Abstract
Purpose
To determine how small bowel neuroendocrine neoplasms (SBNEN’s) are diagnosed and examine the effect of CT enterography (CTE) on diagnosis and rates of disease-free survival.
Methods
Histopathologically-confirmed SBNEN’s diagnosed at our institution between 1996 and 2016 were identified. Clinical presentation, radiology, endoscopy, surgery, and pathology reports were reviewed and compared between consecutive 5-year periods.
Results
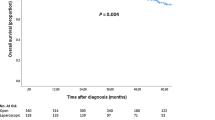
Of the 178 SBNEN initially diagnosed at our institution, the incidence increased 12-fold from 9 (during 1996–2000) to 114 (during 2011–2016). Comparing the first 5 to the last 5 years, GI bleeding and abdominal pain increased significantly as indications (with both increasing from 0 to > 25%, p ≤ 0.023). Initial diagnosis by radiology increased 2-fold [from 33% (n = 3) to 66% (n = 75); p = 0.263]. Detection of a small bowel mass and the suggestion that SBNEN was present varied significantly between imaging modalities (p < 0.0001; CTE − 95% (52/55) and 91% (50/55) vs. abdominal CT 45% (37/85) and 35% (29/85), respectively). Recurrence rates increased with SBNEN size (p = 0.012; e.g., of SBNEN diagnosed by endoscopy, 18% of SBNEN measuring 0.6 ± 0.3 cm recurred vs. 75% measuring 3.7 ± 1.0 cm). Rates of disease-free survival, and the incidence of local and liver metastases were decreased when tumors were first identified by CTE rather than other CT/MR imaging modalities (p = 0.0034, 0.0475, and 0.0032, respectively).
Conclusion
There has been a dramatic increase in SBNENs detected by CTE and endoscopy over the last 20 years. SBNEN’s detected by CTE and small tumors detected at endoscopy have longer disease-free survival after surgical resection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasms have now replaced adenocarcinoma as the most common small bowel neoplasm [1]. Although they only account for 1.2–1.5% of all gastrointestinal tumors, their incidence in the United States has increased by more than 300% in the last 35 years, with the current age-adjusted incidence of primary small bowel neuroendocrine neoplasms (SBNEN’s) estimated to be 4.7 per 100,000 [2]. Better detection of SBNEN, by increased use of endoscopy and improved cross-sectional imaging, may in part explain this change.
Since the 2015 American College of Gastroenterology’s (ACG) recommendation to use CT enterography (CTE) as a primary imaging modality for patients with suspected small bowel bleeding, there has been a dramatic increase in the use of CTE [3]. Compared to modalities such as the routine abdominopelvic CT (APCT) or video capsule endoscopy (VCE), CTE has been found to be more effective in identifying small bowel tumors as a cause of small bowel bleeding [3,4,5], and can be useful when these tests are negative or inconclusive [6]. Beginning in 2006, our institution began to use multiphase CTE (mpCTE) as a routine diagnostic test for patients with suspected small bowel bleeding.
Vasconcelos et al. recently found that since the introduction of mpCTE for GI bleeding at their institution, the incidence of small bowel gastrointestinal stromal tumors (GIST) has risen dramatically [7]. In their retrospective observational study, they found that the large majority of GISTs were diagnosed after the introduction of mpCTE and were smaller in size and lower in biologic aggressiveness.
Given improved cross-sectional imaging and increased use of CTE for suspected small bowel bleeding, we conducted a retrospective, observational review of small bowel neuroendocrine neoplasms to determine the (1) incidence of SBNEN first diagnosed at our institution over the last 20 years by various imaging modalities, (2) the impact of CTE and endoscopy on the diagnosis of SBNEN, and (3) the impact of CTE and endoscopy on the rates of disease-free survival and incidence of liver and local metastases.
Methods
Following approval by the Institutional Review Board, patients with histologically proven SBNEN from January 1996 to February 2016 were retrospectively identified via search of our institution’s surgical pathology database. The patient inclusion criteria were as follows: (1) age > 18 years, (2) histopathological proof of SBNEN, (3) initial diagnosis of SBNEN at our institution, and (4) record of consent to retrospective evaluation of medical records for research purposes. We excluded patients with neuroendocrine neoplasms at locations other than the small bowel (e.g., pancreas), SBNEN with histological findings suggestive of mixed pancreatic origin, and those without pathologic confirmation of SBNEN.
