Abstract
Objective
To review the incidence of significant bleeding complications after ultrasound-guided percutaneous core native renal biopsies at a single center using a standardized technique.
Materials and methods
A retrospective review of ultrasound (US)-guided percutaneous native renal core biopsies done at our institution from September 2005 to December 2015 was performed. Demographic and clinical data were collected at the time of biopsy, with additional clinical information recorded 24 h and 3 months after the biopsy. Bleeding complications were defined using the Common Terminology Criteria for Adverse Events (CTCAE, version 4.0) created by the National Institutes of Health.
Results
2204 US-guided native renal core biopsies were performed during the study period, with 37 hemorrhages (1.64%) that were CTCAE grade 3 or higher. The rate of inadequate sampling as reported by pathology was extremely low (1.1%). Factors demonstrating a significant association with bleeding risk included estimated glomerular filtration rate (eGFR), specifically when the eGFR was less than 60 (p = 0.025), platelet count (p = 0.002), including a statistically significant decreased risk of bleeding with a platelet count greater than 100 (109/L) (p = <0.001), and performing four or more needle passes (p = 0.012). While female gender was also associated with an increased bleeding risk (p = 0.05), there was a significant association between females with a BMI ≥ 25 and a decreased bleeding risk (0.034). No statistically significant association between post-biopsy hemorrhage and aspirin use within 10 days prior to biopsy or a prior diagnosis of amyloidosis was demonstrated.
Conclusion
US-guided native renal biopsy is a safe procedure with a low rate of significant bleeding complications and a high tissue adequacy rate using an 18-gage spring-loaded biopsy device. Factors associated with increased bleeding risk include female gender, lower platelet counts, decreased eGFR and performing four or more needle passes, which has not been reported previously. Interestingly, females with a BMI ≥ to 25 demonstrated a decreased bleeding risk, and aspirin (81 mg or 325 mg) within 10 days of the procedure did not demonstrate a significant effect. While not shown in this current study, the relationship of very recent aspirin therapy with bleeding is yet to be defined. Similarly, the statistically significant decreased risk of bleeding complications in overweight or obese females requires further investigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous image-guided native renal biopsy is an important diagnostic tool in the work-up of renal parenchymal disease [1]. While advancements in imaging and biopsy instruments have improved procedure safety, acquiring tissue remains an invasive procedure, with risks including pain, bleeding, infection, or even death [2].
The most common complication of renal biopsy is hemorrhage, which is likely the result of multiple factors including the innate vascularity and non-compressible location of the kidney, the need for multiple needle passes to ensure an adequate tissue sample, and patient comorbidities such as obesity, liver dysfunction, and diabetes [3]. Post-biopsy bleeding can be further categorized into major and minor complications, with major complications requiring treatments such as blood transfusion, endovascular intervention, or nephrectomy. The incidence of major complications varies throughout literature, with reports ranging from 0.1 to 7.4% [4].
Certain risk factors have been associated with an increased risk of post-biopsy hemorrhage, including patient gender, age, serum creatinine, bleeding diathesis, hypertension, biopsy needle size, and number of needle passes [2, 5,6,7]. While bleeding risk associated with an underlying histologic diagnosis such as amyloidosis has been studied previously, the largest single-institution study was limited to 101 patients [8]. Similarly, significant obesity related risk has yet to be elucidated. The purpose of this study was to retrospectively evaluate the incidence of major bleeding complications following image-guided native renal biopsy at a single institution, and identify factors that may be associated with such post-biopsy hemorrhage.
Methods
Patient population
Approval for this HIPAA-compliant retrospective study was obtained from our institutional review board (IRB). Informed consent was waived by the IRB.
