
Table 1 provides a summary of the clinical characteristics for the PAN, small vessel vasculitis, and non-vasculitis groups. When comparing the PAN and non-vasculitis groups, those with PAN were more likely to have history of a skin rash (33% vs 5%, p = 0.02) or palpable purpura (22% vs 0%, p < 0.01). Median CRP was also higher in the PAN group (51, IQR 27–64, p = 0.04) compared to the non-vasculitis group (17, IQR 10–41). All individuals, however, had a similar prevalence of hypertension, abdominal pain, constitutional symptoms, and other features that are often attributed to PAN.
Table 2 provides a summary of the affected vasculature, while Table 3 provides a summary of the imaging characteristics for the PAN, small vessel vasculitis, and non-vasculitis groups. Involvement of the celiac trunk vasculature was more frequently seen in the non-vasculitis group than the PAN group (53% vs 0%, p = 0.003). On the contrary, SMA involvement was more common in the PAN group than the non-vasculitis group (56% vs 21%, p = 0.04). Both groups commonly involved the renal arteries (40–44%, p = 0.79), while the aorta and iliac vessels were uncommonly involved (0–16%, p = 0.32–0.78). Furthermore, there were no arterial dissections in the PAN group compared to 39% in the non-vasculitis group (p = 0.02). Both PAN cohort and the non-vasculitis cohort had aneurysms (56–61%, p = 0.79); they commonly had luminal irregularities (33–42%, p = 0.64), stenosis (37–44%, p = 0.68), beading (29–33%, p = 0.80), and wall thickening (21–33%, p = 0.64). Vessel occlusions (8–11%, p = 0.76), visceral infarcts (11–21%, p = 0.51), and luminal webs (0–13%, p = 0.26) were uncommon in the PAN and non-vasculitis groups. In the small vessel vasculitis group, 5 individuals did not have any imaging abnormalities of the abdominal vasculature (45%), of which 2 individuals demonstrated visceral abnormalities. In total, 4 individuals (36%) within the small vessel vasculitis group demonstrated visceral abnormalities on imaging, only one of which was confirmed to be ischemia.
Findings from second opinions
Overall, there was 88% agreement (51/58 participants) between the second opinion imaging diagnosis and final clinical diagnosis, with a Cohen’s kappa of 0.56. In terms of diagnostic accuracy, this corresponded to a sensitivity of 67% (95%-CI 30–93%) and a specificity of 92% (95%-CI 80–98%) for diagnosing abdominal PAN in individuals with a suspected medium vessel vasculitis referred for a second opinion CT or MRI consultation. Of the 7 participants with discordance between imaging diagnosis and final clinical diagnosis, 3 were false negatives, with a final clinical diagnosis of PAN with no corresponding PAN diagnosis on imaging. Included in this subset of patients with no vascular abnormalities on imaging, vasculitis was seen histopathologically in one individual on prostate biopsy, and in another individual following colonic resection. The remaining 4 individuals had a false positive result, with an imaging diagnosis of PAN, but no corresponding final clinical diagnosis of PAN. The final clinical diagnoses for these cases were SAM, IgG4-related disease, FMD, and vasospasm related to recent surgery.
Discussion
In this retrospective cohort of individuals who were referred on for a second opinion of vasculitis, we found that individuals who often present with similar clinical and imaging features can have a variety of different underlying diagnoses. A clinical history of skin rash, palpable purpura, and higher CRP were more commonly seen in the PAN group versus the non-vasculitis group, emphasizing the need for collaboration between clinicians and radiologists to guide interpretation.
Only 16% of the total cohort were found to have a final diagnosis of PAN, where the initial clinical suspicion was for an abdominal medium vessel vasculitis. These findings highlight that the angiographic features of PAN demonstrate a considerable overlap with non-vasculitis mimickers, particularly SAM and FMD, which made up 32% of the cohort [8,9,10,11, 13,14,15,16,17]. This also highlights a limitation of the American College of Radiology criteria, where similar clinical syndromes were seen across all individuals, and either histopathology or expertise in clinical findings were needed to differentiate the final diagnosis. While the spectrum of imaging findings for each disease has been previously defined [6, 9, 11], our study suggests the possibility of using differentiating features on angiographic studies, including the vascular bed involvement (SMA vs celiac in PAN) and the presence of arterial dissections in the non-vasculitis mimickers.
Previous studies have reported similar abdominal imaging findings for PAN, with aneurysms seen in approximately half of patients, followed by vessel narrowing and occlusion, most frequently affecting the SMA [1, 2, 6, 18]. However, the literature reports that SAM most commonly affects the SMA with aneurysm formation and/or dissection, whereas we found SMA involvement was more frequently seen in PAN, while celiac vessel involvement suggested a non-vasculitis etiology, such as SAM [15, 16, 19]. FMD most frequently affects renal arteries with dissection and/or aneurysm formation, whereas “mesenteric FMD” affecting the celiac artery and SMA is rare [19, 20]. Given this, the findings of our study suggest that involvement of the mesenteric vasculature and/or the presence of dissection may help in differentiating PAN and FMD, given the overlap in renal artery involvement and aneurysm formation.