Individual medical records were reviewed to collect information from clinical, radiology, pathology, and surgical reports. The patient’s sex, age, and MEN-1 status were recorded. Presenting signs and symptoms, recorded in a non-exclusive fashion, included GI bleeding, small bowel obstruction, nausea/vomiting, abdominal pain, diarrhea, and when appropriate, asymptomatic. The date of diagnosis was defined in this study as the date the pathologic specimen was obtained. Patients referred with a pre-existing diagnosis of SBNEN were excluded to eliminate the bias potentially introduced by including patients referred to our institutions for treatment of more advanced disease and to ensure absence of prior treatment.
The procedure or imaging modality used to diagnose SBNEN at our institution was recorded as endoscopy (EGD and/or colonoscopy), surgery, or radiologic imaging. Radiologic imaging modalities were further categorized as CT enterography, multiphase CT enterography, MR enterography, routine abdominopelvic CT, and CT angiography. No oral contrast was used for all CT angiography studies. For routine abdominopelvic CT studies, either two bottles of water or two bottles of water with dilute iodine solution (approximately 1000 cc) was administered per protocol for gastrointestinal tract distension. For MR or CT enterography exams, patients ingested approximately 1350 cc of a neutral (for CT) or biphase (for MR) oral contrast agent followed by ingestion of 500 cc water over one hour prior to imaging, as has been previously described [5]. All clinical and imaging reports were reviewed to confirm if the interpreting physician/radiologist identified imaging abnormalities reflecting SBNEN at the time of diagnosis.
Characteristics of the primary SBNEN tumor and extent of disease at the time of diagnosis was based on all available imaging prior to surgical resection, as well as surgical and endoscopic reports. Distribution of the primary and metastatic SBNEN was categorized as limited to the small bowel (solitary or multifocal), small bowel involvement and mesenteric nodal metastases, small bowel involvement and liver metastases (with or without mesenteric nodal metastases), and small bowel involvement and non-liver visceral metastases (with or without mesenteric nodal metastases). All clinical follow-up after resection was reviewed and recorded. Data relating to diagnosis and follow-up were compared between patients diagnosed in consecutive 5-year time periods over the course of the study.
Statistical analysis
Patient demographics including age and sex were abstracted. All statistical tests of association, including for tumor location, year of diagnosis, clinical presentation, method of initial diagnosis, imaging modality, tumor size, disease location/spread and follow-up status, were completed by Kruskal–Wallis test or chi-square test, as appropriate. Diagnosis year was grouped into 5-year intervals. Tumor size was grouped into quartiles. All statistical analysis was performed using SAS software version 9.4 (SAS Institute Inc, Cary, NC).
Results
From 1996 to 2016, there were 294 histologically proven SBNEN that underwent endoscopic or radiologic imaging at our institution. Of these, 178 patients were diagnosed with a SBNEN at our institution, and this cohort serves as the basis for our subsequent retrospective observational evaluation. The mean patient age was 62 (SD 13 years) and 48% (n = 86) were female. Over the 20 years examined, the number of SBNEN increased over 12- fold from 9 (between 1996 and 2000) to 114 (between 2011 and 2016; Fig. 1). Additionally, the incidence in the initial diagnosis of a SBNEN as a function of all SBNEN’s seen at our institution increased significantly over time: 9/15 (60%) patients between 1996 and 2000; 26/52 (50%) between 2001 and 2005; 29/58 (50%) between 2006 and 2010; and 114/168 (68%) between 2011 and 2016 (p = 0.031).
Diagnosis of SBNEN
Abdominal pain was the most common presenting symptom, occurring in approximately one-third of patients (Table 1). Over the 20 years of the study, GI bleeding significantly increased as a presenting symptom (0% (0/9) in 1996–2000 to 25.4% (29/114) in 2011–2016, p = 0.023) as did abdominal pain (0% (0/0) in 1996–2000 to 26.3% (30/114) in 2011–2016, p = 0.0026). Diarrhea decreased slightly but significantly (from 33 to 22%, p = 0.009). The remaining presenting symptoms did not significantly change over time. While the number of SBNEN diagnosed by endoscopy increased in each 5 year increment, the proportion first diagnosed with endoscopy tended to decrease over time (33.3% in 1996–2000, 23.7% in 2011–2016) while the proportion initially diagnosed by cross-sectional radiologic imaging increased nearly two-fold (33.3% (3/9) in 1996–2000 to 65.8% (75/114) in 2011–2016, p = 0.263) (Table 1, Figs. 2, 3).
