Abstract
Purpose
To evaluate the correlation between liver stiffness as measured on MR elastography and T1 and T2 relaxation times from T1 and T2 mapping with clinical parameters of liver disease, including the MELD score, MELD-Na and ALBI grade, and endoscopically visible esophageal varices.
Materials and methods
223 patients with known or suspected liver disease underwent MRI of the liver with T1 mapping (Look-Locker sequence) and 2D SE-EPI MR elastography (MRE) sequences. 139 of these patients also underwent T2 mapping with radial T2 FS sequence. Two readers measured liver stiffness, T1 relaxation times and T2 relaxation times, and assessed qualitative features such as presence or absence of cirrhosis, ascites, spleen length, and varices on conventional MRI images. A third reader collected the clinical data (MELD score, MELD-Na Score, ALBI grade, and results of endoscopy in 78 patients).
Results
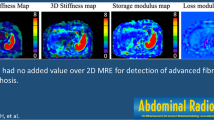
Significant moderate correlation was found between MELD score and all three imaging techniques for both readers (MRE, r = 0.35 and 0.28; T1 relaxometry, r = 0.30 and 0.29; T2 relaxometry, r = 0.45, and 0.37 for reader 1 and reader 2 respectively). Correlation with MELD-Na score was even higher (MRE, r = 0.49 and 0.40; T1, r = 0.45 and 0.41; T2, r = 0.47 and 0.35 for reader 1 and reader 2 respectively). Correlations between MRE and ALBI grade was significant and moderate for both readers: r = 0.39 and 0.37, higher than T1 relaxometry (r = 0.22 and 0.20) and T2 relaxometry (r = 0.17, and r = 0.24). Significant moderate correlations were found for both readers between MRE and the presence of varices on endoscopy (r = 0.28 and 0.30). MRE and T1 relaxometry were significant predictors of varices at endoscopy for both readers (MRE AUC 0.923 and 0.873; T1 relaxometry AUC = 0.711 and 0.675 for reader 1 and reader 2 respectively). Cirrhotic morphology (AUC = 0.654), spleen length (AUC = 0.610) and presence of varices in the upper abdomen on MRI (AUC of 0.693 and 0.595) were all significant predictors of endoscopic varices. Multivariable logistic regression model identified that spleen length and liver MRE were significant independent predictors of endoscopic varices for both readers.
Conclusion
MR elastography, T1 and T2 relaxometry demonstrated moderate positive correlation with the MELD score and MELD-Na Score. Correlation between MRE and ALBI grade was superior to T1 and T2 relaxometry methods. MRE performed better than T1 and T2 relaxometry to predict the presence of varices at endoscopy. On multivariate analyses, spleen length and MRE were the only two significant independent predictors of endoscopic varices.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver disease is increasing in prevalence. As the nonspecific response to liver injury, hepatic fibrosis progresses through stages, culminating in the common end pathway for continued liver insult—cirrhosis [1, 2]. Although liver biopsy has been long considered the gold standard for diagnosing and monitoring liver fibrosis, it is costly, subject to sampling error and has a non-negligible complication rate [3, 4]. Several laboratory-based prognostic models are utilized in patients with liver disease. The MELD score (Model for End-Stage Liver Disease) uses total serum creatinine, total serum bilirubin and the international normalized ratio (INR) to predict short-term survival in cirrhotic patients and is used to prioritize liver transplantation [5, 6]. More recently, the ALBI grade was developed as a simplified measure of liver function, using only albumin and total serum bilirubin, with prognostic implications in patients with hepatocellular carcinoma [7, 8]. Esophageal varices are a potentially life-threatening complication of portal hypertension, requiring monitoring, and often treatment in cirrhotic patients [9]. Endoscopy is routinely performed in cirrhotic patients to exclude GE junction varices, despite low prevalence of varices at high risk of bleeding/needing treatment. Baveno VI guidelines recommends avoiding endoscopy in patients with transient elastography liver stiffness measurement < 20 kPa and a platelet count > 150,000 cells/µl, given the very low incidence of large varices requiring treatment in this population [10, 11]. However, studies have shown that endoscopy may not be necessary in a substantial number of patients who meet the criteria (up to 40%), indicating the need for a more robust criteria to select those in need of endoscopy [12].