Using an internal, prospectively maintained departmental biopsy database, subjects who had undergone a native renal parenchymal biopsy under computed tomographic (CT) or ultrasound (US) guidance between September 1, 2005 and December 29, 2015 were identified. Subjects who received multiple biopsies on the same day (N = 3 subjects, 6 biopsies), subjects who did not grant research authorization approval (N = 106, 4.3%), and those who were under 18 (N = 84) were excluded. The primary outcome of interest was the presence of a bleeding complication (CTCAE grade 3 or higher) within 3 months post-biopsy. Biopsies where the primary outcome was unknown were also excluded (N = 16), where the imaging methodology was atypical for this practice (CT vs US, N = 36), and those where a needle size other than 18 gage was used (N = 12) were also excluded, leaving a total of 2204 biopsies.
Procedural details
For each procedure, written informed consent was obtained. Local anesthesia was provided with 1% lidocaine. Moderate sedation with fentanyl and midazolam was used in some cases (N = 373, 16.9%). Ultrasound-guided biopsies were performed without an introducer, most often using an 18-gage Bard Monopty Device (Bard Biopsy Systems, Tempe, AZ). Each kidney sample was evaluated immediately following retrieval for adequate glomeruli with light microscopy by a trained radiology nurse, procedural assistant, or radiologist. Onsite sample evaluation by a nephrologist or pathologist was not routinely performed. Per protocol, two adequate core samples were obtained during the biopsy procedure.
Immediately following biopsy, the kidney was imaged with the respective imaging modality to assess for hemorrhage. Patients with developing hematomas were observed in the procedural suite. If additional findings such as hemodynamic instability or significant pain were present, urgent CT imaging was obtained to better assess the extent of bleeding with frequent referral for angiography and potential embolization. Following stabilization, these patients were admitted to the hospital for further management. The remaining patients without such hematomas were observed for 6 h prior to dismissal. Neither routine follow-up imaging nor blood work was performed in these patients.
At the time of biopsy, patients were asked to provide a telephone number so a dedicated radiology registered nurse could contact them post-procedurally to inquire about possible complications. Telephone follow-up was attempted on post-procedural day 1, and if contact was unsuccessful, again on days 2 and 3. A standardized questionnaire was administered to the patient and any patients reporting worrisome symptoms such as significant pain, lightheadedness, or marked hematuria were advised to report to the closest emergency department. In addition to this direct post-procedure communication, a simultaneous review of the electronic medical record was performed. A second nursing review of the medical record was performed 3 months post-procedure to capture any significant complications occurring during this time, i.e., subsequent hospital admissions related to angiography, transfusions, hematuria, or pain control. Post-biopsy bleeding complications were defined using the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0, created by the National Institutes of Health [9]. A major adverse bleeding event was characterized by meeting or exceeding a grade 3 complication, which includes the need for hospitalization, transfusion, interventional radiology procedure, or an operative intervention.
Additional information extracted from the database included patient characteristics (gender, age, BMI), specific laboratory data [platelet concentration, creatinine, estimated glomerular filtration rate (eGFR)], aspirin use (both 81 and 325 mg doses), biopsy needle gage, number of needle passes, and tissue sample adequacy (based on the final pathology report).
Potential risk factors of interest included age, gender, BMI, blood pressure [systolic (SBP) and diastolic (DBP) separately], platelet count, blood urea nitrogen (BUN), creatinine, eGFR (calculated using the MDRD equation), whether the procedure was performed by staff or trainee, previous diagnosis of amyloidosis based on chart review, aspirin use (either 81 mg or 325 mg) within 10 days prior to biopsy, imaging type used during procedure (US or CT), and number of needle passes (cores samples) taken during the procedure.
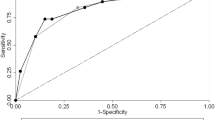
Statistical analysis
Simple descriptive statistics were calculated for each biopsy and described as counts and percentages for categorical variables and medians with 25th and 75th percentiles for continuous variables. To test for risk factors’ associations with bleeding complications, generalized estimating equations logistic regression models were used (Hardin and Hilbe, 2003; Liang and Zeger, 1986); generalized estimating equations are an extension of generalized linear models which account for correlated measurements within individuals. Due to multicollinearity among creatinine, BUN, and eGFR values, only one was included in the multivariable modeling; eGFR was selected as it had the fewest missing values. Subset analyses were performed within gender. These analyses used logistic regression, and Firth’s method was used to address the cases where quasi-complete separation was observed. Due to the small number of bleeds within each subset, only univariable models were fit for these subsets.