Endoscopic image of 6 mm incidentally discovered Grade I duodenal neuroendocrine tumor discovered as part of workup for bariatric surgery. After biopsy, a CT demonstrated absence of pancreatic or duodenal mass and no suspicious lymph nodes. Transduodenal submucosal excision demonstrated 2 mm of residual tumor. Patient was free of disease over subsequent 2 years and 8 months of clinical follow-up
To determine whether the use of certain cross-sectional imaging modalities were associated with different size SBNEN lesions, a comparison of the largest detected lesion size per patient between mpCTE/CTE imaging modalities and routine APCT imaging was performed. In the patients undergoing CTE/mpCTE, the average largest lesion was 1.8 cm (SD = 0.8; 25th/75th percentile: 1.2 cm/2.2 cm). These results are nearly identical to the 85 patients who underwent routine APCT imaging (mean size 1.8 cm (SD = 1.2); 25th/75th percentile: 1.2 cm/2.4 cm). Despite these similarities in size, detection of a small bowel mass and suggestion that it was a SBNEN varied significantly between imaging modalities (p < 0.0001; Table 2). Most importantly, however, of the 178 patients, 55 received CT enterography (CTE) or multiphase-CTE (mpCTE) imaging, with 94.5% (n = 52) of these imaging reports identifying a small bowel mass and 90.9% (n = 50) specifically mentioning SBNEN as the diagnosis. In contrast, 85 of these patients underwent routine abdominopelvic CT, with only 44.6% (n = 37) of these clinical reports identifying a small bowel mass and 34.9% (n = 29) specifying that SBNEN as a potential diagnosis (Table 2). Endoscopy identified more duodenal lesions (58.2%; 23/55) than other diagnostic modalities (p < 0.0001; Figs. 2, 3).
57-year-old male underwent upper endoscopy for surveillance of esophageal varices with duodenal polyp detected incidentally in the duodenal bulb. Polyp was examined endosonographically prior to submucosal injection of methylene blue using endoscopic ultrasound guidance followed by snare mucosal resection. Histopathology demonstrated grade 1 neuroendocrine neoplasm. Patient was negative during endoscopic surveillance of over 3 years
Initial characteristics of SBNEN at time of diagnosis
There were differences in stage of disease between the modalities used to identify SBNEN (p = 0.02). When lesions were first identified with endoscopy, 56.8% (n = 25) of patients had a single neuroendocrine neoplasm confined exclusively to the small bowel, and only 15.9% (7/46) had metastatic disease. When lesions were first detected by imaging or surgery, only 31.1% of small bowel neoplasms were confined to the small bowel (41/132), with another 41.7% (55/132) having small bowel and mesenteric nodal involvement, and the remainder (25%; 33/132) having extra nodal metastatic disease. The stage of disease was not significantly different between alternative diagnostic modalities when lesions were detected by CTE, non-CTE imaging, or surgery. Table 3 shows the overall stage of disease at presentation by presence of symptoms and GI bleeding, as well as location within the small bowel. While the majority of SBNENs were associated with symptoms (80%; 142/178), no one symptom correlated with initial staging. Asymptomatic patients had similar rates of local and distant spread when compared to other presentations. When patients presented with suspected small bowel bleeding (n = 34), there tended to be a lower proportion of patients with distant metastases (14.7% (5/34) vs. 24.5% (35/144); p = 0.4223). About half of these patients had ileal primary tumors, and just under one-third had duodenal tumors (Table 3; Fig. 4). Of the 34 patients presenting with small bowel bleeding, 5 (15%) had a SBNEN in the duodenum compared to 19 (55%) in the ileum (p = 0.023), with 9% of the duodenal SBNEN’s presenting with small bowel bleeding and 22% of ileal SBNEN’s having small bowel bleeding (Fig. 5).
