Abstract
Purpose
To compare the reproducibility and accuracy of R2-relaxometry MRI for estimation of liver iron concentration (LIC) between in-house analysis and FDA-approved commercially available third party results.
Methods
All MR studies were performed on a 1.5T scanner. Multi-echo spin-echo scans with a fixed TR and increasing TE values of 6 ms, 9 ms, 12 ms, 15 ms, and 18 ms (spaced at 3 ms intervals) were used. Post-processing of the images to calculate mean relaxivity, R2, included drawing of regions of interest to include the whole liver on mid-slice. The relationship between liver R2 values and estimated LIC calculated with in-house analysis and values reported by an external company (FerriScan®, Resonance Health, Australia) were assessed with correlation coefficients and Bland–Altman difference plots. Continuous variables are presented as mean ± standard deviation. Significance was set at p value < 0.05.
Results
474 studies from 175 patients were included in the study (mean age 10.4 ± 4.2 years (range 1–18 years); 254 studies from girls, 220 studies from boys). LIC ranged from 0.6 to 43 mg/g dry tissue, covering a broad range from normal levels to extremely high iron levels. Linearity between proprietary and in-house methods was excellent across the observed range for R2 (31.5 to 334.8 s−1); showing a correlation coefficient of r = 0.87, p < 0.001. Bland–Altman R2 difference plot between the two methods shows a mean bias of + 21.5 s−1 (range − 47.0 to + 90.0 s−1 between two standard deviations). LIC reported by FerriScan® compared with LIC estimated in-house with R2 as reported by FerriScan® agreed strongly, (r = 1.0, p < 0.001).
Conclusion
R2 relaxometry MR imaging for liver iron concentration estimation is reproducible between proprietary FDA-approved commercial software and in-house analysis methods.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iron deposition in the liver can be secondary to serial transfusions or hereditary processes that result in abnormally increased red cell turnover or abnormal GI tract absorption of iron [1]. Iron overload in the liver has been associated with liver injury and the developing of other chronic conditions such as liver fibrosis, cirrhosis, and hepatocellular carcinoma (HCC) [2]. The measurement of liver iron concentration (LIC) has traditionally relied on liver biopsy [3, 4]. However, considering liver biopsy is an invasive procedure, it has limitations associated with high sample variability, technique-sampling errors, moderate inter-reader agreement, low acceptance from the patient, and is considered as unsuitable to be used in a consecutive routine follow-up assessment [3, 5,6,7,8,9,10,11]. Moreover, the rate of hospitalization related to liver biopsy and risk of severe complications, have been reported between 1% and 5%, respectively with reported mortality rates ranging from 1:1000 to 1:10,000 [12,13,14,15].
Magnetic resonance image (MRI) has been shown to accurately quantify liver iron content without the need for invasive biopsy, thereby allowing serial assessment that can guide iron-reducing therapies [16]. MRI has largely taken over as the diagnostic modality of choice for the identification and quantitation of LIC [17].
MRI relaxation time techniques to estimate liver iron concentration have been developed and studied for several years [18,19,20,21,22,23,24,25,26,27,28]. Iron shortens T1, T2, and T2* relaxation times measured by MRI, darkening the images [29]. The reciprocals of relaxation times, T2 and T2*, known as relaxivity, R2 and R2*, are directly proportional to iron and are commonly used [30,31,32].
The most widely adopted FDA-approved method is based on the measurement of tissue proton transverse relaxation rates (R2) and show excellent correlation with LIC measured by biopsy [33, 34]. Most investigators have described a linear rise in R2 with iron [18,19,20,21,22,23,24,25,26,27,28]; however, these studies have been criticized for their small size, limited dynamic range, and inter-study calibration variability [18, 19].
R2-MRI (FerriScan®, Resonance Health, Australia) is currently FDA-approved for estimating LIC [35]. Studies have reported sensitivity and specificity up to an LIC of 15 mg/g dry weight of 85% and 92% respectively [17]. However, to the best of our knowledge, the technical details by which FerriScan® performs their analysis have not yet been reproduced using a method on a large pediatric dataset. Our objective in this study was to assess the reproducibility and accuracy of R2-relaxometry MRI for estimation of the LIC between non-proprietary in-house analysis and a FDA-approved commercially available third party derived results in children.