In addition to previously described vasculopathies, we identified a subset of patients with underlying inherited connective tissue disorders presenting with vascular abnormalities on abdominal imaging. We identified 5 patients with genetic mutations, including 2 patients with a genotype suggesting vascular Ehlers-Danlos Syndrome (EDS) with mutation in COL3A1 gene [21]. One individual mutation involving the PRDM5 gene, while a second individual had a mutation involving the ZNF469 gene; both are described in brittle cornea syndrome, which falls in the EDS spectrum [22]. Another mutation identified involved the TGFBR2 gene, which has been described in patients with a Marfan or Loeys-Dietz phenotype [23]. Unfortunately, the majority of patients were not tested for underlying genetic disorders as this only became more widely available towards the end of the study period. Radiologists interpreting abdominal imaging studies should be aware of inherited vasculopathies as a potential cause for splanchnic vascular abnormalities. Vascular dissections, often multiple, were a frequent feature in this patient subset (mean 5.6 ± 4.0 vessels vs 3.7 ± 2.4 vessels in SAM-FMD; p = 0.20). Some of these patients had dissections involving both large (aorta and iliac arteries) and medium vessels, a feature that is atypical in large vessel and medium vessel vasculitis.
Our study had several limitations. First, our sample size for participants with PAN was limited as this study was meant to be a descriptive analysis, and further studies with larger samples are warranted. PAN is rare disease and accumulating a large series of patients for evaluation is difficult even in a tertiary rheumatology referral site. The study is also subject to a complexity bias as more ‘easily’ diagnosed medium vessel vasculopathies may not have been referred on for assessment. Furthermore, we compared both angiographic CT and MRI, and there were slight protocol variations across different studies, as they were imported from different hospital sites with different institutional protocols. Some, but not all patients had some form of follow-up imaging available limiting assessment of temporal evolution in many patients. The imaging criteria utilized were not assessed for inter-reader variability, as interpretation was performed by a single radiologist. The reporting of serologic and genetic testing, as well as access to the initial opinion on imaging, were limited in our study, and these may be assessed further in future studies.
The results of this analysis suggests that celiac axis involvement and vessel dissection are uncommon findings in the diagnosis of PAN and should raise clinical suspicion for non-inflammatory vasculopathies and other diagnoses. We also demonstrated the value of a second opinion imaging consultation, with a high level of agreement between the radiologist second opinion and final clinical diagnosis. Our findings support that in approaching these complex diagnoses, the utility of multidisciplinary collaboration in differentiating these rare but overlapping diagnoses is vital. Indeed, further investigation into more widespread use of second opinion subspecialty radiologist consultations in standardized diagnostic pathways for suspected abdominal vasculitis is warranted.
Data availability
Study data are available upon request.
Abbreviations
- PAN:
-
Polyarteritis nodosa
- SAM:
-
Segmental arterial mediolysis
- FMD:
-
Fibromuscular dysplasia
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- PACS:
-
Picture and Archiving System
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- RF:
-
Rheumatoid factor
- Anti-CCP antibody:
-
Anti-cyclic citrullinated peptide
- ANA:
-
Anti-nuclear antibody
- ANCA:
-
Antineutrophil cytoplasmic antibodies
- SMA:
-
Superior mesenteric artery
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- 95%-CI:
-
95% Confidence intervals
- SLE:
-
Systemic lupus erythematosus
References
Weinrich JM, Lenz A, Adam G, et al (2020) Radiologic Imaging in Large and Medium Vessel Vasculitis. Radiol Clin North Am 58:765–779. https://doi.org/10.1016/j.rcl.2020.02.001
De Virgilio A, Greco A, Magliulo G, et al (2016) Polyarteritis nodosa: A contemporary overview. Autoimmun Rev 15:564–570. https://doi.org/10.1016/j.autrev.2016.02.015
Forbess L, Bannykh S (2015) Polyarteritis nodosa. Rheum Dis Clin North Am 41:33–46. https://doi.org/10.1016/j.rdc.2014.09.005
Alibaz-Oner F, Koster MJ, Crowson CS, et al (2017) Clinical Spectrum of Medium-Sized Vessel Vasculitis. Arthritis Care Res (Hoboken) 69:884–891. https://doi.org/10.1002/acr.23007
Singhal M, Gupta P, Sharma A (2019) Imaging in small and medium vessel vasculitis. Int J Rheum Dis 22:78–85. https://doi.org/10.1111/1756-185X.13390