45-year-old male presenting with GI bleed with multiple negative prior exams including MR enterography, small bowel capsule endoscopy, and anterograde double balloon endoscopy. An enhancing 1.5 cm ileal mass was identified via triple phase CT enterography with the radiologic report suggesting small bowel neuroendocrine neoplasm, with intermediate (Grade 2) neuroendocrine neoplasm confirmed at surgery
79-year-old male with suspected small bowel bleeding underwent multiphase CT enterography, which identified two enhancing ileal polyps and regional mesenteric lymphadenopathy typical for multifocal ileal neuroendocrine neoplasm with regional mesenteric metastases. Surgery and histopathology confirmed an intermediate grade well-differentiated neuroendocrine tumor at these locations
Follow-up of small bowel neuroendocrine neoplasms
Of the 178 SBNEN patients, 150 had clinical follow-up. The mean and median number of days between initial diagnosis and last clinical follow-up were 969 (± 982) days and 662 days, respectively. At the last clinical follow-up, 32.7% (n = 49) had recurrence (at any site after surgery), 12.7% (n = 19) had nodal/mesenteric metastases, 16.7% (n = 25) had liver metastases, and 10.7% (n = 16) had metastases to non-liver visceral organs.
In order to ascertain if the size of SBNEN affected the likelihood of recurrence, the sizes of the different primary SBNEN’s at presentation were separated into quartiles (specifically, 0.3–1.1 cm, 1.2–1.5 cm, 1.6–2.2 cm, and 2.3–7.0 cm). There was an increase in the likelihood for recurrence as tumor size increased (26.5%, n = 9 in the 1st quartile [0.3–1.1 cm] vs. 59.3%, n = 16 in the 4th quartile [2.3 cm and greater in size]; p = 0.012; Table 4). In a subcohort analysis of the 39 SBNEN patients initially diagnosed with endoscopy, the size of the primary tumor was only available for 25 patients, with 11/25 (44%) being small and in the first quartile (1.1 cm and smaller). Recurrence at follow-up was 75% (n = 3) in the 4th quartile [2.3 cm and greater in size] compared to only 18.2% (n = 2) of the 1st quartile [1.1 cm and less in size] (p = 0.20).
Of the 96 SBNEN patients initially diagnosed by imaging, 41 were diagnosed by mpCTE/CTE imaging, and 54 were diagnosed by other CT or MR imaging modalities. At follow-up, patients initially diagnosed by mpCTE/CTE were less likely to recur (14.6% vs. 42.6%; p = 0.0034), or develop nodal/mesenteric metastases (4.9% vs. 18.5%; p = 0.0475), or liver metastases (2.4% vs. 24.1%; p = 0.0032) compared to patients initially diagnosed by other imaging modalities (Table 5). There was not a significant difference between patients without recurrence based on symptoms of initial presentation; GI bleed or other symptoms (77.4% vs. 64.7%, respectively, p = 0.179). However, only 6.5% (n = 2) patients with GI bleed had liver metastases at follow-up, compared to the 19.3% (n = 23) in patients who presented with other symptoms (p = 0.087).
Discussion
Our study found a dramatic increase in the incidence of SBNEN initially diagnosed at our institution over the two decades of our retrospective observational study—a greater than twelve-fold increase when comparing patients diagnosed in the first versus last five years. When comparing the procedure or imaging modality used for the initial diagnosis of SBNEN over this same time interval, we found that the proportion of SBNEN’s initially identified by cross-sectional imaging increased from 33% to 66%, while those identified at endoscopy decreased slightly. Of the imaging modalities, CTE detected and correctly identified more tumors as SBNEN than routine abdominal CT. Importantly, when SBNEN’s were diagnosed with CTE, they were less likely to have recurrence or nodal or hepatic metastases. Similar findings were observed for small SBNENs diagnosed at endoscopy.
The increased detection of SBNEN in our study mirrors the increasing incidence reported in the general population. The Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute reported that in a series of 35,618 tumors, the age-adjusted incidence of SBNENs increased from 1.09/100,000 in 1973 to 5.25/100,000 in 2004 [2]. The increased detection of SBNEN in our study correlated with routine use of CTE for small bowel imaging and the routine use of mpCTE for suspected small bowel bleeding at our institution. The increased detection of SBNEN at our institution may also result from increased incidence of SBNEN in our tertiary care population.