Methods
Subjects
Our Institutional Review Board approved this Health Insurance Portability and Accountability Act (HIPPA) compliant retrospective study. All patients aged 0–18 years with available liver MR indicated for iron quantification using R2 sequences between February 2008 and June 2018 were initially identified. Patients with incomplete imaging data or incomplete demographics in the electronic medical record were excluded. Demographic and anthropometric measures at the time of the exam were retrieved from the electronic medical records. While the MR scanner software was updated in 2011, and in 2016, there were no changes in the liver iron quantification protocol.
MR imaging
All MRI studies were performed using a 1.5T scanner (Avanto, Siemens Healthineers, USA). Multi-echo spin-echo axial scans with a fixed repetition time (TR) of 1000 ms (msec), matrix size of 256 with typical fields of view between 300 and 400 mm (exact dimensions depending on subject size), slice thickness of 5 mm, and increasing echo time (TE) values of 6 ms, 9 ms, 12 ms, 15 ms, and 18 ms (spaced at 3 ms intervals) were acquired based on methodology previously reported by St. Pierre et al. [25, 36]. No fat suppression was used (Table 1). All commercial MR scanners can accommodate the parameters needed to acquire the images. As required in the FerriScan® protocol guidelines, a 1-l saline bag was placed along the left side of the torso as an external reference for correction of signal gain changes. The spin-echo image acquisitions were performed free-breathing without respiratory compensation techniques. Small amounts of respiratory motion artifacts from free-breathing acquisition technique are expected and acceptable. However, if severe motion artifacts are observed on the acquired images, scans need to be repeated or performed under light sedation to improve image quality.
Imaging post-processing
For analysis by an external company (FerriScan®, Resonance Health, Australia), images were securely transmitted offsite to Resonance Health for post-processing and analysis using their proprietary method, the general principles of which have been previously described [17, 25, 37]. The transverse relaxivity, R2, is calculated by exponential curve fitting to the image signal intensities obtained by the individual TE images [38]. The mean R2 value within the liver is then used to yield an estimated LIC using a calibration curve that had been determined through the measurement of liver R2 and needle biopsy LIC [25]. For the images sent offsite, image analysis for LIC values estimated by the R2 method were performed by Resonance Health for a fee per study and a report was sent back to our facility, within 48–72 h. Using the report sent back by Resonance Health, the mean R2, standard deviation, and corresponding estimated LIC were extracted for comparison and analysis.
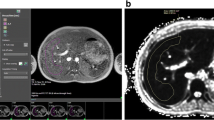
For in-house analysis, post-processing was performed using parametric MRI software (www.parametricMRI.com, Philadelphia, PA, USA) (Fig. 1). We used the individual TE images to calculate R2 maps and by drawing regions of interest (ROI) on the mid-liver slice of the generated R2 map, a mean R2 value was calculated. One ROI was placed in a transverse mid-slice section encompassing the entire visible liver boundary and avoiding any major vessels and bile ducts. Two medical doctors under the guidance of a PhD physicist with 15+ years of experience of R2 measurement performed the analysis. Studies were mutually, randomly and equally split between the two analysts. Mono-exponential T2 relaxation times were calculated for the ROIs. The mono-exponential T2 relaxation was calculated by fitting the signal intensity of each pixel using the equation:
where constant, C, was considered necessary to compensate for contributions from instrument noise and effects from iron-poor species such as blood and bile [34]. The calculated T2 relaxation time in ms was converted to relaxivity, R2, in s−1 by R2 = 1000/T2. R2 was then converted to estimated LIC as previously described [34];
T2, R2, and estimated LIC maps were generated (Fig. 2). LIC reported by FerriScan® was also compared with the LIC estimated in-house using R2 as reported by FerriScan®. The reason to do this was to estimate if the difference in values were truly due to variation in ROI selection.