All tests were 2-tailed with statistical significance defined as P < 0.05. Statistical analyses were performed using SAS (version 9.3; Cary, NC).
Results
The final cohort included 2204 US-guided native renal biopsies in 2130 unique patients. The overall bleeding complication rate (CTCAE grade 3 or higher) was 1.64% (Table 1), with most complications occurring within 24 h of biopsy (N = 33/37; 89.2%). Of the patients with significant bleeding complications (N = 37), all were hospitalized. Table 2 categorizes the reason for admission; 37.8% of admitted patients underwent renal artery angiogram (N = 14), with 50.0% of those requiring concurrent embolization (N = 7). Additionally, 21 of the 37 patients required at least one blood transfusion. Only 1.1% (N= 24/2204) of tissue samples submitted to pathology were deemed inadequate for diagnosis (Table 3).
Demographic, clinical, and procedural characteristics are shown in Table 4. Descriptive statistics are presented as median and interquartile range (IQR) or counts and percentages. Due to skewness, creatinine and platelet counts were natural log (ln)-transformed prior to model inclusion; however, untransformed values are presented in the table to aid in interpretability. Our practice typically uses a threshold platelet count of 50 (109/L) and given the small number of biopsies performed below this threshold (N = 7/1998, 0.4%) and the absence of any significant post-biopsy bleeding events in this category, a platelet threshold of 100 (109/L) was chosen to construct a dichotomous platelet count model.
Unadjusted and adjusted GEE models are shown in Tables 5, 6, 7. Based on previous literature, all multivariable models were adjusted for age and gender. In the final multivariable model, four or more passes taken [OR 2.97 (95% CI 1.26–7), p = 0.012], eGFR < 60 [OR 9.43 (95% CI 1.32–67.2), p = 0.025], and female gender [OR 5.14 (95% CI 1.47–18), p = 0.05] were associated with increased risk of bleeding. Increased platelet count was associated with decreased risk of bleeding [OR 0.341 (95% CI 0.172–0.678), p = 0.002] and there was a significant interaction between gender and BMI, with females with high BMI (≥ 25) showing a significant decrease in bleeding risk [OR 0.183 (95% CI 0.0382–0.878), p = 0.034], whereas males with high BMI showed a non-significant increase in bleeding risk (OR 1.24 (95% CI 0.343–4.49), p = 0.13], after adjustment for eGFR, platelet count, age, gender, and number of passes taken.
Among subjects who had blood pressure data available (N = 584), there were 7 complications observed. Although there was a higher incidence of bleeding complications among hypertensive subjects (hypertensive 5/219, 2.28% vs. non-hypertensive 2/365, 0.54%), statistical significance could not be concluded due to the low number of events.
Discussion
Native renal biopsy is an important tool for accurate diagnosis and treatment of renal parenchymal disease; however, they are not without risk. A recent meta-analysis performed by Corapi et al. in 2015 [6] reviewed 34 studies regarding complications of native kidney biopsies, with the largest single-center study by Mackinnon et al. comprising 1,120 patients. Therefore, this retrospective review is the largest known single-institution study evaluating risks associated with significant hemorrhage, with rates similar to those previously reported 0.1–7.4% [4]. Likewise, multiple studies have evaluated the diagnostic adequacy of percutaneous native renal biopsy comparing different sized needles, with several reporting an inferior yield with 18 gage needles [10, 16]. This study evaluated biopsies using 18 gage spring-loaded devices exclusively, with only a 1.1% rate of sample inadequacy.