CTE is specifically designed to evaluate the small bowel wall and has been proven effective for detection of a variety of bowel pathologies, including small bowel masses [5, 8]. Our study found that CTE and mpCTE detected and correctly identified more SBNEN than routine abdominal CT. The 44.6% rate of diagnosis of SBNEN by routine abdominal CT identified in our study mirrors a previous study conducted by Dahdaleh et al, which found that a primary SBNEN within the small bowel was found in 27/56 (48%) of cases using routine CT with positive oral contrast [9]. This difference between CTE/mpCTE and routine abdominal CT may be secondary to a combination of both imaging technique and imaging interpretation. At our institution, abdominal CT studies are read by the general pool of radiologists, while the majority of CTE and mpCTE studies are read by dedicated radiologists specialized in gastrointestinal radiology.
The proportion of SBNEN’s diagnosed by endoscopy decreased slightly over the course of our study, but nevertheless increased substantially during each 5-year time period. The endoscopic examinations in our study included routine EGD and colonoscopy, which can only evaluate a small fraction of the small bowel. Evaluation of the entire small bowel is important as the SEER program found that the incidence of duodenal SBNEN was 0.19/100,000 and the incidence of jejunal/ileal SBNEN was 0.67/100,000 [2]. Importantly, our study found that the majority of duodenal SBNEN’s are diagnosed with endoscopy. Small duodenal SBNEN’s may represent a unique subset of SBNEN’s with decreased risk and potential for safe endoscopic removal [10]. When a duodenal SBNEN is detected at endoscopy, multiphasic imaging of the pancreas is required to insure the endoscopic mass does not represent a pancreatic neuroendocrine neoplasm invading the duodenum.
Newer endoscopy techniques such as video capsule endoscopy (VCE) and double balloon endoscopy (DBE) also have the potential to evaluate the entire small bowel. VCE is effective for identifying a variety of small bowel pathologies and is considered a complementary study to CTE for evaluation of suspected small bowel bleeding [11, 12]. CTE is typically faster and easier to perform than VCE, and it may have an advantage in detection of small bowel masses, many of which can be submucosal, including small bowel neuroendocrine neoplasms and gastrointestinal stromal tumors [5]. DBE is considered the gold standard for evaluation of the small bowel [13]. A study conducted by Manguso et al demonstrated that DBE is significantly better at identifying primary SBNEN than routine abdominal CT (not specifically CTE) or MRI [14]. DBE may be limited due to local expertise and availability; due to its invasive nature, DBE should only be utilized to evaluate clinically significant indeterminate abnormalities by imaging or to evaluate symptomatic patients without an identifiable primary tumor by imaging [13, 14].
Epidemiologic study using the SEER database has shown that there is a general trend towards diagnosing neuroendocrine tumors at earlier disease stages and with lower grades [15]. Patients with lower stage and grade of disease have better overall survival [15]. The increased incidence of detecting low grade disease is thought to be due to improved ability to detect early and asymptomatic disease, as well as increased awareness of the appearance of primary small bowel tumors on imaging. For example, patients diagnosed with SBNEN by CTE/mpCTE had better prognosis (suggesting lower disease stage and grade) at follow-up compared to individuals diagnosed by other imaging modalities. MpCTE is frequently used to evaluate patients with suspected small bowel bleeding at our institution, and these two factors are likely inter-related in their association with an improved prognosis. Moreover, mpCTE/CTE modalities at our institution are specifically read by gastrointestinal radiologists who are more familiar with the imaging manifestations of small bowel pathology, which likely further contributes to improved diagnosis.
In a retrospective review of 75 patients with duodenal SBNEN, Untch et al found that only tumor size and tumor grade were significantly associated with recurrence [16]. When comparing the size of the primary SBNEN lesions in our study, we also found that regardless of diagnostic modality, patients diagnosed with smaller lesions have longer disease-free survival. When separating SBNEN size by quartiles, there was a significant increase in the recurrence rate once the primary tumor exceeds 2.3 cm in size. This finding emphasizes the need to develop CTE protocols designed to detect small bowel masses of this size and smaller. It also raises the possibility that smaller SBNEN’s have less malignant potential and may require a less aggressive approach to management, particularly for patients with significant comorbidities or contraindications to surgery.