Several non-invasive MRI imaging techniques have gained increasing recognition and utilization in recent years for the staging and monitoring of liver disease. MR elastography, which measures shear wave propagation through tissue, has demonstrated high accuracy and reproducibility in staging liver fibrosis [13,14,15]. Stiffness measurements from MR elastography has been found to correlate with the hepatic venous pressure gradient, the gold standard but invasive method of detecting and monitoring portal hypertension in cirrhosis [16]. MR relaxometry techniques measure the T1 and T2 relaxation times of the liver and have also shown promise in the non-invasive staging of liver fibrosis [17,18,19,20,21]. MRE and T1 mapping have both been used to predict the presence of portal hypertension and esophageal varices [16,17,18, 22,23,24,25,26]. Recently published studies have shown that the T1 relaxation time significantly increases with higher Child-Pugh classification [27, 28]. No published data, however, exists on the utility of T2 mapping for these purposes. Utilization of this sequence in clinical practice when imaging patients with suspected or known hepatic fibrosis may represent a feasible non-invasive alternative to diagnose and monitor disease progression. T1 and T2 mapping sequences can be incorporated into standard MRI protocols without the need for an additional hardware, as in elastography. The goal of this study is two-fold: a) To evaluate the correlation between the stiffness values from MR elastography and T1/T2 relaxation times with clinical parameters of liver disease, including the MELD score, MELD-Na, and ALBI grade. 2. To evaluate to the role of MR elastography, T1 mapping and T2 mapping in predicting the presence of endoscopically visible esophageal varices.
Methods
Study design and patient population
Between June and December 2018, all patients with known or suspected hepatic fibrosis who underwent MR liver with elastography at our institution had an additional T1 mapping sequence (Look-Locker sequence) and T2 mapping sequence obtained as part of the standard protocol. There were a total of 226 patients, 102 of which were female and 114 were male, with an average age of 39 years (range: 20–80 years). Three patients were excluded from the final cohort. One was excluded due to failure of T1 mapping. The other two patients were status post Y-90 embolization with extensive post radioembolization changes precluding meaningful measurement of liver stiffness and T1/T2 relaxation times. The final cohort included 223 patients. The underlying etiology included non-alcoholic fatty liver disease (NAFLD) in 72 patients, hepatitis B infection in 37 patients, and hepatitis C infection in 30 patients. 31 patients had elevated liver function tests without a known etiology at the time of referral for MR elastography, 20 had a history of autoimmune hepatitis, including 1 with drug induced liver injury (DILI) overlap, 4 with primary biliary cholangitis (PBC) overlap and 1 with primary sclerosing cholangitis (PSC) overlap, and 10 had a history of significant alcoholism. Additional etiologies included primary biliary cholangitis [7], no known underlying disease [9], workup of liver mass [4], hemochromatosis [4] and unexplained cirrhosis [2].
Magnetic resonance imaging and imaging analysis
Liver MRI was performed on a 3 T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) and 1.5 T system (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) using the standard body and spine matrix coils. MR elastography utilized an acoustic driver system (Resoundant, Rochester, MN) with the passive driver placed at the patient’s right upper quadrant inducing shear waves at 60 Hz. A prototype 2D-SE-EPI sequence was acquired in each patient. Four individual slices are obtained each in a single breath hold, centered through the thickest portion of the liver with following parameters: TR/TE 1000/45 ms, flip angle: 90 degrees, FOV: typically 380 × 380 mm2, matrix: 100 × 100, slice thickness: 6 mm, fat saturation: SPAIR, wave frequency: 60 Hz, MEG frequency: 60 Hz, MEG amplitude: 36 mT/m, z-axis, GRAPPA acceleration factor: 2, acquisition time: 11 s.
Multi-echo Dixon mapping was also performed to evaluate the liver fat and iron content with the following parameters: TE 1.09/2.3/3.57/4.84/6.11/7.38 ms, TR 9.17 ms, flip angle: 4 degrees, FOV: 380 x 332 mm2, matrix: 160 x 111, slice thickness: 3 mm, number of slices: 72, CAIPIRINHA factor: 3, acquisition time: 19 s.
T1 mapping was performed using a prototype Look-Locker sequence. For each inversion pulse data were acquired for a single slice. Sequence parameters were as follows: TR 3 ms, TE 1.32 ms, multiple TIs at 122, 347, 572, 797, 1022, 1247, 1472, 1697, 1922, 2147, 2372, 2597, 2822, 3047, 3272 and 3497 ms; flip angle: 8 degrees; Matrix − 192 × 80; Number of slices: 4; Acquisition time: 18 s.