Stanson AW, Friese JL, Johnson CM, et al (2001) Polyarteritis Nodosa: Spectrum of Angiographic Findings. RadioGraphics 21:151–159. https://doi.org/10.1148/radiographics.21.1.g01ja16151
Ha HK, Lee SH, Rha SE, et al (2000) Radiologic features of vasculitis involving the gastrointestinal tract. Radiographics 20:779–794. https://doi.org/10.1148/radiographics.20.3.g00mc02779
Skeik N, Hyde JR, Olson SL, et al (2019) Nonatherosclerotic Abdominal Vasculopathies. Ann Vasc Surg 60:128–146. https://doi.org/10.1016/j.avsg.2019.04.004
Pontes T de C, Rufino GP, Gurgel MG, et al (2012) Fibromuscular dysplasia: A differential diagnosis of vasculitis. Rev Bras Reumatol 52:66–74
Chatterjee T, Stephens J, Roy M (2020) Segmental Arterial Mediolysis: An Under-Recognized Cause of Chronic Abdominal Pain. Eur J Case Reports Intern Med 7:001830. https://doi.org/10.12890/2020_001830
Alhalabi K, Menias C, Hines R, et al (2017) Imaging and clinical findings in segmental arterial mediolysis (SAM). Abdom Radiol 42:602–611. https://doi.org/10.1007/s00261-016-0887-4
Ghaferi AA, Schwartz TA, Pawlik TM (2021) STROBE Reporting Guidelines for Observational Studies. JAMA Surg. https://doi.org/10.1001/jamasurg.2021.0528
Chan RJ, Goodman TA, Aretz TH, Lie JT (1998) Segmental mediolytic arteriopathy of the splenic and hepatic arteries mimicking systemic necrotizing vasculitis. Arthritis Rheum 41:935–938. https://doi.org/10.1002/1529-0131(199805)41:5<935::AID-ART22>3.0.CO;2-N
Siegert CEH, Macfarlane JD, Hollander AMJ, Van Kemenade F (1996) Systemic fibromuscular dysplasia masquerading as polyarteritis nodosa. Nephrol Dial Transplant 11:1356–1358. https://doi.org/10.1093/ndt/11.7.1356
Skeik N, Olson SL, Hari G, Pavia ML (2019) Segmental arterial mediolysis (SAM): Systematic review and analysis of 143 cases. Vasc Med (United Kingdom) 24:549–563. https://doi.org/10.1177/1358863X19873410
Shenouda M, Riga C, Naji Y, Renton S (2014) Segmental arterial mediolysis: A systematic review of 85 cases. Ann Vasc Surg 28:269–277. https://doi.org/10.1016/j.avsg.2013.03.003
Kim HS, Min S Il, Han A, et al (2016) Longitudinal evaluation of segmental arterial mediolysis in splanchnic arteries: Case series and systematic review. PLoS One 11:. https://doi.org/10.1371/journal.pone.0161182
Schmidt WA (2004) Use of imaging studies in the diagnosis of vasculitis. Curr Rheumatol Rep 6:203–211. https://doi.org/10.1007/s11926-004-0069-1
Ko M, Kamimura K, Ogawa K, et al (2018) Diagnosis and management of fibromuscular dysplasia and segmental arterial mediolysis in gastroenterology field: A mini-review. World J Gastroenterol 24:3637–3649. https://doi.org/10.3748/wjg.v24.i32.3637
Olin JW, Froehlich J, Gu X, et al (2012) The United States registry for fibromuscular dysplasia: Results in the first 447 patients. Circulation 125:3182–3190. https://doi.org/10.1161/CIRCULATIONAHA.112.091223
Boussouar S, Benattia A, Escudié JB, et al (2021) Vascular Ehlers–Danlos syndrome (vEDS): CT and histologic findings of pleural and lung parenchymal damage. Eur Radiol. https://doi.org/10.1007/s00330-021-07710-6
Dhooge T, Van Damme T, Syx D, et al (2021) More than meets the eye: Expanding and reviewing the clinical and mutational spectrum of brittle cornea syndrome. Hum Mutat 42:711–730. https://doi.org/10.1002/humu.24199
Singh KK, Rommel K, Mishra A, et al (2006) TGFBR1 and TGFBR2 mutations in patients with features of Marfan syndrome and Loeys-Dietz syndrome. Hum Mutat 27:770–777. https://doi.org/10.1002/humu.20354
Funding
No funding was provided for any component of the submitted work.
Author information
Authors and Affiliations
Contributions
All coauthors were involved in inception, data collection, preparation, and editing of this manuscript. The final manuscript has been reviewed and approved for submission by all coauthors involved.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest or competing interests to disclose. The authors declare they have no financial interests or non-financial interests.
Ethical approval
Local institutional research ethics board approval was obtained for this study and the requirement for informed consent was waived prior to commencement (project number 8103).
Informed consent
Appropriate consent was obtained where applicable.
Consent for publication
Appropriate consent was obtained where applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alabousi, M., Junek, M., Garner, S. et al. Value of second opinion subspecialty radiology consultation in suspected abdominal medium vessel vasculitis. Abdom Radiol 46, 5763–5771 (2021). https://doi.org/10.1007/s00261-021-03277-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03277-4