Recently, the diagnosis and management of NEN’s has witnessed a paradigm shift with the USFDA approval of a 68Ga-labeled somatostatin analogue, DOTATATE [DOTA-Tyr3-octreotate]), in June 2016. PET imaging with 68Ga-DOTATATE is based on over-expression of somatostatin receptors) by NENs. In general, well-differentiated NENs tend to have high expression of SSTRs and poorly differentiated neuroendocrine carcinomas tend to have lower expression. 68Ga-DOTATATE PET is considered complementary to cross-sectional imaging with CT or MR. It is indicated for noninvasive confirmation of diagnosis in equivocal cases or for masses that are not amenable to biopsy [17]. Given the higher staging accuracy of 68Ga-DOTATATE PET compared to cross-sectional imaging [18, 19], 68Ga-DOTATATE PET has become the reference standard for staging of SBNENs detected by cross-sectional imaging, especially prior to surgery. This imaging modality is particularly helpful, as SBNEN is not infrequently multifocal, and 68Ga-DOTATATE PET could help identify unsuspected synchronous tumors. The increasing utilization 68Ga-DOTATATE PET is likely to further increase the detection of SBNEN in practice. This study will serve as a useful baseline to track increased diagnosis of SBNEN over time with this new modality.
Our study has limitations, with the principal limitation being that it is a retrospective observational study. Furthermore, although all pathology reports confirmed an immunohistochemical diagnosis of SBNEN, not all pathology reports provided a specific grade for each SBNEN. Some of the SBNEN diagnoses included in this study were based on sub-centimeter endoscopic samples. There may be overestimation of the relative performance of CTE compared to routine abdominopelvic CT as CTE exams were interpreted by subspecialized GI radiologists. The data regarding the type of oral contrast (water or dilute iodine solution) used in routine abdominopelvic CT studies were not collected in our study.
Conclusions
In the last two decades, there has been a dramatic increase (over 12-fold) in the diagnosis of SBNENs diagnosed at our institution, especially by CTE/mpCTE in patients with suspected small bowel bleeding. SBNEN detection and correct identification are more frequent with CTE/mpCTE compared to routine abdominopelvic CT. Patients with smaller SBNEN, and with SBNEN detected at either endoscopy or CTE/mpCTE, have longer periods of disease-free survival.
References
Bilimoria KY, Bentrem DJ, Wayne JD, Ko CY, Bennett CL, Talamonti MS (2009) Small bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg 249 (1):63–71.
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26 (18):3063–3072.
Gerson LB, Fidler JL, Cave DR, Leighton JA (2015) ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol 110 (9):1265–1287; quiz 1288.
Hakim FA, Alexander JA, Huprich JE, Grover M, Enders FT (2011) CT-enterography may identify small bowel tumors not detected by capsule endoscopy: eight years experience at Mayo Clinic Rochester. Dig Dis Sci 56 (10):2914–2919.
Huprich JE, Fletcher JG, Fidler JL, Alexander JA, Guimaraes LS, Siddiki HA, McCollough CH (2011) Prospective blinded comparison of wireless capsule endoscopy and multiphase CT enterography in obscure gastrointestinal bleeding. Radiology 260 (3):744–751.
Agrawal JR, Travis AC, Mortele KJ, Silverman SG, Maurer R, Reddy SI, Saltzman JR (2012) Diagnostic yield of dual-phase computed tomography enterography in patients with obscure gastrointestinal bleeding and a non-diagnostic capsule endoscopy. J Gastroenterol Hepatol 27 (4):751–759.
Vasconcelos RN, Dolan SG, Barlow JM, Wells ML, Sheedy SP, Fidler JL, Hansel S, Harmsen S, Fletcher JG (2017) Impact of CT enterography on the diagnosis of small bowel gastrointestinal stromal tumors. Abdom Radiol (NY) 42 (5):1365–1373.