T2 mapping was performed with a free-breathing, fat suppressed, prototype radial TSE sequence. Sequence parameters were as follows: TR: 3300 ms (3T); 1850 ms (1.5T), FOV: 350 × 350 mm, Slice thickness: 6 mm, Number of radial views = 391, Matrix: 256 × 256; Number of slices: 14; Acquisition time: 2:15 minutes. Images with multiple TEs were reconstructed from the radial data using echo-sharing algorithm. T2 value were estimated from images with different effective TE using the exponential signal decay model, with the first echo excluded from the fitting.
Two readers (reader 1 with 9 years post-fellowship experience in abdominal imaging, and reader 2 a body MRI fellow), blinded to the histopathology or other clinical or laboratory findings, followed a set protocol of image review, which included measuring the mean liver stiffness using ROIs in the right hepatic lobe in an area devoid of large blood vessels both on the T1 map (for T1 relaxation time) and MRE stiffness map with 95% confidence marking (for liver stiffness measurements). This was performed directly on PACS. ROI was drawn in the region of liver away from the liver edge, devoid of vessels, bile duct and focal lesions. Wave images were also assessed to ensure coherent wave propagation in this region. ROIs were placed in the same location in the right lobe of the liver on MR elastography, T1 mapping and T2 mapping sequences with minimum ROI size of 5 cm2. To account for the influence of fat on T1 relaxation times, a dictionary using simulated signal curves at a given fat fraction (obtained from PDFF/HISTO) and T1 value was generated (assuming the T1 of fat being 290 ms at 3T and 230 ms at 1.5T). The corrected T1 values (corrected for fat) were used for statistical analysis.
In addition, both the readers evaluated the following qualitative parameters on MR imaging: cirrhotic morphology of the liver, spleen size, ascites, and presence of varices on MRI including the location (GE junction, or other).
Clinical data collection
A third-independent reader collected relevant clinical data, including serum albumin, bilirubin, sodium, INR, creatinine, and MELD score, if performed within 3 months of the MRI. Endoscopy was done in 78/223 (34.9%) of patients. The presence or absence of endoscopically visible esophageal varices were recorded.
Statistical analysis
Reader agreement was assessed in terms of the intraclass correlation coefficient (ICC) for the absolute agreement between single measures for numeric factors and using the linear weight kappa coefficient for the ordinal imaging-based assessment of varices. Associations among numeric imaging measures were assessed in terms of the Pearson and Spearman rank correlation coefficients. The utility of imaging measures for the detection of binary outcome measures (e.g., advanced fibrosis at biopsy) was tested using binary logistic regression and characterized in terms of area under the ROC curve (AUC). ROC analyses were conducted to identify cutoff values for liver MRE, T1 and T2 for discriminating subjects with and without endoscopic varices that were optimal in the sense of maximizing the Youden index or that were estimated to achieve specified target levels of sensitivity or specificity. Since reader-specific cutoff values would have limited clinical utility, this ROC analysis used the data from both readers combined in order to identify single cutoff values for each imaging feature that showed optimal performance across both readers. All statistical tests were conducted at the two-sided 5% significance level using SAS 9.4 software (SAS Institute, Cary, NC).
Results
There was good reader agreement for MR elastography (ICC estimate 0.84), and excellent agreement for liver T1 and T2 measurements (ICC estimates 0.94 and 0.96, respectively). Agreement for the presence of varices was moderate, with a kappa coefficient of 0.55. Table 1 provides the ICC estimates and the lower and upper limits of a 95% confidence interval.
Correlation between imaging and prognostic laboratory tests demonstrated varying results. Correlations between MRE and ALBI grade was significant and moderate for both readers: r = 0.39 (reader 1) and r = 0.37 (reader 2), both p < 0.05. For T1 relaxometry, correlation with ALBI grade was lower, with r = 0.22 and 0.20, p < 0.05, respectively for both readers. Results were similar for T2 relaxometry, with r = 0.17, p = 0.057 (reader 1), and r = 0.24, p < 0.05 (reader 2). Significant moderate correlations were found for both readers between MRE and the presence of varices on endoscopy: r = 0.28 (reader 1) and r = 0.30 (reader 2), both p < 0.05. Correlation between T1 relaxometry and endoscopic varices was slightly lower and not statistically significant. Correlation between T2 relaxometry and endoscopic varices was r = 0.42, p < 0.05, for reader 1, but lower and not significant for reader 2. Significant moderate correlation was found between MELD score and all three imaging techniques for both readers. For MRE, r = 0.35 (reader 1) and v0.28 (reader 2). For T1 relaxometry, r = 0.30 (reader 1) and r = 0.29 (reader 2), and for T2 relaxometry, r = 0.45 (reader 1) and r = 0.37 (reader 2). For MELD-Na score, there was even higher correlation with MRE, r = 0.49 (reader 1) and r = 0.40 (reader 2), both p < 0.05. Correlations between MELD-Na and both T1 and T2 relaxometry were likewise higher: for T1, r = 0.45 (reader 1) and r = 0.41 (reader 2), both p < 0.05 and for T2, r = 0.47 (reader 1), p < 0.05, and r = 0.35 (reader 2), p > 0.05. Correlations are listed in Table 2.