Statistical analysis
The relationship between liver R2 values and LIC estimated in-house and values calculated by FerriScan® were assessed with correlation coefficients and Bland–Altman difference plots. Statistical analyses were performed with MedCalc version 18.11 (Medcalc, Ostend, Belgium). Continuous variables were presented as mean ± standard deviation (SD). Significance was set at p value < 0.05. Linear regression was used to compare the proprietary and non-proprietary values. Systematic differences between methods were tested with the Bland–Altman analysis, with limits of agreement as mean ± 1.96 multiplied by the standard deviation. Defined outliers are studies that are more than two standard deviations from the mean and discontinuous from the sample. Correlation coefficients were classified using the following definitions: less than 0.39, weak; 0.40–0.59, moderate; 0.60–0.79, strong; 0.80–0.99, excellent [39].
Results
A total of 474 studies (254 studies from girls and 220 studies from boys) from 175 patients were included in the study. 24 studies were excluded because of breathing motion artifacts (n = 6), incomplete scans (n = 7), and failed post-processing due to insufficient images (n = 11). The mean age of the patients was 10.4 ± 4.2 years (range 1–18 years). The LIC ranged from 0.6 to 43.0 mg/g dry liver, covering a broad range from close to normal levels to extremely high iron levels. The etiology of iron overload (number of studies) in the patient population was as follows: Beta thalassemia (n = 207), Sickle cell disease (n = 138), Sideroblastic anemia (n = 20), Pyruvate kinase deficiency (n = 17), Diamond-Blackfan anemia (n = 14), Hemoglobin E disease (n = 13), Hemoglobin H disease (n = 10), aplastic anemia (n = 8), Hereditary hemolytic anemia (n = 4), Idiopathic acquired aplastic anemia (n = 6), Non-autoimmune hemolytic anemia (n = 4), Acute lymphoblastic leukemia (n = 5), Glucose-6-phosphate dehydrogenase deficiency (n = 4), Hemochromatosis (n = 3), Alpha thalassemia (n = 2), Aplastic anemia (n = 2), Autoimmune hemolytic anemia (n = 2), Wilms tumor(n = 2), 1 study each with SAMD9 gene mutation, Langerhan’s cell histiocytosis, Hemolytic anemia of unknown origin, Erwings sarcoma, and Chronic Dyserythropoietic Anemia, and 8 studies for other oncology follow-up reasons.
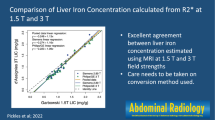
Linearity between proprietary and non-proprietary in-house method for R2 was excellent across the observed range for R2 (31.5 to 334.8 s−1). We obtained a correlation coefficient r = 0.87, p < 0.001 for R2 (Table 2; Fig. 3). A Bland–Altman R2 difference plot between the two methods shows a mean bias of + 21.5 s−1 (range − 47.0 to + 90.0 s−1) between two standard deviations (Fig. 4). Similarly, linearity between proprietary and non-proprietary in-house methods for estimated LIC was also observed to be excellent across the observed range for LIC (0.6 to 43 mg/gm). We obtained a correlation coefficient r = 0.84, p < 0.001 for LIC (Fig. 5). The Bland–Altman LIC difference plot between the two methods show a mean bias of + 2.9 mg/gm (range − 8.9 to + 14.7 mg/gm) between two standard deviations (Fig. 6). Representative images of comparison between the two methods performed on two representative subjects, one with a history of Beta thalassemia (Fig. 7) and the other with Diamond-Blackfan anemia (Fig. 8) are shown. Excellent agreement was observed on LIC reported by FerriScan® compared with LIC estimated in-house using R2 reported by FerriScan®, r = 1.0, p < 0.001 (Fig. 9).