Paulsen SR, Huprich JE, Fletcher JG, Booya F, Young BM, Fidler JL, Johnson CD, Barlow JM, Earnest Ft (2006) CT enterography as a diagnostic tool in evaluating small bowel disorders: review of clinical experience with over 700 cases. Radiographics 26 (3):641–657; discussion 657–662.
Dahdaleh FS, Lorenzen A, Rajput M, Carr JC, Liao J, Menda Y, O’Dorisio TM, Howe JR (2013) The value of preoperative imaging in small bowel neuroendocrine tumors. Ann Surg Oncol 20 (6):1912–1917.
Scherer JR, Holinga J, Sanders M, Chennat J, Khalid A, Fasanella K, Singhi AD, McGrath K (2015) Small duodenal carcinoids: a case series comparing endoscopic resection and autoamputation with band ligation. J Clin Gastroenterol 49 (4):289–292.
Asge Standards of Practice Committee, Gurudu SR, Bruining DH, Acosta RD, Eloubeidi MA, Faulx AL, Khashab MA, Kothari S, Lightdale JR, Muthusamy VR, Yang J, DeWitt JM (2017) The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc 85 (1):22–31.
Wang Z, Chen JQ, Liu JL, Qin XG, Huang Y (2013) CT enterography in obscure gastrointestinal bleeding: a systematic review and meta-analysis. J Med Imaging Radiat Oncol 57 (3):263–273.
Law R, Varayil JE, WongKeeSong LM, Fidler J, Fletcher JG, Barlow J, Alexander J, Rajan E, Hansel S, Becker B, Larson JJ, Enders FT, Bruining DH, Coelho-Prabhu N (2017) Assessment of multi-modality evaluations of obscure gastrointestinal bleeding. World J Gastroenterol 23 (4):614–621.
Manguso N, Gangi A, Johnson J, Harit A, Nissen N, Jamil L, Lo S, Wachsman A, Hendifar A, Amersi F (2018) The role of pre-operative imaging and double balloon enteroscopy in the surgical management of small bowel neuroendocrine tumors: Is it necessary? J Surg Oncol 117 (2):207–212.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, Shih T, Yao JC (2017) Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol 3 (10):1335–1342.
Untch BR, Bonner KP, Roggin KK, Reidy-Lagunes D, Klimstra DS, Schattner MA, Fong Y, Allen PJ, D’Angelica MI, DeMatteo RP, Jarnagin WR, Kingham TP, Tang LH (2014) Pathologic grade and tumor size are associated with recurrence-free survival in patients with duodenal neuroendocrine tumors. J Gastrointest Surg 18 (3):457–462; discussion 462–453.
Hope TA, Bergsland EK, Bozkurt MF, Graham M, Heaney AP, Herrmann K, Howe JR, Kulke MH, Kunz PL, Mailman J, May L, Metz DC, Millo C, O’Dorisio S, Reidy-Lagunes DL, Soulen MC, Strosberg JR (2018) Appropriate Use Criteria for Somatostatin Receptor PET Imaging in Neuroendocrine Tumors. J Nucl Med 59 (1):66–74.
Baumann T, Rottenburger C, Nicolas G, Wild D (2016) Gastroenteropancreatic neuroendocrine tumours (GEP-NET) - Imaging and staging. Best Pract Res Clin Endocrinol Metab 30 (1):45–57.
Deroose CM, Hindie E, Kebebew E, Goichot B, Pacak K, Taieb D, Imperiale A (2016) Molecular Imaging of Gastroenteropancreatic Neuroendocrine Tumors: Current Status and Future Directions. J Nucl Med 57 (12):1949–1956.
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. McCollough and Fletcher receive grant support to their institution from Siemens Healthineers, unrelated to this work.
IRB disclaimer
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (include name of committee + reference number) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Following approval by the Institutional Review Board, Mayo Clinic Rochester patients with histologically proven SBNEN from January 1996 to February 2016 were retrospectively identified via search of our institution’s surgical pathology database. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S., Marcus, R., Wells, M.L. et al. The evolving role of imaging for small bowel neuroendocrine neoplasms: estimated impact of imaging and disease-free survival in a retrospective observational study. Abdom Radiol 45, 623–631 (2020). https://doi.org/10.1007/s00261-020-02410-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02410-z