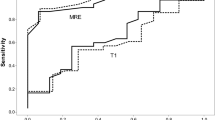
For both readers, MRE and T1 relaxometry were found to be significant predictors of identifying varices at endoscopy. For MRE, the AUC was 0.923 (reader 1) and 0.873 (reader 2), both p < 0.001. For T1 relaxometry, the AUC was 0.711 (reader 1) and 0.675 (reader 2), both p < 0.05. T2 relaxometry did not demonstrate significant prediction of the presence of varices at endoscopy for either reader. AUC values are listed in Table 3.
Several features identifiable on the MR imaging were found to significantly predict the presence of varices identified at endoscopy. Of the 78 patients who underwent endoscopy, 44 (56.4%) had no visible varices and 34 had varices (43.6%). The presence of cirrhotic morphology and spleen length were both significant predictors, with AUC of 0.654 and 0.610, respectively (p < 0.05). The presence of esophageal varices identifiable on MR was also a significant predictor for both readers, with AUC of 0.693 (reader 1) and 0.595 (reader 2), (p < 0.05). Subset analyses revealed that knowing the specific location of varices (GE junction, versus other portosystemic collaterals such as recanalized paraumbilical vein, splenorenal shunt etc.) was not informative for the prediction of endoscopic varices. The presence of abdominal ascites on MR yielded an AUC of 0.545, and was not statistically significant (Table 4).
Multivariable logistic regression model identified that spleen length and liver MRE were significant independent predictors of endoscopic varices for both readers with the type 3 p value of 0.007 (reader 1) and 0.009 (reader 2) for spleen length; and 0.018 and 0.019 for MRE (AUC 0.828 for reader 1 and 0.818 for reader 2).
A cutoff of > 4.5 kPa on MRE yielded a sensitivity of 79.4% and specificity of 85.2% for the presence of varices on endoscopy. A T1 relaxation time cutoff of > 783 ms yielded a sensitivity of 58.8% and specificity of 68.6% for the identifying varices on endoscopy. A T2 relaxation cutoff of > 50 ms gave a 22.2% sensitivity and 95.3% specificity for the presence of endoscopically detectable varices. Cutoff values estimated to achieve specified target levels of sensitivity or specificity and the estimated values of the specificity or sensitivity that would be achieved using the respective cutoff were calculated and are listed in Table 5.
Discussion
Using non-invasive MRI techniques to predict clinical outcomes has the potential to transform the care of patients living with chronic liver disease. Being able to prognosticate and risk stratify in this patient population would increase the high value MRI already has in diagnosing and staging liver disease. In our study, we demonstrated a moderate positive correlation between MRE and MELD-Na score, r = 0.40 and 0.49. Slightly lower but significant was the correlation between MRE and MELD, r = 0.35 (reader 1) and r = 0.28 (reader 2). These findings are similar to the previously published study by Poterucha, et al [29] which demonstrated a correlation of liver stiffness with MELD score of r = 0.48 (p = 0.002) in Fontan patients.
We found a significant moderate correlation between the stiffness values on MRE and ALBI grade (r = 0.37–0.39). ALBI grade is comparable to Child-Pugh classification in assessing the degree of liver dysfunction in patients with hepatocellular carcinoma, and that patients can be stratified into prognostic groups based this measure [7]. While MELD is tailored to those with end-stage liver disease, the ALBI grade can be more broadly applied to any patients with HCC. To our knowledge, MR elastography has not been correlated with the simplified ALBI grade in the literature. Our results are not surprising given the alterations in albumin and bilirubin frequently seen in those with advanced liver disease, and potentially suggests that higher liver stiffness identified on MRE may portend a worse prognosis among those with HCC.