Representative images from a 4-year-old boy with a history of Beta thalassemia. Report by Ferriscan® shows a mean R2 of 91.5 ± 14.2 s−1 corresponding to an estimated LIC of 5.4 mg/g. Performing analysis in-house, we measured a mean T2 of 8.9 ms; translating to a R2 of 98.5 ± 5.2 s−1 and an estimated LIC of 6.5 mg/g. a Signal intensity vs echo time with varying degrees of liver signal are shown. b Proprietary versus generated in-house by non-proprietary analysis R2 map; c generated in-house by non-proprietary analysis, its corresponding T2 map and d LIC map
Representative images from a 5-year-old boy with history of Diamond-Blackfan anemia. Report by Ferriscan® shows a mean R2 of 241 ± 27.9 s−1 corresponding to an estimated LIC of 30.1 mg/g. Performing analysis in-house, we measured a mean T2 of 4.7 ms; translating to a R2 of 280.8 ± 30.4 s−1 and an estimated LIC of 41.1 mg/g. a Signal intensity vs echo time with varying degrees of liver signal are shown. b Proprietary vs generated in-house by non-proprietary analysis R2 map; c generated in-house by non-proprietary analysis, its corresponding T2 map and d LIC map
Discussion
Non-invasive assessment of LIC is universally accepted as an alternative to biopsy and serves as a reliable technique for clinicians to assess evidence-based management of iron overload. In particular, R2 based analysis is currently only available through a commercial off-shore data processing center using a proprietary method (Ferriscan®, Resonance Health, Australia), limiting its clinical and research applications. We investigated the inter-method reproducibility between proprietary and in-house curve fitting methods. We found that values for R2 relaxometry MRI for LIC estimation is reproducible between FDA-approved commercially available and our in-house analysis methods, and it shows excellent agreement. To the best of our knowledge, there are no previous studies that have reported a comparison between two different methods to determine LIC in a pediatric population with a wide range of iron content in a large number of studies.
Our results for R2 values show strong agreement between proprietary and in-house developed non-proprietary methods (r = 0.86, p < 0.001). The Bland–Altman difference plot between the two methods shows a R2 mean bias of + 21.5 s−1 or a LIC mean bias of + 3.0 mg/gm. This in our opinion is unlikely to be clinically meaningful. Our results are within range of a previously reported inter-method agreement of ± 9% performed on a smaller sample of 40 studies in adults [40]. Our results also show that the difference in the values of LIC estimated by the two methods is likely only due to user-dependent ROIs and not in the conversion from R2 to LIC. Using R2 values reported by Ferriscan®, and estimating LIC in-house using the previously reported formula [30, 34], we observe excellent agreement in estimated LIC (r = 1.0, p < 0.001) with the Bland–Altman difference plot between the comparison showing a mean bias of only − 0.37 mg/g (range − 0.74 to + 0.01 mg/g). The purpose of our study was to compare MRI derived R2 and its estimated LIC between two methods using formulae in scientific published literature. We did not intend to or attempt to reverse engineer proprietary analysis methods. Availability of in-house analysis can facilitate further development and research of acquisition and analysis methods by independent academic investigators. Potential research areas may include inclusion of fat suppression, motion suppression techniques such as non-cartesian k-space acquisitions, and acquisition speed improvement such as echo train acquisitions and compressed sensing. Advanced analysis methods may include development of machine learning and deep learning algorithms.
One limitation of this study is that all available R2 MR images for LIC assessment were acquired at a single institution. Future work will require that we correlate our results with multi-centered studies. Second limitation is that although the images are acquired in free-breathing and small amounts of motion artifacts are expected, for severe motion, the images are repeated or performed under light sedation. Within the scope of this work and due to the retrospective nature of the study, we did not track the need to repeat scans or sedation records. Finally, the LIC range of the population included in our study was from 0.6 mg/g to upper range of estimated LIC of 43 mg/g is due to the inherent limitation of the current MRI protocol used for the R2 mapping method (Fig. 10). If needed, UTE based acquisition protocol may be used to increase the dynamic range.
Conclusion
In conclusion, R2 based relaxometry MR imaging for liver iron concentration estimation is a robust and reliable method that is reproducible between FDA-approved commercially available and our in-house analysis methods.
References
Lieu PT, Heiskala M Fau - Peterson PA, Peterson Pa Fau - Yang Y, Yang Y. The roles of iron in health and disease. (0098-2997 (Print)).
Ware HM, Kwiatkowski JL. Evaluation and treatment of transfusional iron overload in children. Pediatric clinics of North America. 2013;60(6):1393-406.
Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. The American journal of gastroenterology. 2002;97(10):2614-8.
Beilby JP, Prins AW, Swanson NR. Determination of hepatic iron concentration in fresh and paraffin-embedded tissue. Clin Chem. 1999;45(4):573-4.
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver biopsy. Hepatology (Baltimore, Md). 2009;49(3):1017-44.