One patient factor significantly associated with bleeding complications was female gender (p = 0.05). This has been described previously, with hypotheses including smaller kidney size compared to men, resulting in deeper needle penetration into the renal medulla [5, 6, 11]. In our final model, however, females with a BMI ≥ to 25 demonstrated a statistically significant decrease in major bleeding complications (OR 0.183, p = 0.034). This would seem counterintuitive, as obesity has been shown to be an increased risk factor in multiple studies [4, 12] likely secondary to poor sonographic visualization, longer needle path, and inadequate patient positioning due to discomfort or associated respiratory difficulties. Interestingly, a more recent publication by Lees et al. retrospectively reviewed 1045 ultrasound-guided native renal biopsies with available BMI data and demonstrated declining rates of complications with increasing BMI, nearing statistical significance [13]. This study would support those findings that, at least in female patients, obesity may be associated with a decreased bleeding risk, although this requires further investigation.
Laboratory markers significantly associated with increased risk of bleeding complications included lower platelet concentrations and low estimated glomerular filtration rates. Specifically, for every 10 unit increase in eGFR or a platelet count greater than 100 (109/L), a statistically significant reduction of bleeding risk was observed. Both observations have been well reported in literature [6, 7, 14, 15], and currently our practice uses a platelet threshold of 50 (109/L). The single technical factor associated with an increase bleeding risk was four or more needle passes, which contradicts prior analyses [5, 6, 16] but is intuitive as each pass requires traumatic entry through the renal capsule into the parenchyma.
The use of aspirin (81 mg or 325 mg) within 10 days of native renal biopsy procedure was not statistically significant, which is consistent with current literature [17, 18]. Further study regarding specific duration of abstinence is needed to determine if a window of risk exists. Specifically, there may be a 3–4 day period following aspirin cessation where risk is elevated [18, 19]. Such information will be particularly valuable given additional impact of uremia on platelet function.
Historically, amyloidosis had been associated with increased bleeding risk secondary to vascular fragility [12, 20]. However, the subset of patients with a prior diagnosis of amyloidosis in the current study did not demonstrate an increased risk of post-biopsy hemorrhage in either the unadjusted or adjusted models. Soares et al. published results in 2008 which also failed to demonstrate an increased bleeding risk following renal biopsy in 101 patients with amyloidosis [8], and our current study adds to this with 471 patients with such disease.
One aim of the current study was to determine if there was a significant association between hypertension and bleeding risk. Unfortunately, of the 584 subjects with peri-procedural blood pressure recordings, there were only 7 complications observed and due to this low incidence, a significant association could not be established. It will be important to study potential associations between elevated blood pressure and native renal biopsies if they exist, as there is contradicting evidence in literature [5, 7, 12, 21]. In general, our practice typically suspends biopsies if patients present with a systolic blood pressure greater than 160 or a diastolic blood pressure greater than 100.
There are several limitations to this study, which include retrospective design and associated potential biases. Post-biopsy complications grade 3 or higher were considered a major adverse event, which excludes potentially clinically important complications such as outpatient management of significant hematuria requiring bladder catheterization. The overall low number of complications limited the potential statistical models that could be adequately fit to the data. Similarly, the presence of peri-procedural hypertension is a potential cofounder as it was unable to be included in the regression model due to a high number of missing values (> 75%).
Conclusion
In conclusion, US-guided renal parenchymal biopsy is a safe procedure with a low risk of major post-biopsy hemorrhage and a high sample adequacy rate. Factors associated with increased risk of significant hemorrhage included lower platelet count, declining renal function, and, contrary to prior analyses, obtaining four or more biopsy samples. Female gender was associated with an increased bleeding risk, although interestingly, females with a BMI ≥ to 25 demonstrated a statistically significant decrease in bleeding risk. The identification of such important risk factors will be helpful in mitigating future procedural risks and patient education, as well as potential avenues of future research.
References
Richards, N.T., et al., Knowledge of renal histology alters patient management in over 40% of cases. Nephrol Dial Transplant, 1994. 9(9): p. 1255-9.