Low stiffness values on transient elastography (Fibroscan) has been shown to have a high negative predictive value for clinically significant varices. The Baveno VI criteria recommends avoiding variceal screening endoscopy in patients with stiffness of < 20 kPa on transient elastography and platelet count of > 150,000 [11]. MR elastography, although not routinely incorporated in the determination of which patients will need the screening endoscopy, has been shown to be potentially beneficial in predicting the presence of portal hypertension and esophageal varices [16, 22,23,24,25, 30]. Our results corroborate these findings. We show the high utility of MRE for the prediction of varices at endoscopy, with AUC of 0.873-0.923. In addition, we found a significant moderate correlation between elevated stiffness at MRE and the presence of varices at endoscopy, r = 0.28–0.30. A cutoff of > 4.5 kPa on MRE yielded a sensitivity of 79.4% and specificity of 85.2% for the presence of varices on endoscopy, while a cutoff of > 5.76 kPa yielded a 95% specificity. Only 5% of patients with MRE stiffness values less than 3.7 kPa had varices in endoscopy, yielding a negative predictive value of 93.7% for any varices. Matsui et al [30] reported that a cutoff of 4.2 kPa yielded a sensitivity of 90%, specificity of 71%, PPV of 39% and NPV of 97% for any varices, and NPV of 99% for high risk varices. This cutoff, in conjunction with a platelet threshold of 18 × 104 yielded a 100% sensitivity for the presence of any and high risk varices and 100% NPV. Our results also suggest that a cutoff of 3.7 kPa may obviate the need for variceal screening, which would provide both time and cost savings and eliminate the potential risks involved with routine repeat endoscopy. We, however, did not evaluate the negative predictive value of MRE in differentiating those with high risk varices, which is expected to be higher.
MR relaxometry involves quantifying the T1 or T2 relaxation times of imaged tissue. T1 mapping is based on the premise that fibrosis results in alteration of the extracellular matrix of liver parenchyma, which leads to an increase in parenchymal T1 relaxation time [31]. Using the Look-Locker sequence [32], the T1 relaxation time (in milliseconds) is encoded into the signal intensity of the individual pixels, which can then easily be derived by drawing a region of interest on the image. Several prior studies have demonstrated T1 mapping to be a beneficial tool that can non-invasively stage liver fibrosis and monitor disease progression [17,18,19]. Like MR elastography, this technique has been shown to correlate with MELD score and Child-Pugh classification, although most of these studies evaluate the changes in T1 values after administration of Gd-EOB-DTPA contrast agent [27, 33,34,35].
In 2012, Heye, et al demonstrated significantly increased T1 relaxation times in cirrhotic livers relative to healthy controls, with T1 values measuring 852 ± 132 ms in cirrhotics versus 678 ± 45 ms in controls [28]. They also showed that T1 relaxation values can be used to stratify patients based on Child-Pugh scores, with significantly increased T1 values of those with class C disease compared with class A and B (956 ± 141 ms versus 816 ± 104 and 821 ± 132 ms, respectively). Haimerl, et al [25], in 2013, similarly demonstrated that T1 relaxation rates measured on Gd-EOB-DTPA-enhanced MR examinations increased with higher Child-Pugh score, with significant increases from class A to B and class B to C disease (335 ± 80 versus 431 ± 75 versus 557 ± 99 ms, respectively). However, Cassinoto et al. [18] demonstrated a much lower positive correlation of 0.30 between unenhanced liver T1 mapping and the MELD score, similar to our findings of r = 0.29 and 0.30. Furthermore, T1 mapping has demonstrated correlation with the degree of portal hypertension and has been used as a predictor of esophageal varices [17, 18, 26]. For example, Yoon, et al [26], demonstrated significantly higher pre-contrast T1 values in those with varices versus those without (951 ± 114 with varices vs 874 ± 105 without varices, p = 0.01). Cassinoto, et al [18], found an AUC of 0.75 for the ability of T1 mapping to predict the presence of large esophageal varices. Palaniyappan et al. showed that T1 relaxation time significantly correlated with hepatic venous pressure gradient (HVPG), the gold standard method to assess portal hypertension [36]. We demonstrated an AUC of 0.711 and 0.675 (for readers 1 and 2, respectively) for the prediction of endoscopically visible varices, which is not as high as MRE, but is nonetheless similar to currently published literature. T1 relaxometry has not been correlated with the ALBI grade in prior studies to our knowledge. Despite the significant moderate correlation found between ALBI grade and MRE, we found a lower correlation between the ALBI grade and T1 relaxometry—a low significant positive correlation of r = 0.22 and 0.20. Further studies are needed to determine the relationship of INR and creatinine (specific to the MELD score) and albumin (specific to the ALBI grade) to these findings.