Cunha GM, Glaser KJ, Bergman A, Luz RP, de Figueiredo EH, Lobo Lopes FPP. Feasibility and agreement of stiffness measurements using gradient-echo and spin-echo MR elastography sequences in unselected patients undergoing liver MRI. The British journal of radiology. 2018;91(1087):20180126.
German AL, Fleming K, Kaye P, Davies S, Goldin R, Hubscher SG, et al. Can reference images improve interobserver agreement in reporting liver fibrosis? Journal of clinical pathology. 2018;71(4):368-71.
Jung ES, Lee K, Yu E, Kang YK, Cho MY, Kim JM, et al. Interobserver Agreement on Pathologic Features of Liver Biopsy Tissue in Patients with Nonalcoholic Fatty Liver Disease. Journal of pathology and translational medicine. 2016;50(3):190-6.
Pournik O, Alavian SM, Ghalichi L, Seifizarei B, Mehrnoush L, Aslani A, et al. Inter-observer and Intra-observer Agreement in Pathological Evaluation of Non-alcoholic Fatty Liver Disease Suspected Liver Biopsies. Hepatitis monthly. 2014;14(1):e15167.
Ratziu V, Bonyhay L, Di Martino V, Charlotte F, Cavallaro L, Sayegh-Tainturier MH, et al. Survival, liver failure, and hepatocellular carcinoma in obesity-related cryptogenic cirrhosis. Hepatology (Baltimore, Md). 2002;35(6):1485-93.
Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology (Baltimore, Md). 2003;38(6):1449-57.
Cadranel JF, Rufat P, Degos F. Practices of liver biopsy in France: results of a prospective nationwide survey. For the Group of Epidemiology of the French Association for the Study of the Liver (AFEF). Hepatology (Baltimore, Md). 2000;32(3):477-81.
Froehlich F, Lamy O, Fried M, Gonvers JJ. Practice and complications of liver biopsy. Results of a nationwide survey in Switzerland. Dig Dis Sci. 1993;38(8):1480-4.
Perrault J, McGill DB, Ott BJ, Taylor WF. Liver biopsy: complications in 1000 inpatients and outpatients. Gastroenterology. 1978;74(1):103-6.
Bravo AA, Sheth SG, Chopra S. Liver biopsy. N Engl J Med. 2001;344(7):495-500.
Verlhac S, Morel M, Bernaudin F, Bechet S, Jung C, Vasile M. Liver iron overload assessment by MRI R2* relaxometry in highly transfused pediatric patients: an agreement and reproducibility study. Diagnostic and interventional imaging. 2015;96(3):259-64.
St Pierre TG, Clark PR, Chua-Anusorn W. Measurement and mapping of liver iron concentrations using magnetic resonance imaging. Annals of the New York Academy of Sciences. 2005;1054:379-85.
Angelucci E, Giovagnoni A, Valeri G, Paci E, Ripalti M, Muretto P, et al. Limitations of magnetic resonance imaging in measurement of hepatic iron. Blood. 1997;90(12):4736-42.
Brittenham GM, Badman DG. Noninvasive measurement of iron: report of an NIDDK workshop. Blood. 2003;101(1):15-9.
Dixon RM, Styles P, al-Refaie FN, Kemp GJ, Donohue SM, Wonke B, et al. Assessment of hepatic iron overload in thalassemic patients by magnetic resonance spectroscopy. Hepatology (Baltimore, Md). 1994;19(4):904-10.
Engelhardt R, Langkowski JH, Fischer R, Nielsen P, Kooijman H, Heinrich HC, et al. Liver iron quantification: studies in aqueous iron solutions, iron overloaded rats, and patients with hereditary hemochromatosis. Magn Reson Imaging. 1994;12(7):999-1007.
Kaltwasser JP, Gottschalk R, Schalk KP, Hartl W. Non-invasive quantitation of liver iron-overload by magnetic resonance imaging. Br J Haematol. 1990;74(3):360-3.
Mavrogeni SI, Gotsis ED, Markussis V, Tsekos N, Politis C, Vretou E, et al. T2 relaxation time study of iron overload in b-thalassemia. Magma (New York, NY). 1998;6(1):7-12.