Zhu, M.S., J.Z. Chen, and A.P. Xu, Factors that can minimize bleeding complications after renal biopsy, in Int Urol Nephrol. 2014. p. 1969-75.
McWilliams, J.P. and S.T. Kee, Native Renal Biopsy: The Perfect Storm. Journal of Vascular and Interventional Radiology, 2015. 26(2): p. 212-213.
Brachemi, S. and G. Bollée, Renal biopsy practice: What is the gold standard? World J Nephrol, 2014. 3(4): p. 287-94.
Manno, C., et al., Predictors of bleeding complications in percutaneous ultrasound-guided renal biopsy. Kidney Int, 2004. 66(4): p. 1570-7.
Corapi, K.M., et al., Bleeding complications of native kidney biopsy: a systematic review and meta-analysis. Am J Kidney Dis, 2012. 60(1): p. 62-73.
Shidham, G.B., et al., Clinical risk factors associated with bleeding after native kidney biopsy. Nephrology (Carlton), 2005. 10(3): p. 305-10.
Soares, S.M., et al., Bleeding Complications After Transcutaneous Kidney Biopsy in Patients With Systemic Amyloidosis: Single-Center Experience in 101 Patients. American Journal of Kidney Diseases, 2008. 52(6): p. 1079-1083.
US Department of Health and Human Services. National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0. US Department of Health and Human Services. National Institutes of Health. National Cancer Institute (2009).
Mai, Jun et al. Is bigger better? A retrospective analysis of native renal biopsies with 16 gauge versus 18 gauge automatic needles. Nephrology. 2013. 18(7).
Peters B, Andersson Y, Stegmayr B, et al. (2014) A study of clinical complications and risk factors in 1001 native and transplant kidney biopsies in Sweden. Acta Radiol 55:890–896
Eiro, M., T. Katoh, and T. Watanabe, Risk factors for bleeding complications in percutaneous renal biopsy. Clin Exp Nephrol, 2005. 9(1): p. 40-5.
Lees, Jennifer S et al. Risk factors for bleeding complications after nephrologist-performed native renal biopsy. Clinical kidney journal vol. 10,4 (2017): 573-577.
Slichter, S.J., Relationship between platelet count and bleeding risk in thrombocytopenic patients. Transfusion Medicine Reviews, 2004. 18(3): p. 153-167.
Stratta, P., et al., Risk management of renal biopsy: 1387 cases over 30 years in a single centre. European Journal of Clinical Investigation, 2017. 37(12): p. 954-963.
Hogan Jonathan J et al. The Native Kidney Biopsy: Update and Evidence for Best Practice. Clinical journal of the American Society of Nephrology : CJASNvol. 11,2 (2015): 354-62.
Atwell, T.D., et al., Incidence of Bleeding After 15,181 Percutaneous Biopsies and the Role of Aspirin. American Journal of Roentgenology, 2010. 194(3): p. 784-789.
Baffour, F.I., et al., Effects of Aspirin Therapy on Ultrasound–Guided Renal Allograft Biopsy Bleeding Complications. Journal of Vascular and Interventional Radiology, 2017. 28(2): p. 188-194.
Jimenez, A. H., et al. Rapidity and duration of platelet suppression by enteric-coated aspirin in healthy young men. American Journal of Cardiology 69(3): 258-262.
Yood, R.A., et al., Bleeding manifestations in 100 patients with amyloidosis. JAMA, 1983. 249(10): p. 1322-1324.
Potretzke, T.A., et al., Incidence of bleeding complications after percutaneous core needle biopsy in hypertensive patients and comparison to normotensive patients. Abdominal Radiology, 2016. 41(4): p. 637-642.
Acknowledgements
The authors acknowledge the assistance of Sonia Watson, PhD, in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Monahan, H., Gunderson, T., Greene, E. et al. Risk factors associated with significant bleeding events after ultrasound-guided percutaneous native renal biopsies: a review of 2204 cases. Abdom Radiol 44, 2316–2322 (2019). https://doi.org/10.1007/s00261-019-01962-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-01962-z