Similar to T1 mapping, T2 mapping assumes that liver fibrosis results in alteration of parenchymal T2 relaxation times (due to high water content of the advanced fibrosis). The use of radial T2 FS sequence similarly enables T2 relaxation times to be encoded into the signal intensity of individual pixels in an image. This technique has been evaluated in diagnosing and staging liver fibrosis in both animal and human models with variable success [19, 20, 37]. There are limited data correlating T2 mapping with laboratory-based prognostic tests and the presence of varices. To our knowledge, there has been no study correlating T2 mapping with the MELD score or ALBI grade.
We demonstrate a significant moderate correlation between T2 mapping and the MELD score, although T2 mapping did not perform as well with the ALBI grade, with a significantly positive low correlation found for only one reader. In a 2019 study of pediatric patients with autoimmune liver disease, Dillman, et al, [23] found T2 mapping to be a suboptimal predictor of portal hypertension with an AUC of 0.63. This is similar to our ROC analysis demonstrating AUC of 0.612 and 0.524 for the prediction of varices at endoscopy. Lee et al. in their study in infants with cholestasis, showed limited utility of T2 relaxation times in staging liver fibrosis and differentiating patients with biliary atresia from normal controls [37].
Qualitative assessment of cirrhotic morphology, spleen length, and presence of varices on T1-weighted contrast-enhanced conventional MRI were all found to significantly predict the presence of varices identified at endoscopy, with AUC of 0.654, 0.610, and 0.693 respectively. Shin et al. found that spleen length and contrast-enhanced T1-weighted images have similar to higher accuracy for prediction of endoscopic varices (AUC 0.697 and 0.839 respectively). Our findings corroborate these results. In addition, on multivariable analyses, we found that spleen length and stiffness measurement on MRE were the only two significant predictors of endoscopic varices. Only one of our patients with endoscopic varices had low stiffness on MRE (2.2 kPa), however, also had a markedly enlarged spleen (17 cm craniocaudally) as well as visible varices at the GE junction and other regions in the upper abdomen on contrast-enhanced T1-weighted images. Previously published studies have suggested that portal hypertension (for which spleen length is an imaging marker), can precede the development of hepatic fibrosis [38, 39] and hence, spleen length in combination with stiffness measurements on MRE could potentially limit the ‘false-negative’ results based on stiffness measurements alone. Our patient with low stiffness of MRE with enlarged spleen and endoscopic varices was, however, eventually diagnosed with non-cirrhotic portal hypertension secondary to portal vein thrombosis. On the contrary, 8 out of 44 patients with no varices on endoscopy had stiffness values above 4 kPa (4.1–6.8 kPa). Only two of these patients had portosystemic collaterals (with no GE junction varices) and one had enlarged spleen (> 12.5 cm craniocaudally). Interpretation of elevated stiffness in combination in spleen length and visible GE junction varices on contrast-enhanced MRI, potentially can reduce the false-positive cases on MRE.
This study has several limitations. First, the endoscopy was performed in just over one-third of the patients (78/223; 34.9%). Endoscopy was performed as a part of clinical workup, by several operators (clinicians). Interobserver variability in finding endoscopic varices cannot be addressed. Also, imaging data were correlated to ‘any’ varices on endoscopy, without specific correlation to stage of endoscopic varices. Subset analyses for patients with clinically significant varices that require treatment was not performed. Second, hepatic venous pressure gradient (HVPG), the gold standard for evaluate portal hypertension was not measured or correlated. Third, role of serum platelet count, a common variable used in other studies was not evaluated in conjunction with imaging parameters to predict endoscopic varices.
Conclusion
MR elastography, T1 and T2 relaxometry all demonstrates promise in predicting the clinical outcomes of patients with chronic liver disease. While all techniques demonstrates moderate correlation with the MELD score, MRE demonstrates superior correlation with the ALBI grade compared to T1 and T2 relaxometry. MRE also demonstrates a superior ability to predict the presence of varices at endoscopy compared to T1 and T2 mapping, with a cutoff of > 4.5 kPa yielding a sensitivity of 79.4% and specificity of 85.2% for the presence of varices on endoscopy. On multivariate analyses, stiffness measurements from MRE and spleen length were the only two significant predictors of endoscopic varices.
References
Albanis E, Friedman SL. Hepatic fibrosis. Pathogenesis and principles of therapy. Clin Liver Dis. 2001;5(2):315–34, v-vi.
Mallat A, Lotersztajn S. Cellular mechanisms of tissue fibrosis. 5. Novel insights into liver fibrosis. Am J Physiol Cell Physiol. 2013;305(8):C789–99.