Papakonstantinou O, Kostaridou S, Maris T, Gouliamos A, Premetis E, Kouloulias V, et al. Quantification of liver iron overload by T2 quantitative magnetic resonance imaging in thalassemia: impact of chronic hepatitis C on measurements. Journal of pediatric hematology/oncology. 1999;21(2):142-8.
St Pierre TG, Clark PR, Chua-anusorn W, Fleming AJ, Jeffrey GP, Olynyk JK, et al. Noninvasive measurement and imaging of liver iron concentrations using proton magnetic resonance. Blood. 2005;105(2):855-61.
Stark DD, Bass NM, Moss AA, Bacon BR, McKerrow JH, Cann CE, et al. Nuclear magnetic resonance imaging of experimentally induced liver disease. Radiology. 1983;148(3):743-51.
Voskaridou E, Douskou M, Terpos E, Papassotiriou I, Stamoulakatou A, Ourailidis A, et al. Magnetic resonance imaging in the evaluation of iron overload in patients with beta thalassaemia and sickle cell disease. Br J Haematol. 2004;126(5):736-42.
Wang ZJ, Haselgrove JC, Martin MB, Hubbard AM, Li S, Loomes K, et al. Evaluation of iron overload by single voxel MRS measurement of liver T2. J Magn Reson Imaging. 2002;15(4):395-400.
Sirlin CB, Reeder SB. Magnetic resonance imaging quantification of liver iron. Magnetic resonance imaging clinics of North America. 2010;18(3):359-81, ix.
Serai SD, Fleck RJ, Quinn CT, Zhang B, Podberesky DJ. Retrospective comparison of gradient recalled echo R2* and spin-echo R2 magnetic resonance analysis methods for estimating liver iron content in children and adolescents. Pediatric radiology. 2015;45(11):1629-34.
Serai SD, Trout AT, Fleck RJ, Quinn CT, Dillman JR. Measuring liver T2* and cardiac T2* in a single acquisition. Abdom Radiol (NY). 2018.
Towbin AJ, Serai SD, Podberesky DJ. Magnetic resonance imaging of the pediatric liver: imaging of steatosis, iron deposition, and fibrosis. Magn Reson Imaging Clin N Am. 2013;21(4):669-80.
Hankins JS, McCarville MB, Loeffler RB, Smeltzer MP, Onciu M, Hoffer FA, et al. R2* magnetic resonance imaging of the liver in patients with iron overload. Blood. 2009;113(20):4853-5.
Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, et al. MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood. 2005;106(4):1460-5.
Wood JC, Pressel S, Rogers ZR, Odame I, Kwiatkowski JL, Lee MT, et al. Liver iron concentration measurements by MRI in chronically transfused children with sickle cell anemia: baseline results from the TWiTCH trial. Am J Hematol. 2015;90(9):806-10.
St Pierre TG, El-Beshlawy A, Elalfy M, Al Jefri A, Al Zir K, Daar S, et al. Multicenter validation of spin-density projection-assisted R2-MRI for the noninvasive measurement of liver iron concentration. Magn Reson Med. 2014;71(6):2215-23.
Clark PR, Chua-Anusorn W, St Pierre TG. Proton transverse relaxation rate (R2) images of liver tissue; mapping local tissue iron concentrations with MRI [corrected]. Magnetic resonance in medicine. 2003;49(3):572-5.
Clark PR, St Pierre TG. Quantitative mapping of transverse relaxivity (1/T(2)) in hepatic iron overload: a single spin-echo imaging methodology. Magnetic resonance imaging. 2000;18(4):431-8.
Hallgren KA. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutorials in quantitative methods for psychology. 2012;8(1):23-34.
Pirasteh A, Yuan Q, Hernando D, Reeder SB, Pedrosa I, Yokoo T. Inter-method reproducibility of biexponential R2 MR relaxometry for estimation of liver iron concentration. Magnetic resonance in medicine. 2018;80(6):2691-701.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calle-Toro, J.S., Barrera, C.A., Khrichenko, D. et al. R2 relaxometry based MR imaging for estimation of liver iron content: A comparison between two methods. Abdom Radiol 44, 3058–3068 (2019). https://doi.org/10.1007/s00261-019-02074-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02074-4