Ble M, Procopet B, Miquel R, Hernandez-Gea V, Garcia-Pagan JC. Transjugular liver biopsy. Clin Liver Dis. 2014;18(4):767–78.
Chi H, Hansen BE, Tang WY, Schouten JN, Sprengers D, Taimr P, et al. Multiple biopsy passes and the risk of complications of percutaneous liver biopsy. Eur J Gastroenterol Hepatol. 2017;29(1):36–41.
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–6.
Kamath PS, Kim WR, Advanced Liver Disease Study G. The model for end-stage liver disease (MELD). Hepatology. 2007;45(3):797–805.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–8.
Hiraoka A, Michitaka K, Kumada T, Izumi N, Kadoya M, Kokudo N, et al. Validation and Potential of Albumin-Bilirubin Grade and Prognostication in a Nationwide Survey of 46,681 Hepatocellular Carcinoma Patients in Japan: The Need for a More Detailed Evaluation of Hepatic Function. Liver Cancer. 2017;6(4):325–36.
Simonetto DA, Liu MF, Kamath PS. Portal Hypertension and Related Complications: Diagnosis and Management. Mayo Clinic Proceedings. 2019;94(4):714–26.
Cardenas A, Mendez-Bocanegra A. Report of the Baveno VI Consensus Workshop. Ann Hepatol. 2016;15(2):289–90.
de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52.
Augustin S, Pons M, Genesca J. Validating the Baveno VI recommendations for screening varices. J Hepatol. 2017;66(2):459–60.
Rustogi R, Horowitz J, Harmath C, Wang Y, Chalian H, Ganger DR, et al. Accuracy of MR elastography and anatomic MR imaging features in the diagnosis of severe hepatic fibrosis and cirrhosis. J Magn Reson Imaging. 2012;35(6):1356–64.
Venkatesh SK, Ehman RL. Magnetic resonance elastography of liver. Magn Reson Imaging Clin N Am. 2014;22(3):433–46.
Yasar TK, Wagner M, Bane O, Besa C, Babb JS, Kannengiesser S, et al. Interplatform reproducibility of liver and spleen stiffness measured with MR elastography. J Magn Reson Imaging. 2016;43(5):1064–72.
Gharib AM, Han MAT, Meissner EG, Kleiner DE, Zhao X, McLaughlin M, et al. Magnetic Resonance Elastography Shear Wave Velocity Correlates with Liver Fibrosis and Hepatic Venous Pressure Gradient in Adults with Advanced Liver Disease. Biomed Res Int. 2017;2017:2067479.
Luetkens JA, Klein S, Traber F, Schmeel FC, Sprinkart AM, Kuetting DLR, et al. Quantification of Liver Fibrosis at T1 and T2 Mapping with Extracellular Volume Fraction MRI: Preclinical Results. Radiology. 2018;288(3):748-54.
Cassinotto C, Feldis M, Vergniol J, Mouries A, Cochet H, Lapuyade B, et al. MR relaxometry in chronic liver diseases: Comparison of T1 mapping, T2 mapping, and diffusion-weighted imaging for assessing cirrhosis diagnosis and severity. Eur J Radiol. 2015;84(8):1459-65.
Chow AM, Gao DS, Fan SJ, Qiao Z, Lee FY, Yang J, et al. Measurement of liver T(1) and T(2) relaxation times in an experimental mouse model of liver fibrosis. J Magn Reson Imaging. 2012;36(1):152-8.
Guimaraes AR, Siqueira L, Uppal R, Alford J, Fuchs BC, Yamada S, et al. T2 relaxation time is related to liver fibrosis severity. Quantitative Imaging in Medicine and Surgery. 2016;6(2):103-14.
Pavlides M, Banerjee R, Tunnicliffe EM, Kelly C, Collier J, Wang LM, et al. Multiparametric magnetic resonance imaging for the assessment of non-alcoholic fatty liver disease severity. Liver Int. 2017;37(7):1065-73.
Morisaka H, Motosugi U, Ichikawa T, Sano K, Ichikawa S, Araki T, et al. MR-based measurements of portal vein flow and liver stiffness for predicting gastroesophageal varices. Magn Reson Med Sci. 2013;12(2):77-86.
Dillman JR, Serai SD, Trout AT, Singh R, Tkach JA, Taylor AE, et al. Diagnostic performance of quantitative magnetic resonance imaging biomarkers for predicting portal hypertension in children and young adults with autoimmune liver disease. Pediatr Radiol. 2019;49(3):332-41.
Yin M, Kolipaka A, Woodrum DA, Glaser KJ, Romano AJ, Manduca A, et al. Hepatic and splenic stiffness augmentation assessed with MR elastography in an in vivo porcine portal hypertension model. J Magn Reson Imaging. 2013;38(4):809-15.
Sun HY, Lee JM, Han JK, Choi BI. Usefulness of MR elastography for predicting esophageal varices in cirrhotic patients. J Magn Reson Imaging. 2014;39(3):559-66.
Yoon JH, Lee JM, Paek M, Han JK, Choi BI. Quantitative assessment of hepatic function: modified look-locker inversion recovery (MOLLI) sequence for T1 mapping on Gd-EOB-DTPA-enhanced liver MR imaging. European Radiology. 2016;26(6):1775-82.
Haimerl M, Verloh N, Zeman F, Fellner C, Muller-Wille R, Schreyer AG, et al. Assessment of clinical signs of liver cirrhosis using T1 mapping on Gd-EOB-DTPA-enhanced 3T MRI. PLoS One. 2013;8(12):e85658.
Heye T, Yang SR, Bock M, Brost S, Weigand K, Longerich T, et al. MR relaxometry of the liver: significant elevation of T1 relaxation time in patients with liver cirrhosis. Eur Radiol. 2012;22(6):1224–32.
Poterucha JT, Johnson JN, Qureshi MY, O’Leary PW, Kamath PS, Lennon RJ, et al. Magnetic Resonance Elastography: A Novel Technique for the Detection of Hepatic Fibrosis and Hepatocellular Carcinoma After the Fontan Operation. Mayo Clin Proc. 2015;90(7):882–94.
Matsui N, Imajo K, Yoneda M, Kessoku T, Honda Y, Ogawa Y, et al. Magnetic resonance elastography increases usefulness and safety of non-invasive screening for esophageal varices. J Gastroenterol Hepatol. 2018;33(12):2022–8.
Li Z, Sun J, Hu X, Huang N, Han G, Chen L, et al. Assessment of liver fibrosis by variable flip angle T1 mapping at 3.0T. J Magn Reson Imaging. 2016;43(3):698–703.
Deichmann R, Haase A. Quantification of T1 Values by Snapshot-Flash Nmr Imaging. Journal of Magnetic Resonance. 1992;96(3):608–12.
Haimerl M, Verloh N, Fellner C, Zeman F, Teufel A, Fichtner-Feigl S, et al. MRI-based estimation of liver function: Gd-EOB-DTPA-enhanced T1 relaxometry of 3T vs. the MELD score. Sci Rep. 2014;4:5621.
Ding Y, Rao SX, Chen C, Li R, Zeng MS. Assessing liver function in patients with HBV-related HCC: a comparison of T(1) mapping on Gd-EOB-DTPA-enhanced MR imaging with DWI. Eur Radiol. 2015;25(5):1392–8.
Katsube T, Okada M, Kumano S, Hori M, Imaoka I, Ishii K, et al. Estimation of Liver Function Using T1 Mapping on Gd-EOB-DTPA-Enhanced Magnetic Resonance Imaging. Investigative Radiology. 2011;46(4):277–83.
Palaniyappan N, Cox E, Bradley C, Scott R, Austin A, O’Neill R, et al. Non-invasive assessment of portal hypertension using quantitative magnetic resonance imaging. J Hepatol. 2016;65(6):1131–9.
Lee MJ, Kim MJ, Yoon CS, Han SJ, Park YN. Evaluation of liver fibrosis with T2 relaxation time in infants with cholestasis: comparison with normal controls. Pediatr Radiol. 2011;41(3):350–4.
Nedredal GI, Yin M, McKenzie T, Lillegard J, Luebke-Wheeler J, Talwalkar J, et al. Portal hypertension correlates with splenic stiffness as measured with MR elastography. J Magn Reson Imaging. 2011;34(1):79–87.
Zaman A, Hapke R, Flora K, Rosen HR, Benner K. Factors predicting the presence of esophageal or gastric varices in patients with advanced liver disease. Am J Gastroenterol. 1999;94(11):3292–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoffman, D.H., Ayoola, A., Nickel, D. et al. MR elastography, T1 and T2 relaxometry of liver: role in noninvasive assessment of liver function and portal hypertension. Abdom Radiol 45, 2680–2687 (2020). https://doi.org/10.1007/s00261-020-02432-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02432-7